User login
The liability climate for Kentucky physicians has long been bleak, according to Bruce A. Scott, MD, president of the Kentucky Medical Association. Insurance premiums are high, few doctors want to relocate to the Bluegrass State, and an overriding fear of lawsuits weighs heavily on the minds of physicians practicing there.
So the physician community was encouraged when in 2017, Kentucky enacted a law requiring all new malpractice claims to go before a medical review panel. The panel, comprised of an attorney and three health care professionals, would review evidence and opine on whether defendants had breached the standard of care. Plaintiffs could then decide whether to drop or resolve the case, or whether to continue to court.
“We saw it as a modest step forward,” Dr. Scott said in an interview. “[The panel] was hopefully going to speed up justice. Those cases that had merit would be settled, and those cases that didn’t have merit would be eliminated to allow the trial court to move on to the cases that needed to be tried.”
The Kentucky Supreme Court disagreed. In November 2018, state justices struck down the panel law as unconstitutional. Requiring plaintiffs to go before a medical review panel delays access to the courts and impedes their right to a speedy trial, the court ruled.
The end to Kentucky’s short-lived medical review panel raises questions about whether such advisory committees are beneficial in medical liability cases. Do review panels help reduce frivolous claims? What effects do the panels have on case duration and court costs?
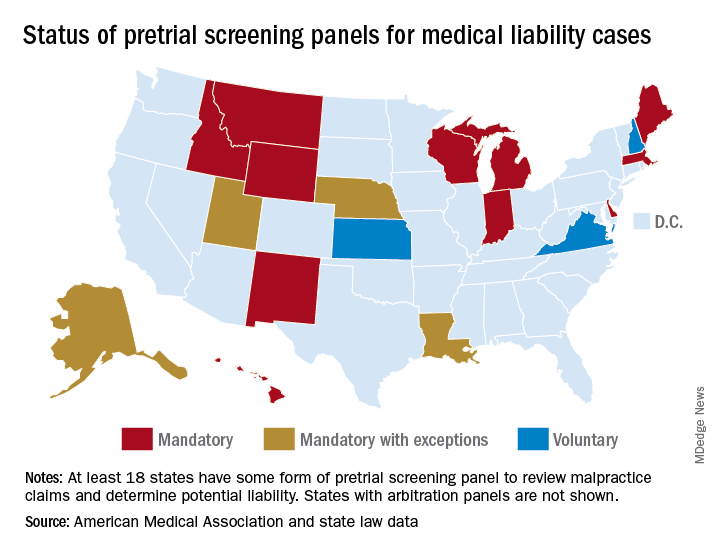
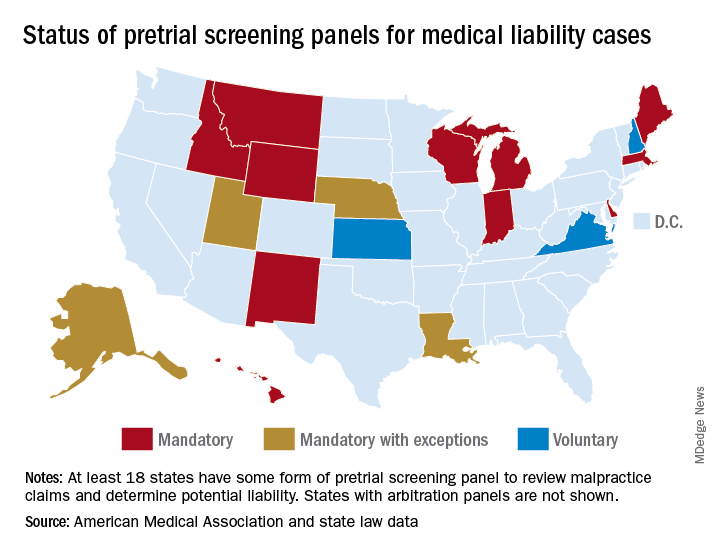
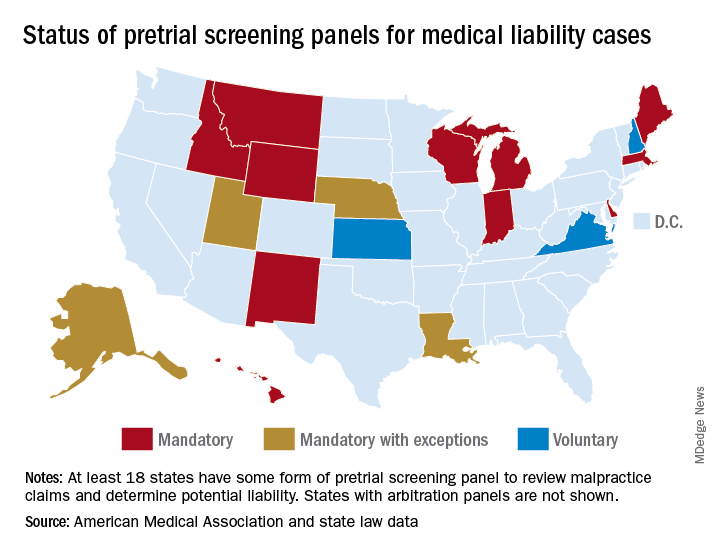
