An 85-year-old man presented to the ED with a presyncopal episode, which included lightheadedness and sharp chest pain. His medical history was significant for atrial fibrillation, for which he was taking warfarin. In addition to warfarin, the patient had recently completed a 5-day dose pack of azithromycin for pneumonia. Despite treatment for the pneumonia, he reported persistent episodes of cough and mild hemoptysis.
Radiographs and a noncontrast computed tomography (CT) scan of the chest were obtained. A representative posterior-anterior radiograph (Figure 1a) and a coronal noncontrast CT image (Figure 2a) are shown above.
What is your diagnosis?
What additional imaging, if any, should be performed?
Answer
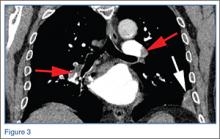
The frontal chest radiograph demonstrated abnormal peripheral opacity at the left lung base (white arrow, Figure 1b), and the noncontrast chest CT demonstrated a peripheral, wedge/pyramid-shaped subpleural ground-glass opacity (white arrow, Figure 2b). Based on the persistent peripheral opacity despite treatment, and the patient’s clinical symptoms of acute sharp chest pain/hemoptysis, a pulmonary infarct was considered as part of the differential diagnosis, and a contrast-enhanced pulmonary embolism (PE) protocol CT was obtained for further evaluation. A coronal image from the contrast-enhanced CT demonstrated the wedge-shaped peripheral opacity (white arrow, Figure 3) as well as filling defects in the bilateral pulmonary arteries (red arrows, Figure 3), indicating the presence of PE.
Large PE, such as those seen in this case, may result in peripheral infarcts due to occlusion of the pulmonary arteries. The subpleural location of the infarcts typically causes acute pleuritic chest pain, which this patient experienced.
The radiographic appearance of pulmonary infarct was originally described in 1940 by Hampton and Castleman and is commonly referred to as Hampton’s hump.1 Chest radiographic imaging, however, is often not specific in patients with suspected PE. In the Prospective Investigation of Pulmonary Embolism Diagnosis Study, the most common chest radiographic findings in patients with angiographically documented PE were atelectasis and/or parenchymal opacities in the affected lung zone, but there was no significant difference in prevalence seen in patients without PE. Although a Hampton’s hump is a more specific finding, it is often not present, and is therefore not a reliable marker for PE.2 As this case illustrates, in patients with high clinical probability of PE, peripheral areas of consolidation may not always represent pneumonia and should be evaluated further with contrast-enhanced CT.