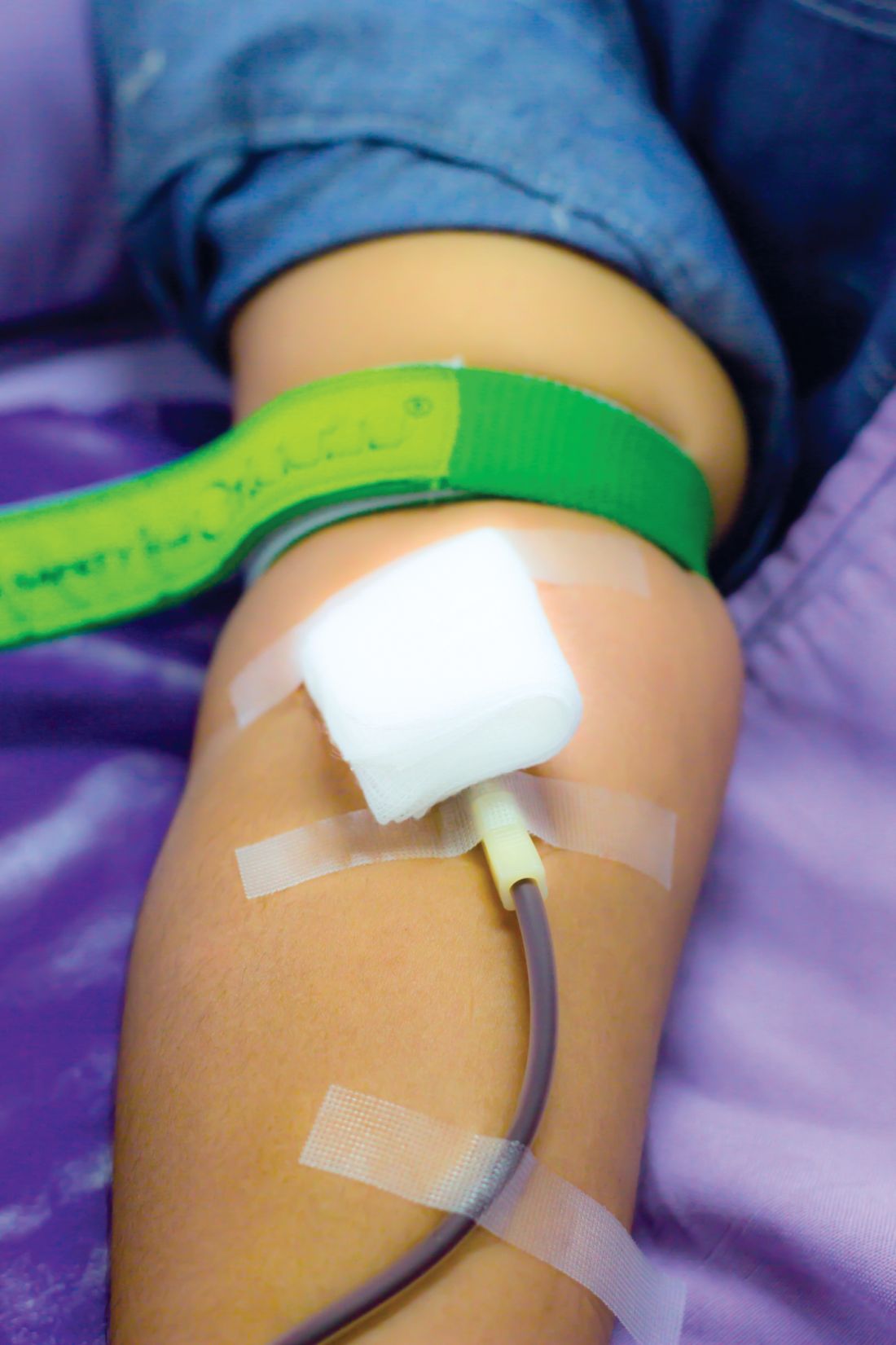
Reducing the interval between blood donations from every 12 weeks to every 8 weeks increases blood units collected with little ill effects on donor quality of life other than symptoms related to iron deficiency, based on results reported by the INTERVAL Trial Group.
In the United States, men and women can donate blood every 8 weeks; the Food and Drug Administration and the AABB (formerly the American Association of Blood Banks) have considered lengthening the 8-week minimum inter-donation interval to reduce the risk of iron deficiency. The current practice in the United Kingdom is to allow men to donate every 12 weeks and women every 16 weeks, the authors noted.
“More frequent blood donation is a feasible and safe option for donors in the U.K., and gives blood services the short-term option of more frequent collection from donors if the supply falls or demand rises,” wrote Emanuele Di Angelantonio, MD, of the University of Cambridge and National Health Service Blood and Transplant, and fellow INTERVAL Trial Group members. “Our study has provided the first randomised evaluation, including precise quantification, of key measures of efficiency and safety that blood services need to ... safeguard donor health and maintain the blood supply.The INTERVAL study examined hemoglobin levels, ferritin levels, and self-reported symptoms as well as the number of blood donations over a 2-year period among 22,466 men randomly assigned to either 8-, 10-, or 12-week blood donation intervals and 22,797 women randomly assigned to donation intervals of 12, 14, and 16 weeks.
Men in the 8-week interval group donated significantly more blood on a per-donor basis, contributing 1.69 and 7.9 units more than the men in the 10- and 12-week interval groups, respectively. Similarly, women in the 12-week interval group contributed approximately 0.84 and 0.46 units more than did women in the 14- and 16-week interval groups.
Hemoglobin and ferritin concentrations stayed relatively stable throughout the study in men and women in all donation interval groups. The baseline hemoglobin and ferritin averages were 149.7 g/L and 44.9 mcg/L in men, and 133.9 g/L and 24.6 mcg/L in women, respectively. Ultimately, mean hemoglobin level decreased by 1%-2%. Ferritin level decreased by 15%-30%, indicating that it is a more accurate marker of iron depletion, the study authors wrote. The report was published online in The Lancet.
The researchers also analyzed self-reported symptoms associated with blood donations derived from donor follow-up surveys sent at 6-, 12-, and 18-month intervals. At the end of the 2-year study, donors underwent a series of cognitive function tests and answered a physical activity questionnaire. Increased donation rates correlated with increased symptoms of iron deficiency such as tiredness, restless legs, and dizziness. This effect was reported more strongly in men.
About 10% of participants were allowed to donate despite having baseline hemoglobin concentrations below the minimum regulatory threshold, said the authors, who said that the screening method used in the United Kingdom to test eligibility to donate needs to be reviewed.
“In response to these findings, we have started the COMPARE study (ISRCTN90871183) to provide a systematic, within-person comparison of the relative merits of different haemoglobin screening methods,” they wrote
The study was funded by National Health Service Blood and Transplant and the National Institute for Health Research Blood and Transplant Research Unit in Donor Health and Genomics (NIHR BTRU-2014-10024).