At least 17 states have some form of pretrial screening panel that evaluates claims against health care professionals. Most panels include legal experts and medical professionals who review evidence and make a determination about potential negligence. In some states, such as Indiana, a panel review is mandatory, whereas in others, like Kansas, the process is voluntary.* Most panel decisions are nonbinding, and parties can proceed to court if they prefer.
Maine: A success story
Maine has experienced marked success with its medical review panel, which has been active since 1986, said Andrew B. MacLean, an attorney and interim CEO for the Maine Medical Association (MMA). The three-person panel, which includes a judicial expert, an attorney, and a physician, addresses whether the defendant’s actions constitute a deviation from the standard of care, whether acts or omissions caused the alleged injury, and the degree to which potential negligence exists on the part of the health care professional and/or the patient.
“The vast majority of medical malpractice claims in Maine are resolved at or before the screening panel stage and our state’s relatively small medical malpractice bar has come to accept this and to work cooperatively within the panel process,” Mr. MacLean said in an interview. “This has not been easy, but we’ve achieved such a result through many years of negotiation among representatives of the judiciary, plaintiffs’ and defense bar, professional liability insurers, and the professional organizations of trial lawyers and physicians.”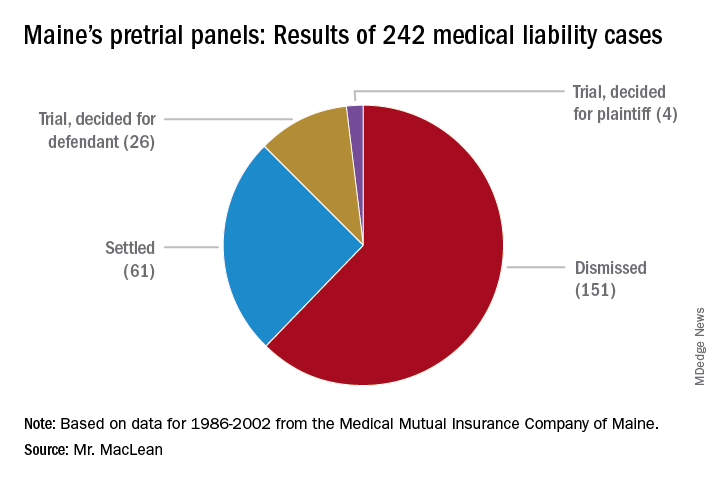
From 1986 to 2002, pretrial panels in Maine analyzed 242 medical liability cases, according to MMA data. Panelists found unanimously for the defendant in 157 cases and unanimously for the plaintiff in 42. In 43 cases, panelists were split. Of the total 242 cases, 151 were ultimately dismissed, 61 cases were settled, and 30 cases went to trial. Of the 30 cases that went to trial, jurors found for the health care professional 26 times.
