Treatment has consisted of containment of the femoral head with the use of splints, although there is little evidence that this treatment alters outcomes.9,10 One study found conflicting evidence that it improved results and does not support its use.9 This is why having a pediatric orthopedist involved in these cases is important.
Long-term prognosis is closely related to the degree of involvement of the femoral head and to the age at onset. Those who are younger than 6 to 8 years typically have the best outcomes, with less hip pain and dysfunction later in life.9,10
SCFE, the most common hip disorder in adolescents, can be easily missed. SCFE has a strong correlation with obesity and is especially common in obese males between the ages of 10 and 16 years who have delayed secondary sex characteristics.2,11 SCFE is generally a mechanical disorder, but in children who are younger than 10 or have low weight or height for their age, an endocrine work-up is indicated.
Symptoms include a painful limp and nonspecific knee, anterior thigh, or groin pain. A delay in diagnosis has a significant effect on complications. Prognosis is also related to the stability of the slip.11,12 An unstable slip is defined as the inability to bear weight.13 The risk of osteonecrosis, a complication of SCFE, is negligible if the slip is stable, but may be as high as 50% when the slip is unstable.2
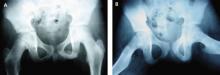
On examination, internal rotation is painful and limited, and flexion of the hip will lead to simultaneous external rotation. Leg length discrepancy or a positive Trendelenburg’s sign may be present. Diagnosis may be made with bilateral AP (FIGURES 2A AND 2B) and frog lateral radiographic views, looking for growth plate widening.12 Klein’s line—the line that would intersect the epiphysis when drawn along the anterior neck of the femur of an AP view of a normal hip13—is abnormal in a hip with SCFE.
CT or MRI can be performed in patients who have clinical evidence of SCFE but normal radiographs. Treatment is the same regardless of whether the slip is stable or unstable—patients are told to avoid weight bearing and are sent to an orthopedist. Stabilization with in situ pinning is the gold standard, regardless of severity.9,10,12
CASE AP x-rays of Sean’s right hip are abnormal, showing that the femoral epiphysis is not aligned with the femoral neck correctly when compared with the opposite side. You advise the patient and his parents that he has a serious condition called SCFE, which can lead to long-term problems if not treated surgically. You recommend that he start using crutches and remain fully non-weight bearing on his right leg, and refer him to a pediatric orthopedist.
FIGURE 2
Bilateral AP views reveal slipped capital femoral epiphysis
X-rays show the pelvic widening of the physis on the right (A) and the epiphysis slipping posteriorly and inferiorly (B).
Suspect these hip disorders in young athletes
Femoral stress fractures are particularly common in adolescents who are runners or endurance athletes. The classic history is gradual onset of anterior thigh pain, beginning during physical activity and progressing to pain at rest. Risk factors for femoral stress fractures include the female athlete triad (amenorrhea, eating disorder, and osteoporosis), a recent change in training, poor biomechanics, and underlying bone or metabolic disease.14
A positive hop test. The physical exam in a patient with a femoral stress fracture is likely to be normal, with the possible exception of limitation in hip ROM at the extremes. Pain may be reproduced with hopping (a positive result) on the affected leg; 1 study noted that 70% of patients with femoral stress fractures had a positive hop test.15
Hip radiographs should be done, but may not be helpful. In initial x-rays, sensitivity may be as low as 15%; delayed x-rays, taken 2 to 4 weeks later, have a sensitivity of about 50% for findings suggestive of a stress fracture.16
Although bone scan and MRI have approximately equal sensitivity, bone scan is less specific for detecting early stress fractures, so MRI has become the gold standard for diagnosing femoral stress fractures.14 Treatment depends on the location of the fracture. A compression stress fracture on the inferior surface of the femoral neck has a good prognosis when the patient remains non-weight bearing for 6 to 8 weeks, then gradually returns to activity.14
Tension stress fractures are on the superior surface, and patients need to be sent to an orthopedist for internal fixation.14,16 A tension-sided fracture can progress to non-union or avascular necrosis. Training and diet should be modified as indicated to promote healing and prevent recurrence.