CHICAGO – Pelvic artery embolization is a highly effective technique for managing postpartum hemorrhage with the added advantage that it preserves the uterus and fertility, according to Dr. Ji Hoon Shin.
In a retrospective study of 225 women who underwent pelvic artery embolization (PAE) to stop postpartum hemorrhage (PPH), a single procedure stopped bleeding in 86% of women. A second procedure stopped bleeding in 89%.
"The major advantage of this procedure is that you can save the uterus and fertility," Dr. Shin said at the annual meeting of the Society for Interventional Radiology.
Standard therapies include fluid resuscitation/blood transfusion, management of the underlying cause, or surgery – uterine artery ligation, suturing, and hysterectomy.
PAE involves inserting a catheter into the femoral artery via a small incision in the groin. The interventional radiologist can then inject small particles or coils into the arteries to stem hemorrhage. Not only is the technique minimally invasive, it can save the uterus and preserve fertility. While the use of PAE was first reported in 1979, obstetrician awareness of this option remains limited.
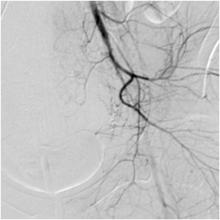
In this study, researchers identified 225 patients who underwent pulmonary artery embolization for PPH within 24 hours of delivery between 2000 and 2010. Technical success was defined as cessation of bleeding on postembolization angiogram and cessation of vaginal bleeding on physical inspection. Clinical success was defined as the cessation of bleeding following PAE without the need for additional surgery during the hospital stay.
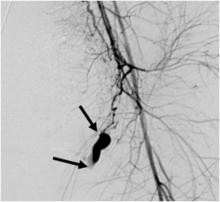
Uterine atony was the most common cause of PPH in this group (81%). Roughly a third (36%) of patients had positive angiographic findings. Contrast extravasation (a sign of acute bleeding) was seen in most patients (86%) and pseudoaneurysm occurred in 14% of patients, said Dr. Shin of the department of radiology at the University of Ulsan in Seoul, South Korea.
Technical success was 89%. Clinical success with only one PAE procedure was 86% and was 89% when women who had an additional PAE procedure were included. Overall bleeding control – including patients who had repeat PAEs and/or surgeries – was 98%.
In terms of safety, major complications occurred in 2% of patients and included puncture site hematoma and uterine artery dissection. Transient numbness – a minor complication – occurred in 1% of women.
In terms of fertility preservation, 97% of 113 women who were available for follow-up resumed regular menstruation. Irregular menses occurred in two women (2%), and early menopause occurred in one patient (1%). Notably, 11 patients (10%) were able to become pregnant.
On statistical analysis, the presence of disseminated intravascular coagulopathy was the most important negative prognostic factor.
Dr. Shin reported that he had no relevant financial disclosures.