Video

All from the Dermatology Service, Memorial Sloan Kettering Cancer Center, New York, New York. Dr. Yélamos also is from the Dermatology Department, Hospital Clínic, Universitat de Barcelona, Spain. Dr. Rossi also is from the Department of Dermatology, Weill Cornell Medical College, New York.
Drs. Hibler, Yélamos, Cordova, Sierra, Nehal, and Rossi report no conflict of interest. Dr. Rajadhyaksha owns equity in and is a former employee of Caliber Imaging & Diagnostics. This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748 and the Beca Excelencia Fundación Piel Sana (directed to Dr. Yélamos).
The eTable is available in the Appendix in the PDF.
Correspondence: Anthony M. Rossi, MD, Memorial Sloan Kettering Cancer Center, Dermatology Service, 16 E 60th St, Ste 407, New York, NY 10022 (rossia@mskcc.org).

Following institutional review board approval, cases of facial LM/LMM presenting for assessment and treatment from January 2014 to December 2015 were retrospectively reviewed. Initially, the clinical margins of the lesions were determined using Wood lamp and/or dermoscopy. Using HRCM, vertical stacks were taken at the 12-, 3-, 6-, and 9-o'clock positions, and videos were captured along the peripheral margins at the DEJ. To create videomosaics, HRCM video frames were extracted and later stitched using a computer algorithm written in a fourth-generation programming language based on prior studies.10,14 An example HRCM video that was captured and turned into a videomosaic accompanies this article online (http://bit.ly/2oDYS6k). Additional stacks were taken in suspicious areas. We considered an area positive for LM under HRCM when the LM score developed by Guitera et al2 was 2 or more. The algorithm scoring includes 2 major criteria--nonedged papillae and round large pagetoid cells--which score 2 points, and 4 minor criteria, including 3 positive criteria--atypical cells at the DEJ, follicular invasion, nucleated cells in the papillae--which each score 1 point, and 1 negative criterion--broadened honeycomb pattern--which scores -1 point.2
RELATED VIDEO: RCM Videomosaic of Melanoma In Situ
An 82-year-old woman was referred to us for management of an LMM on the left side of the forehead (Figure 1A). Handheld RCM from the biopsy site showed large atypical cells in the epidermis, DEJ, and papillary dermis. Superiorly, HRCM showed large dendritic processes but did not reveal LM features in 3 additional clinically worrisome areas. Biopsies showed LMM at the prior biopsy site, LM superiorly, and actinic keratosis in the remaining 3 areas, supporting the HRCM findings. Due to upstaging, the patient was referred for head and neck surgery. To aid in resection, HRCM was performed intraoperatively in a multidisciplinary approach (Figure 1B). Due to the large size of the lesion, surgical margins were taken right outside the HRCM border. Pathology showed LMM extending focally into the margins that were reexcised, achieving clearance.