A medical panel review is a quicker way to determine liability, and the process generally benefits both parties, said Peter Michaud, MMA associate general counsel. Panel hearings last 1-2 days, whereas court trial can take weeks, said Mr. Michaud, who chaired Maine’s panel for 10 years. At the same time, the patient gets their “day in court” and a chance to share their side of the story, he added.
“If you have a panel that votes 3-0 for no liability, or 3-0 for liability, that’s pretty persuasive to the attorneys,” Mr. Michaud said in an interview. “And it’s something they can use in their discussion with their own clients about what to do next.”
The fact that professionals make up the panel enables the case to unfold more smoothly, Mr. Michaud noted.
“It’s very important because if there’s any game playing going on by counsel, having a person with judicial experience, plus another attorney, cuts through that,” he said. “Also having a medical professional on the panel helps the nonmedical panelists understand and evaluate the expert evidence submitted by both parties.”
Reduced claims, higher costs
In Indiana, physician defendants have experienced similar benefits from the state’s medical review panel. Medical malpractice claims for more than $15,000 must be presented to the panel, comprised of an attorney and three health care professionals. After reviewing evidence, the panel provides its opinions, which are admissible at trial but not conclusive, according to state law.
When sued, health care professionals generally feel more comfortable that their conduct will initially be judged by a panel of peers before being presented to a jury, said J. Richard Moore, an Indianapolis-based medical liability defense attorney.
“In my experience, the medical review panel process does reduce the number of truly frivolous claims,” Mr. Moore said in an interview. “The panel adds another layer of process that requires knowledge and experience. ”
However, while the panel helps eliminate invalid claims, the process often can increase legal expenses, Mr. Moore said. The discovery process – subpoenaing records, taking sworn witnesses testimony, and obtaining paid expert witness opinions – is a major cost of litigation, he explained, and also happens before a case goes before the panel.
“In panel cases, there is really no cost savings with respect to discovery, and the two-phase process tends to increase, rather than reduce, attorney fees and costs,” Mr. Moore said. ”This is particularly true on the defense side because we are typically compensated via hourly billing.”
Such costs are counterbalanced if the panel finds in favor of the medical provider and the case is dropped without any plaintiff payment or settlement, he added.
The value of a case review depends greatly on the panelists, according to Karen E. Beach, an appellate attorney in Bloomfield Hills, Mich. In Michigan, the majority of claims go before a mediation panel that includes three attorneys and two health care professionals, one chosen by the plaintiff and one chosen by the defendant. Within 14 days of the panel hearing, the group submits an evaluation of the case regarding the applicable standard of care.
Panels that have more experience with medical malpractice law are more useful than those with less, said Ms. Beach. Overall, however, the case review process in Michigan is widely regarded as unhelpful in getting medical malpractice cases settled, she said.
“The sense, especially from defendants, is that the panel does not spend enough time on each case, and the assessment of the value is not realistic in the eyes of the attorney/client,” Ms. Beach said in an interview. “In fact, the Michigan Supreme Court is presently examining whether to do away with or modify the case-evaluation process.”
Screening panels have been repealed in at least seven states and overturned by courts on constitutional grounds in another six states, including Kentucky.
Broader studies needed
Little national data exists on the overall impact of medical review panels.
Pretrial screening panels had no significant effect on claims frequency or compensation amounts, according to a 2016 report from the Medicare Payment Advisory Commission (MedPAC).
That report looked at seven state tort reform strategies and concluded that data on pretrial screening panels was older and more limited, compared with that of other reforms. Because few early studies identified any notable effects of screening panels, researchers in later studies typically excluded screening panels from the models being tested, according to the MedPAC report.
