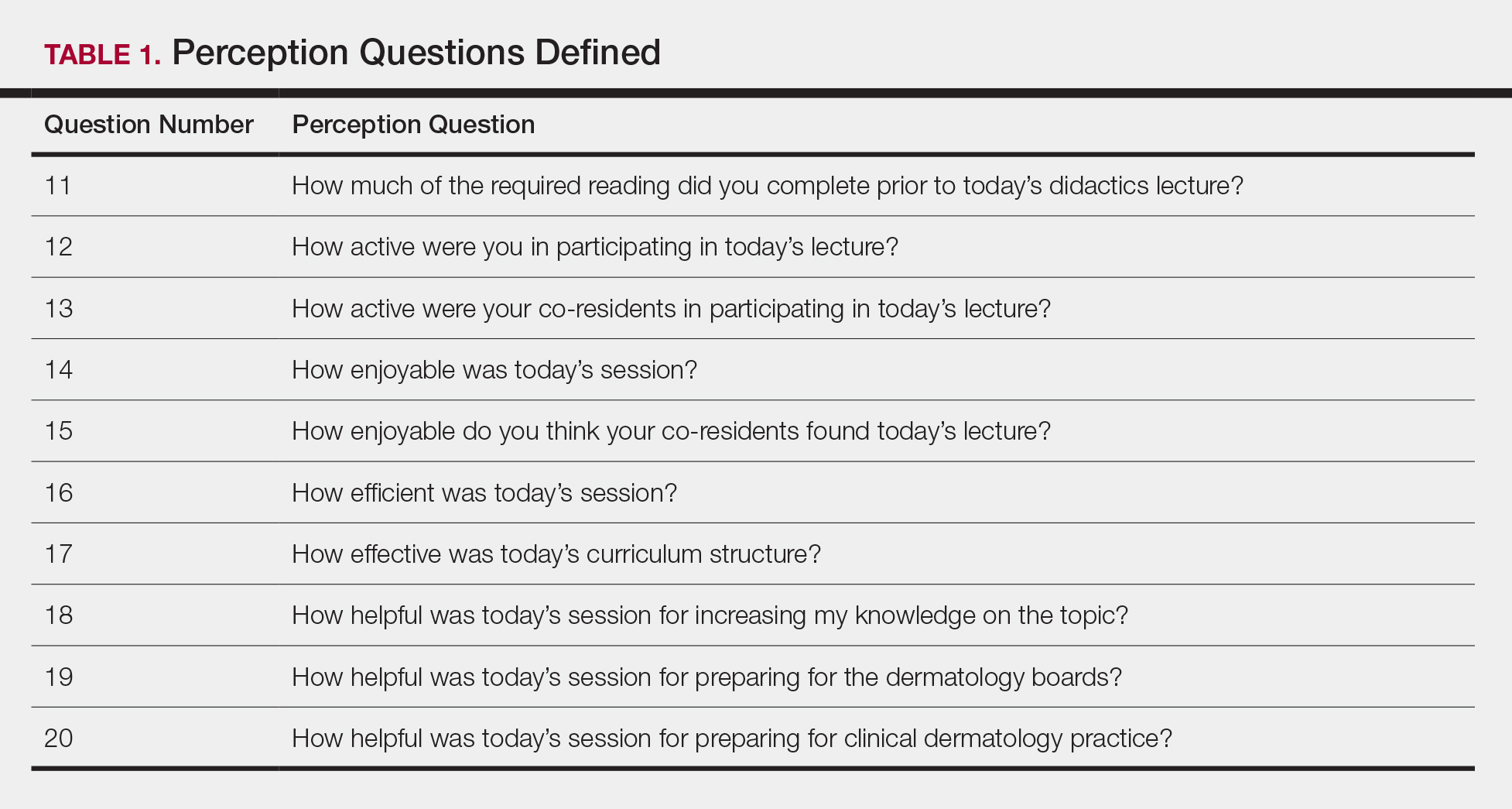
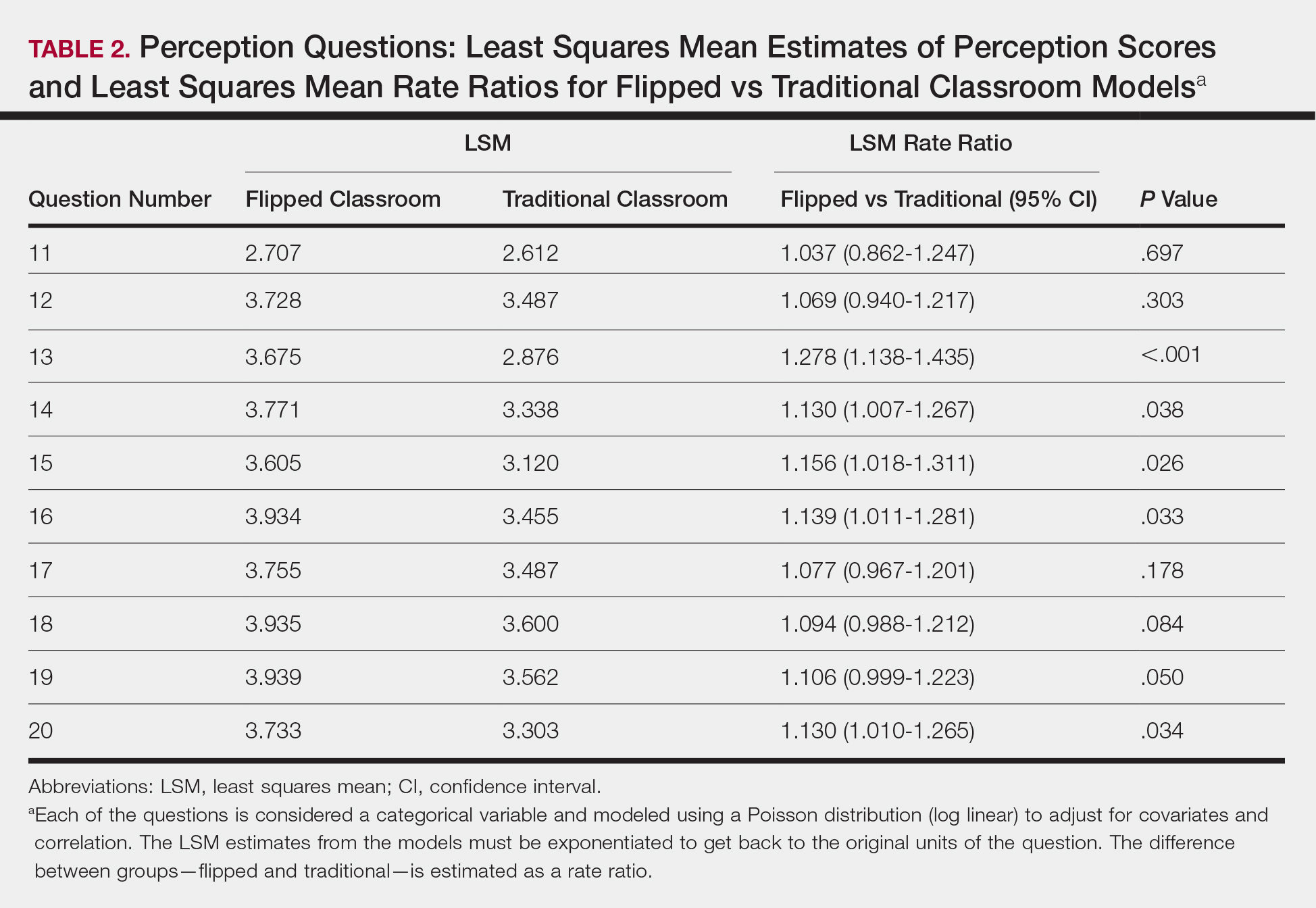
Each resident also answered 10 perception questions (Table 1). When comparing the responses by quiz type (Table 2), there was a significant difference for several questions in favor of the flipped classroom: how actively residents thought their co-residents participated in the lecture (P<.001), how much each resident enjoyed the session (P=.038), and how much each resident believed their co-residents enjoyed the session (P=.026). Additionally, residents thought that the flipped classroom sessions were more efficient (P=.033), better prepared them for boards (P=.050), and better prepared them for clinical practice (P=.034). There was not a significant difference in the amount of reading and preparation residents did for class (P=.697), how actively the residents thought they participated in the lecture (P=.303), the effectiveness of the day’s curriculum structure (P=.178), or whether residents thought the lesson increased their knowledge on the topic (P=.084).
