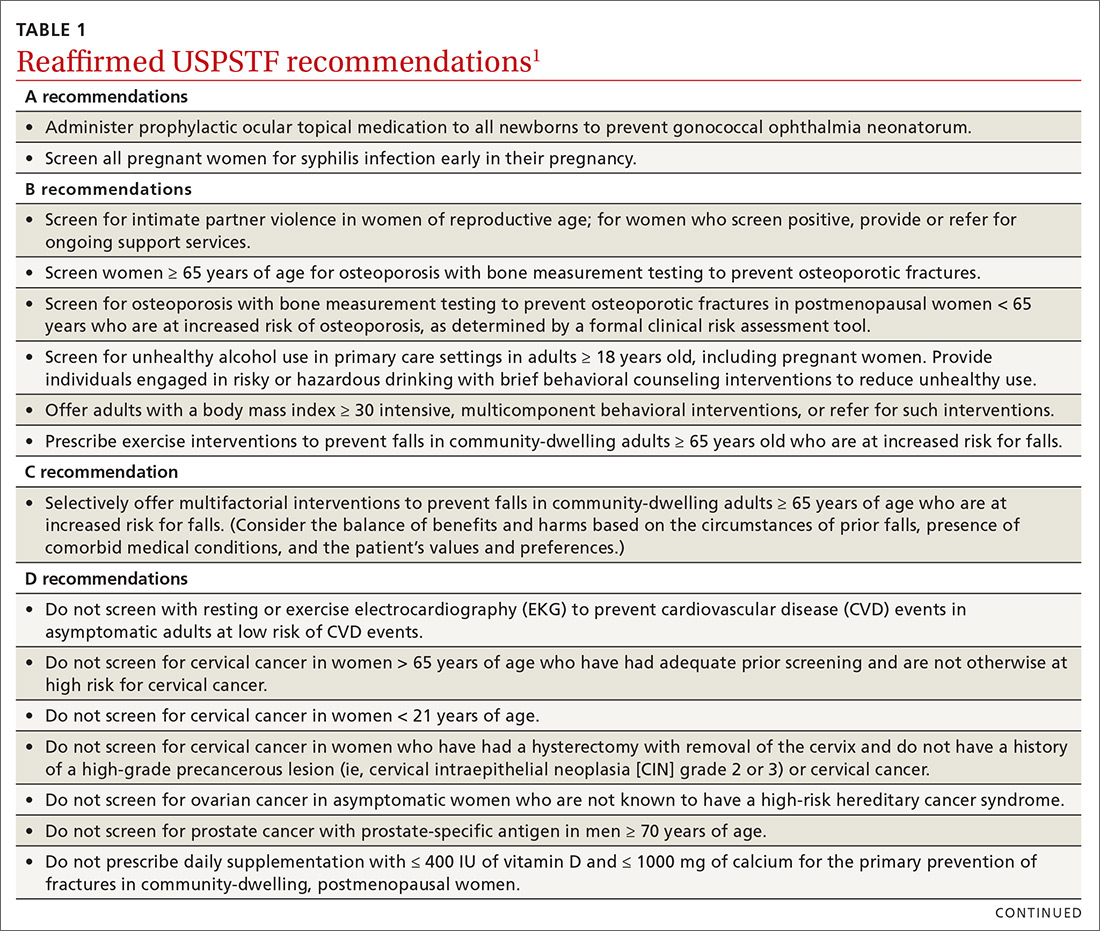
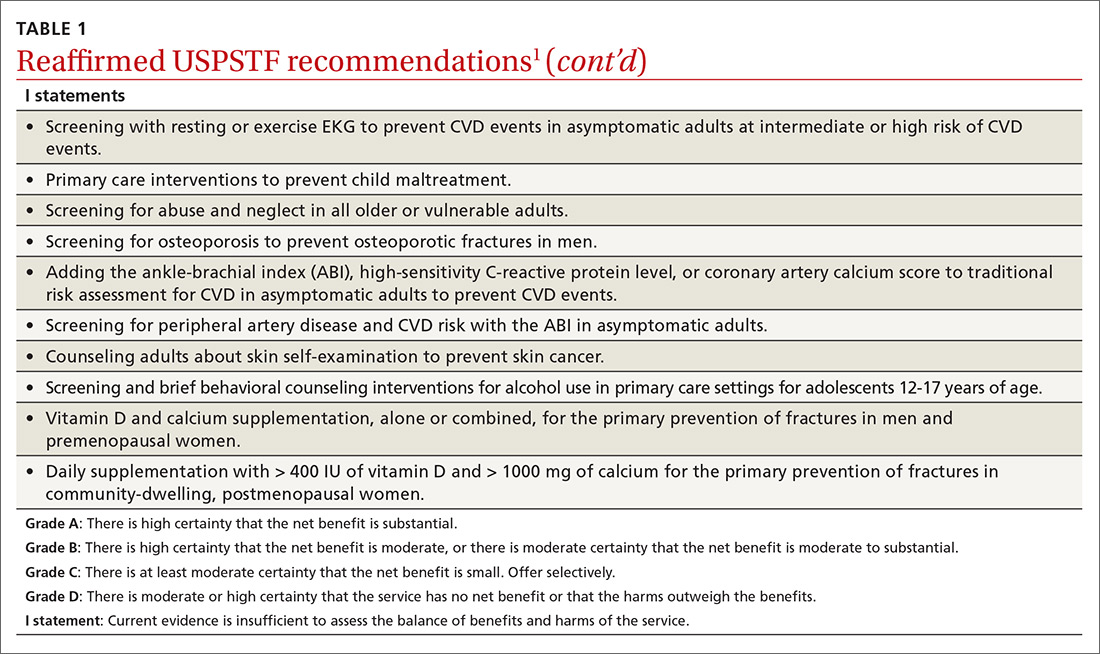
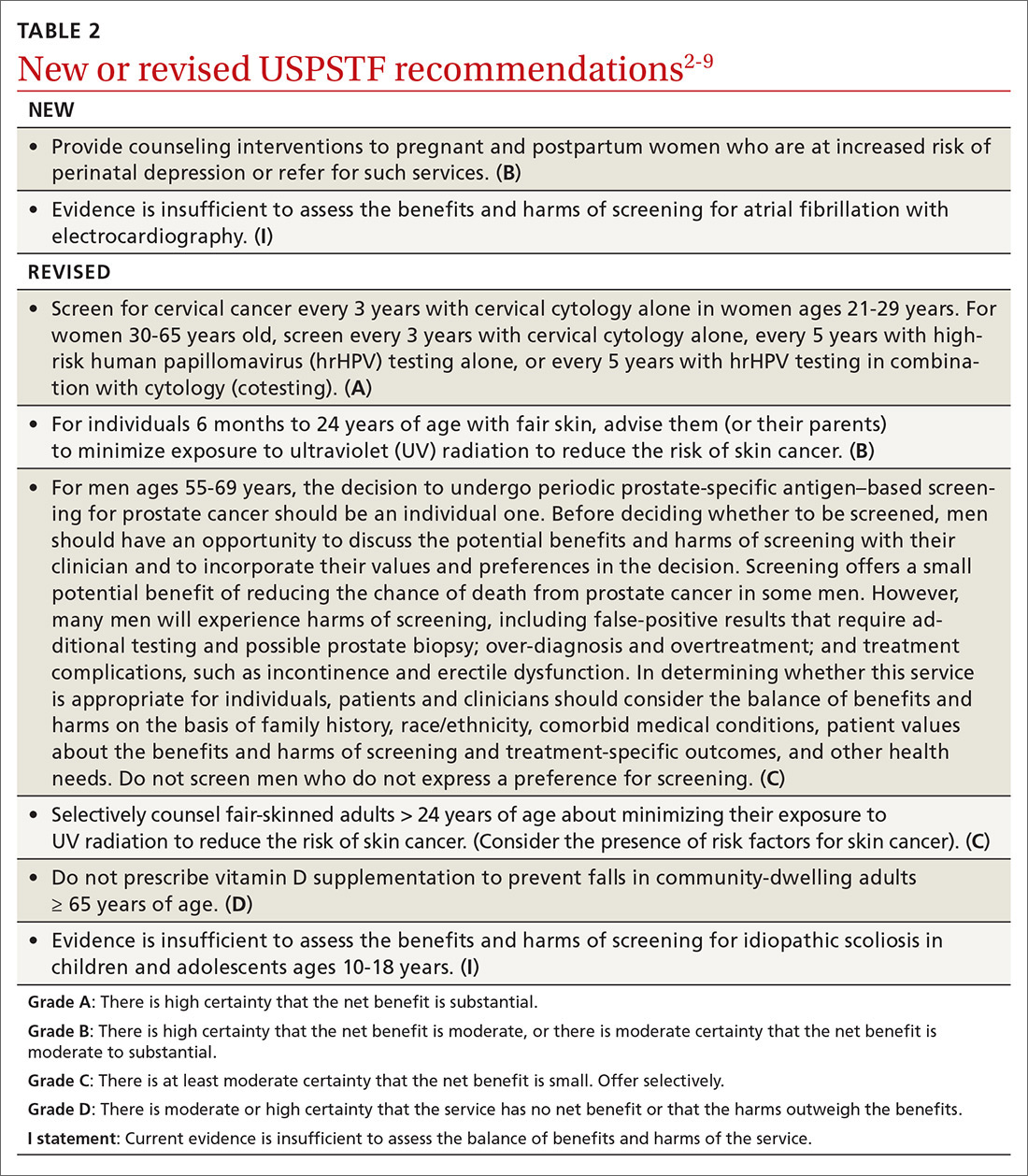
Over the past year through early 2019, the US Preventive Services Task Force made 34 recommendations on 19 different topics. Twenty-six were reaffirmations of recommendations made in previous years (TABLE 11); the Task Force attempts to reassess topics every 7 years. Two new topics were addressed with 2 new recommendations, and 6 previous recommendations were revised or reversed (TABLE 22-9).