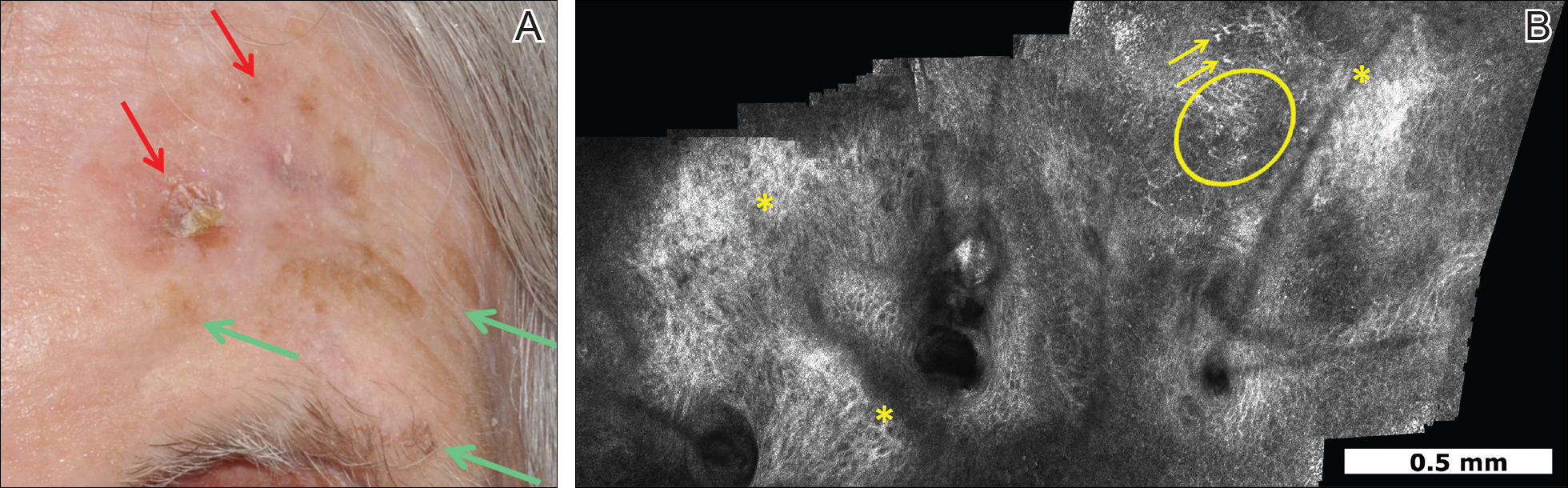
Figure 1. Brown, ill-defined, 1.0×0.5-cm, amelanotic, scaling, atrophic patch on the left side of the forehead with surrounding focal areas of hyperkeratotic brown papules (A). After handheld reflectance confocal microscopy guidance, 2 biopsies were performed at sites that had shown pagetoid cells (red arrows). These biopsies showed lentigo maligna melanoma (0.95 mm in depth). Three biopsies at clinically suspicious areas but without confocal features suggestive for lentigo maligna also were done and showed actinic keratoses (green arrows). Videomosaic obtained after capturing videos using handheld reflectance confocal microscopy was used to guide demarcation of the surgical margins (B). It showed clusters of dendritic atypical cells (circle) and large, hyperreflectile, round cells (arrows) that occasionally invaded the hair follicles. Other areas also showed amorphous collagen and irregular honeycomb pattern (asterisks) related to solar elastosis.
An 88-year-old woman presented with a slightly pigmented, 2.5×2.3-cm LMM on the left cheek. Because of her age and comorbidities (eg, osteoporosis, deep vein thrombosis in both lower legs requiring anticoagulation therapy, presence of an inferior vena cava filter, bilateral lymphedema of the legs, irritable bowel syndrome, hyperparathyroidism), she was treated with imiquimod cream 5% achieving partial response. The lesion was subsequently excised showing LMM extending to the margins. Not wanting to undergo further surgery, she opted for radiation therapy. Handheld RCM was performed to guide the radiation field, showing pagetoid cells within 1 cm of the scar and clear margins beyond 2 cm. She underwent radiation therapy followed by treatment with imiquimod. On 6-month follow-up, no clinical lesion was apparent, but HRCM showed atypical cells. Biopsies revealed an atypical intraepidermal melanocytic proliferation, but due to patient's comorbidities, close observation was decided.
A 78-year-old man presented with an LMM on the right preauricular area. Handheld RCM demonstrated pleomorphic pagetoid cells along and beyond the clinical margins. Wide excision with sentinel lymph node biopsy was planned, and to aid surgery a confocal map was created (Figure 2). Margins were clear at 1 cm, except inferiorly where they extended to 1.5 cm. Using this preoperative HRCM map, all intraoperative sections were clear. Final pathology confirmed clear margins throughout.
