Dermpath Diagnosis
Extramammary Paget Disease
Extramammary Paget disease (EMPD) is an uncommon condition that usually presents in apocrine sweat gland–rich areas, most commonly the vulva...
Yunyoung C. Chang, MD; Campbell Stewart, MD; Emily Y. Chu, MD, PhD; Misha Rosenbach, MD
From the Department of Dermatology, Hospital of the University of Pennsylvania, Philadelphia.
The authors report no conflict of interest.
Correspondence: Misha Rosenbach, MD, 3600 Spruce St, 2nd Floor, Maloney Building, University of Pennsylvania, Philadelphia, PA 19104 (Misha.Rosenbach@uphs.upenn.edu).

Leukemia cutis (LC) is characterized by the infiltration of malignant neoplastic leukocytes or their precursors into the skin and is most often seen in conjunction with systemic leukemia. Patients with LC frequently are in a relative or absolute immunocompromised state. We report the case of a 52-year-old man with primary refractory acute myelogenous leukemia (AML) following allogeneic stem cell transplant (SCT) who presented with a progressive reddish purple nodule with surrounding erythema and central necrosis in the setting of leukocytosis and possible fungal pneumonia. Histopathologic examination revealed an ulcerated dense diffuse dermal infiltrate of large atypical lymphocytes consistent with LC and septate hyphae with acute-angle branching in the dermal blood vessels. Cultures from a biopsied lesion grew Paecilomyces species, a rare but emerging opportunistic infection, despite the patient being on antifungal prophylaxis. This novel report of a rare angioinvasive infection occurring within a lesion of LC supports the need to maintain a high index of suspicion for invasive infection in patients with hematologic malignancy, even those on antifungal prophylaxis.
Practice Points
Leukemia cutis (LC) is characterized by the infiltration of malignant neoplastic leukocytes or their precursors into the skin, most often in conjunction with systemic leukemia.1 Acute myelogenous leukemia (AML) is the second most common cause of LC and the most common form of leukemia among adults.1 Patients with leukemia often are in a relative or absolute immunocompromised state, which may be secondary to neutropenia, chemotherapy regimens, or immunosuppressive regimens following stem cell transplant (SCT). Thus, when evaluating cutaneous lesions consistent with LC in immunocompromised patients, there must be a high index of suspicion for concomitant opportunistic infections.
We report the case of a 52-year-old man with primary refractory AML following allogeneic SCT with relapse who presented with an LC lesion below the knee with concomitant invasive fungal infection despite being on prophylactic oral antifungal therapy.
Case Report
A 52-year-old man with primary refractory AML (M1) of 1 year’s duration presented for evaluation of a slowly progressing reddish purple nodule on the right knee of 2 to 4 months’ duration. The patient had undergone a matched unrelated donor allogeneic SCT 6 months following diagnosis of AML with subsequent disease progression despite reduction of posttransplant graft-versus-host disease prophylactic immune suppression and a cycle of clofarabine. The patient was hospitalized 2 months after the SCT for neutropenic fever and was found to have vancomycin-resistant enterococcal bacteremia, Clostridium difficile colitis, and possible fungal pneumonia. He was treated with voriconazole 200 mg twice daily, which he continued following discharge for antifungal prophylaxis. At the time of discharge, the patient reported that he noticed an asymptomatic “purple papule” on the right knee but did not seek further workup.
Two months later, the patient presented with a fever (temperature, 38.6°C) and leukocytosis (white blood cell count, 130 cells/mL [increased from 53 cells/mL 1 week prior to admission]). Due to his history of immunosuppression and neutropenia, the patient was placed on a broad-spectrum antibiotic regimen of cefepime, daptomycin, and linezolid on admission. Later, vancomycin and gentamicin were added and voriconazole was switched to caspofungin. The patient also received granulocyte-macrophage colony-stimulating factor for neutropenia. During the current hospitalization, blood cultures demonstrated vancomycin-resistant enterococcemia, and computed tomography of the chest revealed findings consistent with multilobar pneumonia.
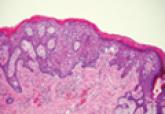
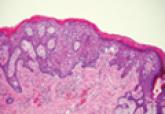
Dermatology was consulted to evaluate the purple nodule on the right knee, which had slowly progressed since his last admission. Physical examination revealed a violaceous, 1.5×1.5-cm nodule with central necrosis covered by black eschar with surrounding erythema (Figure 1). Biopsy specimens for routine histology and a tissue culture were obtained. Histopathologic examination revealed a dense diffuse infiltrate of large hyperchromatic mononuclear cells extending through the dermis, which was consistent with the patient’s known AML (Figure 2). Acid-fast bacillus staining was negative for mycobacterial organisms. Grocott-Gomori methenamine-silver stain demonstrated an overwhelming number of septate fungal hyphae with acute-angle branching, concerning for Aspergillus species (Figure 3). Of note, an Aspergillus serum antigen test was performed at this time and was negative. On repeat review of the routine histologic sections, angioinvasion by hyphae was detected amidst the dense lymphocytic infiltrate (Figure 4).
Given the patient’s immunocompromised state, the presence of angioinvasive fungi on the skin biopsy, and unresolved pneumonia, the patient was restarted on voriconazole for treatment of likely Aspergillus infection. He was continued on chemotherapy for the primary refractory AML and received a donor lymphocyte infusion prior to discharge. After the patient was discharged, the tissue culture grew Paecilomyces, a rare fungal species. The patient died 1 week after discharge.
Figure 2. A punch biopsy specimen demonstrated a dense interstitial infiltrate of hyperchromatic cells extending through the dermis (A)(H&E, original magnification ×200). Higher-power view of monomorphic cells exhibited elevated nuclear-cytoplasmic ratios (B)(H&E, original magnification ×600). | Figure 3. Grocott-Gomori methenamine-silver stain revealed numerous fungal hyphae (A)(original magnification ×200). Higher-power magnification showed septate fungal hyphae (B)(original magnification ×600). |
Comment
Leukemia cutis is an extramedullary manifestation of leukemia that appears in 10% to 15% of patients with AML.2 The frequency of LC differs widely for the various types of AML, with the majority of cases occurring in the acute myelomonocytic leukemia (M4) or acute monocytic leukemia (M5) subtypes.3,4 One large study of AML patients (N=381) demonstrated an incidence of LC in 28.6% of patients with the M4 subtype and 42.9% of those with the M5 subtype, with an incidence of only 7.1% of patients with the M1 subtype.3 It occurs less frequently in chronic myeloproliferative diseases.2,4
Extramammary Paget disease (EMPD) is an uncommon condition that usually presents in apocrine sweat gland–rich areas, most commonly the vulva...

Cutaneous manifestations of leukemia can be defined as specific or nonspecific skin lesions.