Michelle M. Mello, PhD, a law professor at Stanford (Calif.) University and coauthor of the MedPAC report, said she was uncertain why there has not been closer study of pretrial screening panels in recent years. Pretrial screening panels probably have little effect because they apply a low standard to complaints, and thus, few claims get weeded out, she said in an interview. “The statutes don’t require them to do much more than say the plaintiff has a plausible case.”
The last comprehensive study on the effects of pretrial screening panels was published almost 10 years ago.
Researchers at Virginia Military University in Lexington evaluated panel data collected during 1991-2004 and data on malpractice awards from the National Practitioner Data Bank for the analysis. The study found review panels had no significant effect on the number of malpractice awards. However, results showed that states with noneconomic damages caps had markedly fewer malpractice awards (Virginia Economic Journal. 2010;15:35-45).
“The fact that damage caps are binding, while [medical malpractice review panel] recommendations are not, could explain the significance of the former, and the insignificance of the latter,” the authors wrote. “It seems reasonable that reforms must be binding, unavoidable, and obligatory to have real effects.”
*Clarification, 6/5/2019: An earlier version of this story indicated that Utah has a voluntary pretrial screening panel. In Utah, a panel review is mandatory, unless both parties agree to waive the hearing process. The accompanying graphic of the United States has been updated accordingly.
The liability climate for Kentucky physicians has long been bleak, according to Bruce A. Scott, MD, president of the Kentucky Medical Association. Insurance premiums are high, few doctors want to relocate to the Bluegrass State, and an overriding fear of lawsuits weighs heavily on the minds of physicians practicing there.
So the physician community was encouraged when in 2017, Kentucky enacted a law requiring all new malpractice claims to go before a medical review panel. The panel, comprised of an attorney and three health care professionals, would review evidence and opine on whether defendants had breached the standard of care. Plaintiffs could then decide whether to drop or resolve the case, or whether to continue to court.
“We saw it as a modest step forward,” Dr. Scott said in an interview. “[The panel] was hopefully going to speed up justice. Those cases that had merit would be settled, and those cases that didn’t have merit would be eliminated to allow the trial court to move on to the cases that needed to be tried.”
The Kentucky Supreme Court disagreed. In November 2018, state justices struck down the panel law as unconstitutional. Requiring plaintiffs to go before a medical review panel delays access to the courts and impedes their right to a speedy trial, the court ruled.
The end to Kentucky’s short-lived medical review panel raises questions about whether such advisory committees are beneficial in medical liability cases. Do review panels help reduce frivolous claims? What effects do the panels have on case duration and court costs?
At least 17 states have some form of pretrial screening panel that evaluates claims against health care professionals. Most panels include legal experts and medical professionals who review evidence and make a determination about potential negligence. In some states, such as Indiana, a panel review is mandatory, whereas in others, like Kansas, the process is voluntary.* Most panel decisions are nonbinding, and parties can proceed to court if they prefer.
Maine: A success story
Maine has experienced marked success with its medical review panel, which has been active since 1986, said Andrew B. MacLean, an attorney and interim CEO for the Maine Medical Association (MMA). The three-person panel, which includes a judicial expert, an attorney, and a physician, addresses whether the defendant’s actions constitute a deviation from the standard of care, whether acts or omissions caused the alleged injury, and the degree to which potential negligence exists on the part of the health care professional and/or the patient.