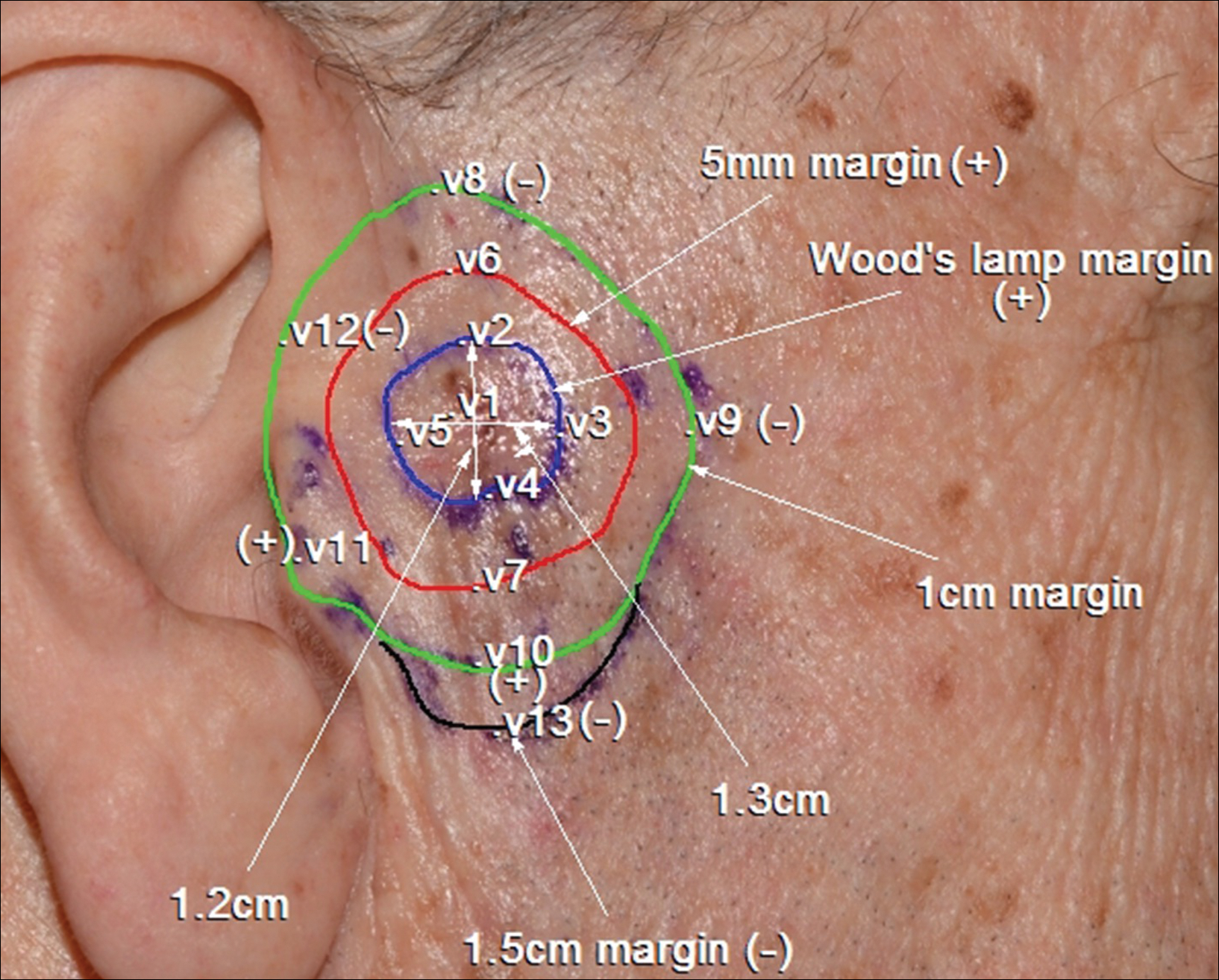
Figure 2. Confocal mapping of lentigo maligna melanoma on the right preauricular area. The inner blue line demarcates Wood lamp margins. The red line shows the 5-mm surgical margin, which was positive throughout. The green line shows the 10-mm surgical margin, which showed positive reflectance confocal microscopy findings (dendritic atypical cells invading hair follicles, junctional thickening, and nonedged papillae) suggestive of subclinical lentigo maligna at the area close to the tragus (v11) and at the 6-o’clock position (v10). The black line indicates the 15-mm margin where disease was not detected (v13). The lesion was removed guided by this confocal mapping with clear margins. V indicates sites where stacks of images were taken in the vertical direction.
A 62-year-old man presented with hyperpigmentation and bleeding on the left cheek where an LMM was previously removed 8 times over 18 years. Handheld RCM showed pleomorphic cells along the graft border and interestingly within the graft. Ten biopsies were taken, 8 at sites with confocal features that were worrisome for LM (Figures 3A and 3B) and 2 at clinically suspicious sites. The former revealed melanomas (2 that were invasive to 0.3 mm), and the latter revealed solar lentigines. The patient underwent staged excision guided by HRCM (Figure 3C), achieving clear histologic margins except for a focus in the helix. This area was RCM positive but was intentionally not resected due to reconstructive difficulties; imiquimod was indicated in this area.
