Case
A 39-year-old woman, previously in good health, presented to the ED with a chief complaint of severe sore throat, which she said had begun approximately 4 hours prior and was rapidly worsening. She thought her voice sounded muffled, and said she was now having difficulty swallowing her saliva. The patient denied fever but did admit to chills. She experienced onset of shortness of breath 30 minutes prior to arrival to the ED.
The patient stated that she was a house painter and had been working in the home of someone who had several dogs. While not previously allergic to animals, the patient was concerned exposure to the dogs might have contributed to her symptoms. Regarding her social history, the patient admitted to daily consumption of beer, but denied smoking cigarettes. She had no known drug allergies.
On physical examination, the patient was afebrile. Her vital signs were: heart rate, 125 beats/min; blood pressure, 137/74 mm Hg; and respiratory rate, 18 breaths/min. Oxygen saturation was 99% on room air. Overall, the patient appeared anxious and exhibited mild inspiratory stridor. Examination of the eyes and ears were normal. There was no obvious inflammation or swelling of the posterior pharynx; the tongue was normal; there was no swelling of the floor of the mouth; and the uvula was midline and without swelling.
The patient was noted to having difficulty handling her secretions. She exhibited full range of motion of her neck. Her trachea was tender upon palpation but without jugular venous distension or lymphadenopathy. The cardiac examination was significant for tachycardia with a regular rhythm and without murmurs, rubs, or gallops; the pulmonary examination was normal except for transmitted upper airway sounds. The patient’s abdominal, dermatological, and neurological examinations were all normal.
Based on the examination findings, the differential diagnosis included allergic reaction, angioedema, epiglottitis, and retropharyngeal abscess. An intravenous (IV) line was placed and blood was drawn for laboratory evaluation, which included a complete blood count, basic metabolic panel (BMP), and a quantitative pregnancy test. Given the patient’s history, the emergency physician (EP) was most concerned for an allergic reaction, and administered epinephrine 0.5 mg (1:1,000) intramuscularly (IM) in the mid-anterolateral thigh, in addition to methylprednisolone, 125 mg; diphenhydramine, 25 mg; and famotidine, 20 mg IV.
A portable soft-tissue lateral radiograph of the neck was obtained. Radiology services interpreted the film as showing “prominent prevertebral soft tissues and epiglottis.
Retropharyngeal abscess or inflammation, potentially complicated with epiglottitis, has to be considered. Recommend computed tomography (CT) scan of the neck to further evaluate” (Figure 1).At this point, the patient appeared relatively stable and without progression of symptoms. Since there was the possibility of an infectious etiology, she was given piperacillin/tazobactam, 4.5 g IV.
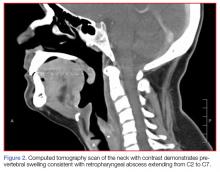
Since the patient was able to tolerate being placed in the supine position, she was taken to radiology services for a CT scan of the neck with IV contrast, which was interpreted by radiology services as “findings consistent with a retropharyngeal abscess extending from C2 to C7” (Figure 2).Laboratory evaluation results were significant for an elevated white blood cell count (WBC) of 14.8 ×109/L, but without a left shift; BMP results were within normal limits, and the pregnancy test was negative.
Based on these findings, otolaryngology services were consulted. The consulting otolaryngologist sprayed oxymetazoline and tetracaine into both of the patient’s nostrils and performed a flexible fiberoptic nasopharyngolaryngoscopy. During the procedure, a significant amount of diffuse supraglottic edema was noted, but no posterior pharyngeal wall edema.
Based on the presence of stridor, difficulty managing secretions, and significant amount of supraglottic edema, the patient was taken to the surgical suite for urgent airway control. She was given dexamethasone, 10 mg IV, and after some difficulty, the anesthesiologist orally intubated the patient with a 7.0-mm endotracheal tube. Examination during the procedure noted diffuse supraglottic edema but no other abnormalities.
The patient was transferred to the intensive care unit (ICU) and treated with IV piperacillin/tazobactam and dexamethasone. While in the ICU, the patient became extremely agitated and combative. After further inquiry into the patient’s social history, the patient’s husband reported that his wife drank 12 to 13 beers nightly. The patient required treatment for alcohol withdrawal with IV benzodiazepines, sedation, and physical restraints. By hospital day 9, she was extubated and tolerated fluids by mouth. On hospital day 10, her mental status had returned to baseline, her WBC was within normal limits, and she no longer complained of difficulty swallowing. The patient was discharged home on hospital day 11 with a final diagnosis of supraglottitis and alcohol withdrawal, and she was given a prescription for amoxicillin/clavulanate. Unfortunately, she did not return for her follow-up appointments.