“The vast majority of medical malpractice claims in Maine are resolved at or before the screening panel stage and our state’s relatively small medical malpractice bar has come to accept this and to work cooperatively within the panel process,” Mr. MacLean said in an interview. “This has not been easy, but we’ve achieved such a result through many years of negotiation among representatives of the judiciary, plaintiffs’ and defense bar, professional liability insurers, and the professional organizations of trial lawyers and physicians.”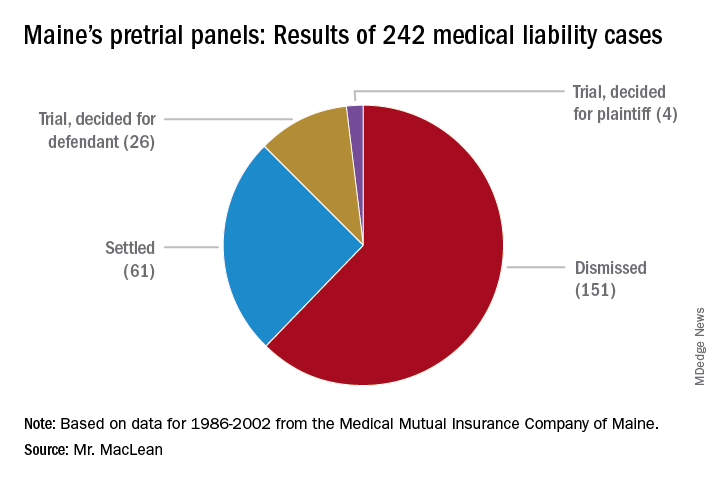
From 1986 to 2002, pretrial panels in Maine analyzed 242 medical liability cases, according to MMA data. Panelists found unanimously for the defendant in 157 cases and unanimously for the plaintiff in 42. In 43 cases, panelists were split. Of the total 242 cases, 151 were ultimately dismissed, 61 cases were settled, and 30 cases went to trial. Of the 30 cases that went to trial, jurors found for the health care professional 26 times.
A medical panel review is a quicker way to determine liability, and the process generally benefits both parties, said Peter Michaud, MMA associate general counsel. Panel hearings last 1-2 days, whereas court trial can take weeks, said Mr. Michaud, who chaired Maine’s panel for 10 years. At the same time, the patient gets their “day in court” and a chance to share their side of the story, he added.
“If you have a panel that votes 3-0 for no liability, or 3-0 for liability, that’s pretty persuasive to the attorneys,” Mr. Michaud said in an interview. “And it’s something they can use in their discussion with their own clients about what to do next.”
The fact that professionals make up the panel enables the case to unfold more smoothly, Mr. Michaud noted.
“It’s very important because if there’s any game playing going on by counsel, having a person with judicial experience, plus another attorney, cuts through that,” he said. “Also having a medical professional on the panel helps the nonmedical panelists understand and evaluate the expert evidence submitted by both parties.”
Reduced claims, higher costs
In Indiana, physician defendants have experienced similar benefits from the state’s medical review panel. Medical malpractice claims for more than $15,000 must be presented to the panel, comprised of an attorney and three health care professionals. After reviewing evidence, the panel provides its opinions, which are admissible at trial but not conclusive, according to state law.
When sued, health care professionals generally feel more comfortable that their conduct will initially be judged by a panel of peers before being presented to a jury, said J. Richard Moore, an Indianapolis-based medical liability defense attorney.
“In my experience, the medical review panel process does reduce the number of truly frivolous claims,” Mr. Moore said in an interview. “The panel adds another layer of process that requires knowledge and experience. ”
However, while the panel helps eliminate invalid claims, the process often can increase legal expenses, Mr. Moore said. The discovery process – subpoenaing records, taking sworn witnesses testimony, and obtaining paid expert witness opinions – is a major cost of litigation, he explained, and also happens before a case goes before the panel.
“In panel cases, there is really no cost savings with respect to discovery, and the two-phase process tends to increase, rather than reduce, attorney fees and costs,” Mr. Moore said. ”This is particularly true on the defense side because we are typically compensated via hourly billing.”
Such costs are counterbalanced if the panel finds in favor of the medical provider and the case is dropped without any plaintiff payment or settlement, he added.