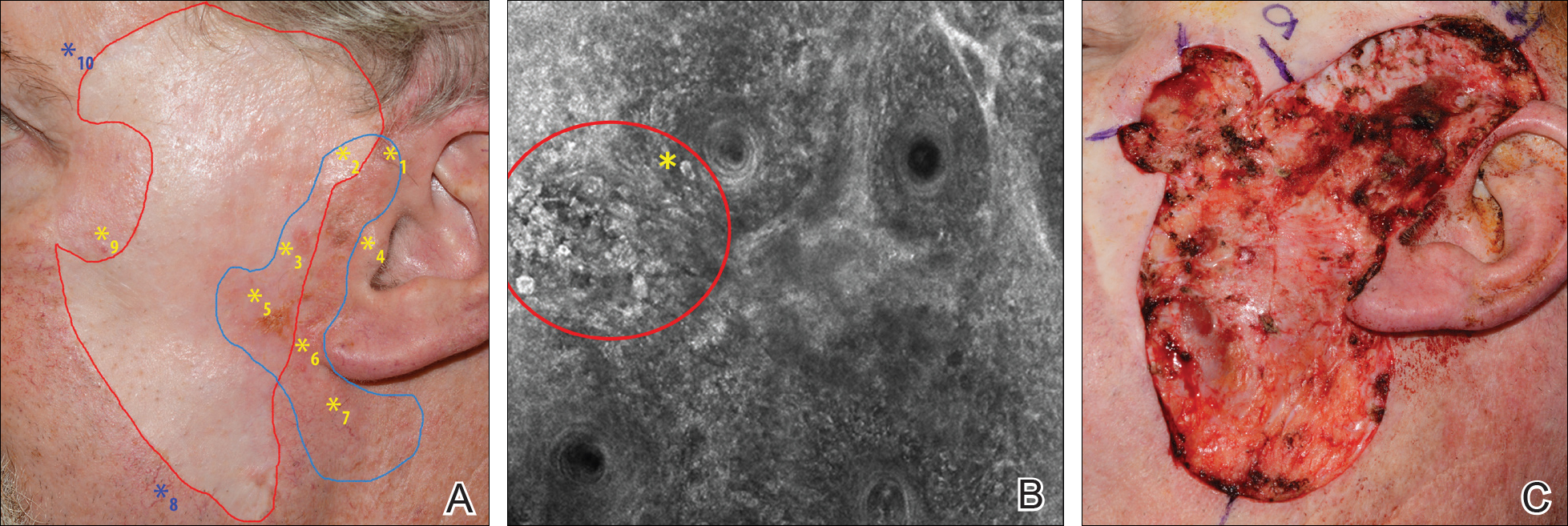
Figure 3. Patient with 8 prior surgeries for excision of lentigo maligna melanoma on the left cheek (A). The blue line outlines Wood lamp margins. The red line outlines the site of a prior graft. Ten mapping biopsies were performed guided by reflectance confocal microscopy. Eight were from sites with positive findings (yellow asterisks) and were confirmed histologically as lentigo maligna. Two biopsies were taken at clinically suspicious areas without positive features (blue asterisks) and showed solar lentigines on histology. Reflectance confocal microscopy showed clusters of large, round, atypical cells (red circle) with some invading hair follicles (yellow asterisk), suggestive of lentigo maligna and confirmed on biopsy (B). Other features observed included atypical pagetoid cells and dendritic processes invading the hair follicles. Final surgical defect after clinical, dermoscopic, Wood lamp, and confocal evaluation (C). Repair included removal of the prior grafts and replacement with a new split-thickness skin graft from the abdomen.
An 85-year-old woman with 6 prior melanomas over 15 years presented with ill-defined light brown patches on the left cheek at the site where an LM was previously excised 15 years prior. Biopsies showed LM, and due to the patient's age, health, and personal preference to avoid extensive surgery, treatment with imiquimod cream 5% was decided. Over a period of 6 to 12 months, she developed multiple erythematous macules with 2 faintly pigmented areas. Handheld RCM demonstrated atypical cells within the papillae in previously biopsied sites that were rebiopsied, revealing LMM (Breslow depth, 0.2 mm). Staged excision achieved clear margins, but after 8 months HRCM showed LM features. Histology confirmed the diagnosis and imiquimod was reapplied.




In an article published online on January 26 in the Journal of the American Academy of Dermatology, my colleagues and I (Menge et al)...
