The diagnosis of aortic dissection is often challenging due to its various presentations and the frequent absence of classic findings. This high-morbidity and high-mortality condition may present with nonspecific chest, back, or abdominal pain, and is often associated with hypotension.1 Point-of-care (POC) ultrasound in the ED allows for rapid diagnosis of this time-sensitive disease.
Case
A 70-year-old woman presented to the ED for evaluation of acute sharp chest pain, which she stated began while she was exercising earlier that day. The pain was substernal and radiated to her upper back. The patient also described associated lightheadedness and dyspnea, but denied any focal weakness or paresthesias. Her vital signs were remarkable for a blood pressure of 90/31 mm Hg and a heart rate of 42 beats/min. A bedside ultrasound of the patient’s aortic root and abdominal aorta was performed to assess for evidence of aortic dissection.
Imaging Technique
To evaluate for aortic dissection using POC ultrasound, views of the aortic root and the abdominal aorta should be obtained with the patient in the supine position. The phased array (cardiac) probe is used to obtain the parasternal long axis (PSLA) view of the heart to visualize the aortic root. The PSLA view is obtained by placing the probe in the third or fourth intercostal space, adjacent to the left sternal border, with the probe parallel to the long axis of the left ventricle (Figure 1). The American Society of Echocardiography recommends measuring the aortic diameter at the sinus of Valsalva, but measurement of the largest visible portion of the aortic root may be more practical.2,3 Measurement of the aortic root diameter should occur at end diastole.2,3 Tricks for better visualization of the aortic root include tilting the probe tail 10° toward the patient’s right elbow (ie, aiming the probe footprint toward the patient’s left shoulder), or placing the patient in the left lateral decubitus position. Values greater than 4 cm indicate aortic root dilatation.4 Figure 2 demonstrates the PSLA view in our patient, showing the dilated aortic root, which measured roughly 5 cm.
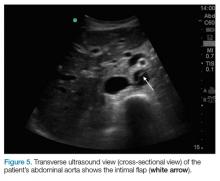
The abdominal aorta is best visualized using a low-frequency curvilinear (abdominal) probe. The aorta should be visualized in the transverse plane from the diaphragm to its bifurcation by placing the probe in the epigastrium and slowly moving it inferiorly to the level of the umbilicus (Figure 3). The aorta can then be visualized in the longitudinal plane by rotating the probe clockwise until it is parallel with the long axis of the aorta (Figure 4). Visualization of an intimal flap is the most common sonographic finding associated with an abdominal aortic dissection. In our patient, an intimal flap was visualized in both the transverse and longitudinal views (Figures 5 and 6).
Discussion
Aortic dissection is a medical emergency—one that has a reported in-hospital mortality of 27.4%.1 Therefore, prompt diagnosis of an aortic dissection in the ED is crucial to improving patient outcomes. Traditionally, emergency physicians (EPs) have relied on aortography and contrast-enhanced computed tomography (CT) to diagnose aortic dissection. However, both of these modalities require a considerable length of time, injection of contrast material, and often transportation of the patient from the ED.
Point-of-care ultrasound provides a fast and noninvasive tool for the diagnosis of aortic dissection. Several recent case reports and case series have highlighted the utility of POC ultrasound to diagnose aortic dissection in the ED.5-7
As our case demonstrates, dilatation of the thoracic aorta and the presence of an intimal flap are indicators of aortic dissection. Evaluation of transthoracic and transabdominal ultrasound for aortic dissection shows that aortic root dilatation has a sensitivity of 77% and specificity of 95%, and visualization of an intimal flap has a sensitivity of 67% to 80% and a specificity of 99% to 100%.4,8-11 Therefore, a combination of a bedside transthoracic and transabdominal ultrasound provides a comprehensive bedside evaluation for aortic dissection.
Case Conclusion
After the results of the POC transthoracic and transabdominal ultrasound were reviewed, we promptly consulted the vascular surgery team. They performed a CT scan verifying a DeBakey type I aortic dissection involving both the ascending aorta and the descending aorta. The patient was subsequently taken to the operating room for definitive repair with a graft. She was discharged home on hospital day 9 in good condition.
Summary
Point-of-care ultrasound is a useful bedside tool for the rapid diagnosis of aortic dissection in the ED. The aortic root dilatation seen on the PSLA view and the presence of an intimal flap seen on either transthoracic or transabdominal views of the aorta are both highly sensitive for aortic dissection.