The value of a case review depends greatly on the panelists, according to Karen E. Beach, an appellate attorney in Bloomfield Hills, Mich. In Michigan, the majority of claims go before a mediation panel that includes three attorneys and two health care professionals, one chosen by the plaintiff and one chosen by the defendant. Within 14 days of the panel hearing, the group submits an evaluation of the case regarding the applicable standard of care.
Panels that have more experience with medical malpractice law are more useful than those with less, said Ms. Beach. Overall, however, the case review process in Michigan is widely regarded as unhelpful in getting medical malpractice cases settled, she said.
“The sense, especially from defendants, is that the panel does not spend enough time on each case, and the assessment of the value is not realistic in the eyes of the attorney/client,” Ms. Beach said in an interview. “In fact, the Michigan Supreme Court is presently examining whether to do away with or modify the case-evaluation process.”
Screening panels have been repealed in at least seven states and overturned by courts on constitutional grounds in another six states, including Kentucky.
Broader studies needed
Little national data exists on the overall impact of medical review panels.
Pretrial screening panels had no significant effect on claims frequency or compensation amounts, according to a 2016 report from the Medicare Payment Advisory Commission (MedPAC).
That report looked at seven state tort reform strategies and concluded that data on pretrial screening panels was older and more limited, compared with that of other reforms. Because few early studies identified any notable effects of screening panels, researchers in later studies typically excluded screening panels from the models being tested, according to the MedPAC report.
Michelle M. Mello, PhD, a law professor at Stanford (Calif.) University and coauthor of the MedPAC report, said she was uncertain why there has not been closer study of pretrial screening panels in recent years. Pretrial screening panels probably have little effect because they apply a low standard to complaints, and thus, few claims get weeded out, she said in an interview. “The statutes don’t require them to do much more than say the plaintiff has a plausible case.”
The last comprehensive study on the effects of pretrial screening panels was published almost 10 years ago.
Researchers at Virginia Military University in Lexington evaluated panel data collected during 1991-2004 and data on malpractice awards from the National Practitioner Data Bank for the analysis. The study found review panels had no significant effect on the number of malpractice awards. However, results showed that states with noneconomic damages caps had markedly fewer malpractice awards (Virginia Economic Journal. 2010;15:35-45).
“The fact that damage caps are binding, while [medical malpractice review panel] recommendations are not, could explain the significance of the former, and the insignificance of the latter,” the authors wrote. “It seems reasonable that reforms must be binding, unavoidable, and obligatory to have real effects.”
*Clarification, 6/5/2019: An earlier version of this story indicated that Utah has a voluntary pretrial screening panel. In Utah, a panel review is mandatory, unless both parties agree to waive the hearing process. The accompanying graphic of the United States has been updated accordingly.
The liability climate for Kentucky physicians has long been bleak, according to Bruce A. Scott, MD, president of the Kentucky Medical Association. Insurance premiums are high, few doctors want to relocate to the Bluegrass State, and an overriding fear of lawsuits weighs heavily on the minds of physicians practicing there.
So the physician community was encouraged when in 2017, Kentucky enacted a law requiring all new malpractice claims to go before a medical review panel. The panel, comprised of an attorney and three health care professionals, would review evidence and opine on whether defendants had breached the standard of care. Plaintiffs could then decide whether to drop or resolve the case, or whether to continue to court.
“We saw it as a modest step forward,” Dr. Scott said in an interview. “[The panel] was hopefully going to speed up justice. Those cases that had merit would be settled, and those cases that didn’t have merit would be eliminated to allow the trial court to move on to the cases that needed to be tried.”
The Kentucky Supreme Court disagreed. In November 2018, state justices struck down the panel law as unconstitutional. Requiring plaintiffs to go before a medical review panel delays access to the courts and impedes their right to a speedy trial, the court ruled.
The end to Kentucky’s short-lived medical review panel raises questions about whether such advisory committees are beneficial in medical liability cases. Do review panels help reduce frivolous claims? What effects do the panels have on case duration and court costs?