This Practice Alert discusses the new and the changed recommendations. (In 2018, the Practice Alert podcast series covered screening for ovarian cancer [April], prostate cancer [June], and cervical cancer [October], and EKG screening for cardiovascular disease [November].) All current Task Force recommendations are available on the USPSTF Web site.1
New topics
Perinatal depression prevention
The Task Force recommends that clinicians counsel pregnant women and women in the first year postpartum who are at increased risk for perinatal depression, or refer for such services. The recommendation applies to those who are not diagnosed with depression but are at increased risk.
Perinatal depression can negatively affect both mother and child in several ways and occurs at a rate close to 9% during pregnancy and 37% during the first year postpartum.2 The interventions studied by the Task Force included cognitive behavioral therapy and interpersonal therapy; most sessions were initiated in the second trimester of pregnancy and varied in number of sessions and intensity. The Task Force includes the following in the list of risks that should prompt a referral: a history of depression, current depressive symptoms that fall short of that needed for a depression diagnosis, low income, adolescent or single parenthood, recent intimate partner violence, elevated anxiety symptoms, physical or sexual abuse, or a history of significant negative life events. (See “Postpartum anxiety: More common than you think,” in the April issue.)
Atrial fibrillation
The Task Force found insufficient evidence to recommend for or against the use of electrocardiography (EKG) to screen for atrial fibrillation (AF).3 Atrial fibrillation is common, affecting 3% of men and 2% of women between the ages of 65 and 69 years, and it increases in prevalence with age.4 It is a major risk factor for stroke, although it is commonly first diagnosed after a stroke. Treatment with anticoagulant therapy reduces the incidence of stroke in patients with symptomatic AF, but this treatment is associated with the risk of major bleeding. The problem in screening for AF with EKG is that it is associated with misdiagnosis, over-treatment, and further testing. The Task Force could not find any direct evidence of the totality of benefits and harms of screening asymptomatic adults with EKG, and it raised the possibility that benefit with less harm might be achieved by screening with pulse palpation and heart auscultation, followed by EKG testing of those with an irregular pulse.
Revisions of previous recommendations
Cervical cancer screening
The Task Force continues to recommend screening for cervical cancer in women 21 to 65 years of age.5 The major change in the current recommendation is for women ages 30 to 65 years. For this group, the Task Force now recommends screening every 5 years with high-risk human papillomavirus (hrHPV) testing alone as a possible alternative to screening every 3 years with cytology alone. They also halfheartedly endorse co-testing as an option, even though it may result in more tests and procedures compared with either cytology or hrHPV testing alone, with equal effectiveness. For women ages 21 to 29 years, cervical cytology alone every 3 years is still the only recommended regimen.
Skin cancer prevention
The Task Force made 2 revisions to the 2012 recommendation on preventing skin cancer through behavioral counseling to avoid ultraviolet (UV) radiation.6 These recommendations continue to focus on those with fair skin. The first revision: The earliest age at which children (through their guardians) can benefit from counseling on UV avoidance has been lowered from age 10 years to 6 months. The second revision: Some adults older than age 24 can also benefit from such counseling if they have fair skin and other skin cancer risks such as using tanning beds, having a history of sunburns or previous skin cancer, having an increased number of nevi (moles) and atypical nevi, having human immunodeficiency virus (HIV) infection, having received an organ transplant, or having a family history of skin cancer.
Continue to: Those at risk...