Conference Coverage
Experts say don’t SPRINT to adopt low blood pressure target
NEW ORLEANS – The SPRINT trial target of systolic blood pressure less than 120 mm Hg doesn’t apply to most hypertensive patients.

AT THE ESC CONGRESS 2017
BARCELONA – How low to go in treating hypertension is a topic of considerable recent controversy. Now the HOPE-3 trial investigators have weighed in, reporting that optimal outcomes in their landmark randomized trial were seen with an achieved, on-treatment systolic blood pressure of 130-140 mm Hg and a diastolic blood pressure of 75-80 mm Hg, Eva M. Lonn, MD, reported at the annual congress of the European Society of Cardiology.
Those results stand in glaring contrast to the findings of the much-discussed SPRINT trial, in which hypertensive patients fared best with an on-treatment SBP driven below 120 mm Hg (N Engl J Med. 2015 Nov 26; 373:2103-16).
“Our trial findings don’t suggest that aggressive SBP lowering below 120 mm Hg is required in our specific population,” according to Dr. Lonn, professor of medicine and director of the vascular research ultrasound laboratory, Population Health Research Institute at McMaster University in Hamilton, Ont.“Please note that lower blood pressures, both systolic and diastolic, weren’t associated with lower risk, whereas higher blood pressures considerably increased the risk for major vascular events,” she added.
HOPE-3 (the Third Heart Outcomes Prevention Evaluation) included 12,705 patients in 21 countries who did not have cardiovascular disease and were at intermediate risk, with an average age of 65 years at enrollment and a Framinhgam Risk Score of about 10%. They were randomized double-blind in a 2x2 factorial design to rosuvastatin at 10 mg per day or placebo and/or candesartan at 16 mg plus hydrochlorothiazide at 12.5 mg per day or placebo and prospectively followed for a median of 5.6 years.
The primary outcomes of HOPE-3 have been published (N Engl J Med. 2016 May 26;374[21]:2009-20 and 2021-31). This was a practice-changing trial that opened the door to broader use of statin therapy for primary prevention.
At the ESC congress in Barcelona, Dr. Lonn presented a secondary post-hoc analysis that focused on the impact of antihypertensive therapy in HOPE-3. The results shed new light on the optimal blood pressure levels for triggering initation of antihypertensive therapy, as well as defining the achieved blood pressures that resulted in the greatest reductions in major vascular events.
As this was essentially an all-comers trial of intermediate-risk patients, participants presented with a range of blood pressures at baseline. But more than 4,700 subjects had a baseline SBP of 140-159.9 mm Hg, and 833 had an SBP of 160 mm Hg or more.
The candesartan/hydrochlorothiazide regimen resulted in what Dr. Lonn termed a “moderate” net placebo-subtracted blood pressure reduction of 6/3 mm Hg. The higher the baseline blood pressure, the bigger the reduction.
In the one-third of subjects with a baseline SBP greater than 143.5 mm Hg, antihypertensive therapy resulted in a significant 27% reduction in the composite endpoint of cardiovascular death, MI, or stroke compared with placebo. Those with a baseline SBP of 150 mm Hg or more showed even greater benefit from antihypertensive therapy, with a composite event rate of 4.8% compared with 7.2% for placebo, representing a 34% relative risk reduction in which the event curves began separating at about 2 years.
In contrast, antihypertensive therapy brought no significant reduction in events in patients in the lower two tertiles of baseline SBP. And there was no association at all between baseline DBP and major cardiovascular events across the range of DBP values evaluated in HOPE-3.
But wait: Things get more interesting, according to the cardiac electrophysiologist.
“I find the association between mean in-trial blood pressure as recorded in many measurements and vascular outcomes to be the most interesting analysis. This may be a better look at the association between blood pressure and outcomes than a measurement obtained just once or twice at baseline,” she explained.
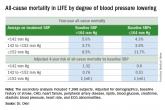
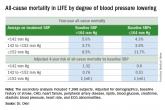
Of note, among the 6,356 subjects on candesartan/hydrochlorothiazide, those with a mean on-treatment SBP of 160 mm Hg or more had a 2.61% per year rate of the composite of cardiovascular death, MI, stroke, rescue from cardiac arrest, heart failure, or revascularization. This was more than three-fold higher than the 0.75% per year rate in patients with an on-treatment SBP of 120-139.9 mm Hg. The composite event rate was also significantly higher in those with a mean on-treatment SBP of 140-159.9 mm Hg, at 1.4% per year. The event rate in patients with an on-treatment SBP below 120 mm Hg was identical to that of patients with a value of 120-139.9 mm Hg.
Only among patients with an on-treatment DBP of 90 mm Hg or more was the composite event rate significantly greater than in those with a DBP of 70-79.9 mm Hg, who had the lowest event rate by a margin of 1.89% versus 0.75% per year.
An Australian cardiologist in the audience who has been involved in revamping hypertension treatment guidelines Down Under expressed frustration. He only recently succeeded in wrangling his fellow panelists into incorporating the SPRINT results into the draft guidelines; now HOPE-3 is sending a very different message. What gives? Could the disparate findings simply be due to play of chance? he asked.
Highly unlikely, Dr. Lonn replied.
“There were substantial differences between our trials,” she explained. “First of all, the SPRINT population was at substantially higher risk. They either had to have established cardiovascular disease – we eliminated those people – or significant renal disease – we eliminated those people, too – or age greater than 75, or a Framingham Risk Score above 15%.”
Also, the SPRINT protocol controversially called for unattended blood pressure measurement.
“This is a very pure way ot eliminating white coat hypertension, but it is different from other studies, so it is very difficult to compare SPRINT to older studies or to HOPE-3. Some other investigators have suggested that the difference between attended and unattended blood pressure is close to 10 mm Hg. So our SBP of 130 mm Hg, which had the best outcomes in HOPE-3, may be the same as about 120 mm Hg in SPRINT,” according to Dr. Lonn.
HOPE-3 was funded by the Canadian Institutes of Health Research and AstraZeneca. Dr. Lonn reported serving as a consultant to and receiving research grants from AstraZeneca, Amgen, Bayer, and Novartis.
NEW ORLEANS – The SPRINT trial target of systolic blood pressure less than 120 mm Hg doesn’t apply to most hypertensive patients.