At least 17 states have some form of pretrial screening panel that evaluates claims against health care professionals. Most panels include legal experts and medical professionals who review evidence and make a determination about potential negligence. In some states, such as Indiana, a panel review is mandatory, whereas in others, like Kansas, the process is voluntary.* Most panel decisions are nonbinding, and parties can proceed to court if they prefer.
Maine: A success story
Maine has experienced marked success with its medical review panel, which has been active since 1986, said Andrew B. MacLean, an attorney and interim CEO for the Maine Medical Association (MMA). The three-person panel, which includes a judicial expert, an attorney, and a physician, addresses whether the defendant’s actions constitute a deviation from the standard of care, whether acts or omissions caused the alleged injury, and the degree to which potential negligence exists on the part of the health care professional and/or the patient.
“The vast majority of medical malpractice claims in Maine are resolved at or before the screening panel stage and our state’s relatively small medical malpractice bar has come to accept this and to work cooperatively within the panel process,” Mr. MacLean said in an interview. “This has not been easy, but we’ve achieved such a result through many years of negotiation among representatives of the judiciary, plaintiffs’ and defense bar, professional liability insurers, and the professional organizations of trial lawyers and physicians.”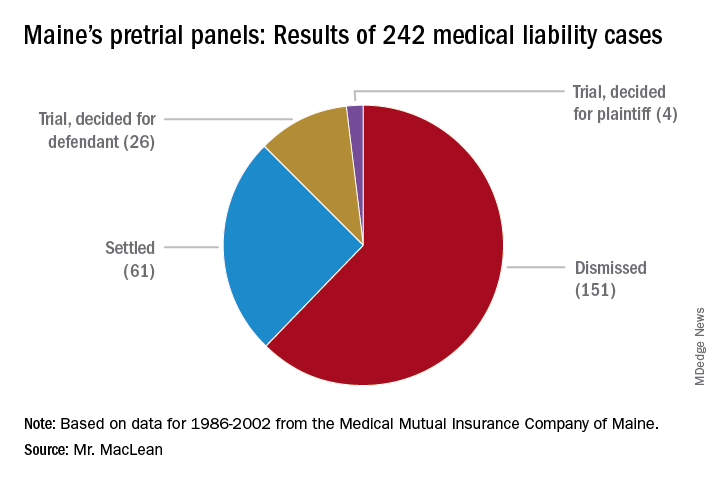
From 1986 to 2002, pretrial panels in Maine analyzed 242 medical liability cases, according to MMA data. Panelists found unanimously for the defendant in 157 cases and unanimously for the plaintiff in 42. In 43 cases, panelists were split. Of the total 242 cases, 151 were ultimately dismissed, 61 cases were settled, and 30 cases went to trial. Of the 30 cases that went to trial, jurors found for the health care professional 26 times.
A medical panel review is a quicker way to determine liability, and the process generally benefits both parties, said Peter Michaud, MMA associate general counsel. Panel hearings last 1-2 days, whereas court trial can take weeks, said Mr. Michaud, who chaired Maine’s panel for 10 years. At the same time, the patient gets their “day in court” and a chance to share their side of the story, he added.
“If you have a panel that votes 3-0 for no liability, or 3-0 for liability, that’s pretty persuasive to the attorneys,” Mr. Michaud said in an interview. “And it’s something they can use in their discussion with their own clients about what to do next.”
The fact that professionals make up the panel enables the case to unfold more smoothly, Mr. Michaud noted.
“It’s very important because if there’s any game playing going on by counsel, having a person with judicial experience, plus another attorney, cuts through that,” he said. “Also having a medical professional on the panel helps the nonmedical panelists understand and evaluate the expert evidence submitted by both parties.”
Reduced claims, higher costs
In Indiana, physician defendants have experienced similar benefits from the state’s medical review panel. Medical malpractice claims for more than $15,000 must be presented to the panel, comprised of an attorney and three health care professionals. After reviewing evidence, the panel provides its opinions, which are admissible at trial but not conclusive, according to state law.