Comment
The traditional model in medical education has undergone changes in recent years, and researchers have been looking for new ways to convey more information in shorter periods of time, especially as the field of medicine continues to expand. Despite the growing popularity and adoption of the flipped classroom, studies in dermatology have been limited. In this study, we compared a traditional classroom model with the flipped model, assessing both knowledge acquisition and resident perception of the experience.
There was not a significant difference in mean objective quiz scores when comparing the 2 curricula. The flipped model was not better or worse than the traditional teaching model at relaying information and promoting learning. Rather, there was a significant difference in quiz scores based on the individual resident and on the individual quiz. Individual performance was not affected by the teaching model but rather by the individual resident and lecture topic.
These findings differ from a study of internal medicine residents, which revealed that trainees in a quality-improvement flipped classroom had greater increases in knowledge than a traditional cohort.7 It is difficult to make direct comparisons to this group, given the difference in specialty and subject content. In comparison, an emergency medicine program completed a cross-sectional cohort study of in-service examination scores in the setting of a traditional curriculum (2011-2012) vs a flipped curriculum (2015-2016) and found that there was no statistical difference in average in-service examination scores.8 The type of examination content in this study may be more similar to the quizzes that our residents experienced (ie, fact-based material based on traditional medical knowledge).
The dermatology residents favored the flipped curriculum for 6 of 10 perception questions, which included areas of co-resident participation, personal and co-resident enjoyment, efficiency, boards preparation, and preparation for clinical practice. They did not favor the flipped classroom for prelecture preparation, personal participation, lecture effectiveness, or knowledge acquisition. They perceived their peers as being more engaged and found the flipped classroom to be a more positive experience. The residents thought that the flipped lectures were more time efficient, which could have contributed to overall learner satisfaction. Additionally, they thought that the flipped model better prepared them for both the boards and clinical practice, which are markers of future performance.
These findings are consistent with other studies that revealed improved postcourse perception scores for a quality improvement emergency medicine–flipped classroom. Most of this group preferred the flipped classroom over the traditional after completion of the flipped curriculum.9 A neurosurgery residency program also reported increased resident engagement and resident preference for a newly designed flipped curriculum.10
Overall, our data indicate that there was no objective change in knowledge acquisition at the time of the quiz, but learner satisfaction was significantly greater in the flipped classroom model.
Limitations
This study was comprised of a small number of residents from a single institution and was based on a limited number of lectures given throughout the year. All lectures during the study year were flipped with the exception of the 6 traditional study lectures. Therefore, each resident who presented a traditional lecture was not blinded for her individual assigned lecture. In addition, because traditional lectures only occurred on study days, once the lectures started, all trainees could predict that a content quiz would occur at the end of the session, which could potentially introduce bias toward better quiz performance for the traditional lectures.
Conclusion
When comparing traditional and flipped classroom models, we found no difference in knowledge acquisition. Rather, the difference in quiz scores was among individual residents. There was a significant positive difference in how residents perceived these teaching models, including enjoyment and feeling prepared for the boards. The flipped classroom model provides another opportunity to better engage residents during teaching and should be considered as part of dermatology residency education.
Acknowledgments
Duke Social Sciences Institute postdoctoral fellow Scott Clifford, PhD, and Duke Dermatology residents Daniel Chang, MD; Sinae Kane, MD; Rebecca Bialas, MD; Jolene Jewell, MD; Elizabeth Ju, MD; Michael Raisch, MD; Reed Garza, MD; Joanna Hooten, MD; and E. Schell Bressler, MD (all Durham, North Carolina).