March 24 is World TB Day. It was on this date in 1882 that physician Robert Koch announced the discovery of Mycobacterium tuberculosis, the causative agent of tuberculosis. Worldwide, activities are planned to raise awareness of TB and to support initiatives for prevention, better control, and ultimately the elimination of this disease.
Globally in 2015, the World Health Organization estimated there were 10.4 million new cases of TB, including 1 million in children. Data from the United States reveal that after 20 years of annual decline, the incidence of TB has plateaued. In 2015, 9,563 cases of TB disease were reported, including 440 cases in children less than 15 years of age. While the overall incidence was 3 cases per 100,000, the incidence among foreign-born persons was 15.1 cases per 100,000. There were 3,201 cases (33.5%) among U.S.-born individuals. Foreign-born persons accounted for 66.2% of cases; however, the majority of those cases were diagnosed several years after their arrival in the United States. The top five countries of origin of these individuals were China, India, Mexico, the Philippines, and Vietnam. In contrast, only one-quarter of all pediatric cases occurred in foreign-born children. Four states (California, Florida, New York, and Texas) reported more than 500 cases each in 2015, as they have for the last 7 consecutive years. In 2015, these states accounted for slightly more than half (4,839) of all cases (MMWR 2016 Mar 25;65[11]:273-8).
Why did the incidence seem to plateau? The number of cases of coinfection with HIV has declined, and although the incidence of TB is higher in foreign-born individuals, the incidence in this group also has decreased yearly. One concern is the continued transmission of TB within the United States, based on molecular genotyping of TB cases and the persistence of transmission among U.S.-born children. Are more cases of untreated latent TB infection reactivating? Could this be one explanation for the higher rate of cases occurring in U.S.-born children? Public health officials still are reviewing the data to explain the plateauing of the decline.Why as pediatricians should we be concerned? TB in a child is a sentinel event and represents recent or ongoing transmission. Young children who are infected are more likely to progress to TB disease and develop severe manifestations such as miliary TB or meningitis. Children less than 4 years old and those with certain underlying disorders, including those with an immunodeficiency or who are receiving immunosuppressive agents, also are at greater risk for progression from infection to disease. Other predictors of disease progression include diagnosis of the infection within the past 2 years, use of chemotherapy and high-dose corticosteroids, as well as certain cancers, diabetes, and chronic renal failure.
Once infected, most children and adolescents remain asymptomatic. If disease occurs, symptoms develop 1-6 months after infection and include fever, cough, weight loss or failure to thrive, night sweats, and chills. Chest radiographic findings are nonspecific. Infiltrates and intrathoracic lymph node enlargement may or may not be present. However, our goal is to diagnose at-risk children with infection, treat them, and avoid their progression to TB disease.
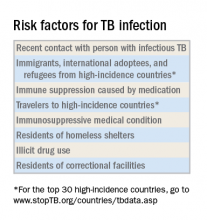
Routine screening of all patients is discouraged because it may lead to false-positive tests and unnecessary interventions. Targeted screening of at-risk patients has been recommended by both the American Academy of Pediatrics and the Centers for Disease Control and Prevention. Being foreign born, having a parent who is foreign born, and residing and/or traveling outside of the United States to high-incidence countries are just a few risk factors. Residence in a homeless shelter or a correctional facility is also a risk factor. Many shelters now house families and, unfortunately, some of our youth have been incarcerated. In terms of U.S.-born children with TB, one study noted that the TB rate in children with at least one foreign-born parent was six times greater than if both parents were born in the United States (Pediatrics. 2014 Mar;133[3]:e494-504). Keep this in mind when screening.Screening tests
A positive tuberculin skin test (TST) can be seen in both latent TB infection and TB disease. It indicates that the individual may be infected with M. tuberculosis. Reactivity is apparent 2-10 weeks after initial infection. BCG vaccine administration may produce a false-positive TST result. It is still the preferred testing method in children less than 5 years of age. The results are interpreted the same way regardless of prior BCG administration. False-negative test results can occur under a variety of circumstances including when there is a viral infection, inappropriate administration, or an inexperienced reader.The interferon-gamma release assay is a blood test that has a greater specificity than TST and requires only one visit. A positive test is seen in both latent TB infection and TB disease. There is no cross-reaction with BCG. This is the ideal test for prior BCG recipients and others who are unlikely to return for TST readings and are at least 5 years of age.
A chest radiograph is required to differentiate latent TB infection from TB disease. Latent TB infection is diagnosed when there is an absence of parenchymal disease, opacification, or intrathoracic adenopathy.
Treatment of latent TB infection versus TB disease is beyond the scope of this article. Consultation with an infectious disease expert is recommended.
For additional information and resources, go to www.cdc.gov/tb, and for a sample TB risk assessment tool, go to www.cdc.gov/tb/publications/ltbi/appendixa.htm.
As we mark the passing of another World TB Day, we have one goal – to identify, screen, and treat children and adolescents at risk for latent TB infection and help eliminate future cases of TB disease.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.