When sued, health care professionals generally feel more comfortable that their conduct will initially be judged by a panel of peers before being presented to a jury, said J. Richard Moore, an Indianapolis-based medical liability defense attorney.
“In my experience, the medical review panel process does reduce the number of truly frivolous claims,” Mr. Moore said in an interview. “The panel adds another layer of process that requires knowledge and experience. ”
However, while the panel helps eliminate invalid claims, the process often can increase legal expenses, Mr. Moore said. The discovery process – subpoenaing records, taking sworn witnesses testimony, and obtaining paid expert witness opinions – is a major cost of litigation, he explained, and also happens before a case goes before the panel.
“In panel cases, there is really no cost savings with respect to discovery, and the two-phase process tends to increase, rather than reduce, attorney fees and costs,” Mr. Moore said. ”This is particularly true on the defense side because we are typically compensated via hourly billing.”
Such costs are counterbalanced if the panel finds in favor of the medical provider and the case is dropped without any plaintiff payment or settlement, he added.
The value of a case review depends greatly on the panelists, according to Karen E. Beach, an appellate attorney in Bloomfield Hills, Mich. In Michigan, the majority of claims go before a mediation panel that includes three attorneys and two health care professionals, one chosen by the plaintiff and one chosen by the defendant. Within 14 days of the panel hearing, the group submits an evaluation of the case regarding the applicable standard of care.
Panels that have more experience with medical malpractice law are more useful than those with less, said Ms. Beach. Overall, however, the case review process in Michigan is widely regarded as unhelpful in getting medical malpractice cases settled, she said.
“The sense, especially from defendants, is that the panel does not spend enough time on each case, and the assessment of the value is not realistic in the eyes of the attorney/client,” Ms. Beach said in an interview. “In fact, the Michigan Supreme Court is presently examining whether to do away with or modify the case-evaluation process.”
Screening panels have been repealed in at least seven states and overturned by courts on constitutional grounds in another six states, including Kentucky.
Broader studies needed
Little national data exists on the overall impact of medical review panels.
Pretrial screening panels had no significant effect on claims frequency or compensation amounts, according to a 2016 report from the Medicare Payment Advisory Commission (MedPAC).
That report looked at seven state tort reform strategies and concluded that data on pretrial screening panels was older and more limited, compared with that of other reforms. Because few early studies identified any notable effects of screening panels, researchers in later studies typically excluded screening panels from the models being tested, according to the MedPAC report.
Michelle M. Mello, PhD, a law professor at Stanford (Calif.) University and coauthor of the MedPAC report, said she was uncertain why there has not been closer study of pretrial screening panels in recent years. Pretrial screening panels probably have little effect because they apply a low standard to complaints, and thus, few claims get weeded out, she said in an interview. “The statutes don’t require them to do much more than say the plaintiff has a plausible case.”
The last comprehensive study on the effects of pretrial screening panels was published almost 10 years ago.
Researchers at Virginia Military University in Lexington evaluated panel data collected during 1991-2004 and data on malpractice awards from the National Practitioner Data Bank for the analysis. The study found review panels had no significant effect on the number of malpractice awards. However, results showed that states with noneconomic damages caps had markedly fewer malpractice awards (Virginia Economic Journal. 2010;15:35-45).
“The fact that damage caps are binding, while [medical malpractice review panel] recommendations are not, could explain the significance of the former, and the insignificance of the latter,” the authors wrote. “It seems reasonable that reforms must be binding, unavoidable, and obligatory to have real effects.”
*Clarification, 6/5/2019: An earlier version of this story indicated that Utah has a voluntary pretrial screening panel. In Utah, a panel review is mandatory, unless both parties agree to waive the hearing process. The accompanying graphic of the United States has been updated accordingly.




