HOUSTON – Asthmatic smokers who switched to electronic cigarettes showed evidence suggestive of respiratory harm reversal in a retrospective pilot study.
“Electronic cigarette use improves respiratory physiology and subjective asthma outcomes in asthmatic smokers. E-cigarettes are a safer alternative to conventional cigarettes in this vulnerable population,” Dr. Cristina Russo declared at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
She said that her small retrospective study is the first to examine the respiratory health impact of a switch to e-cigarettes by asthmatic smokers.
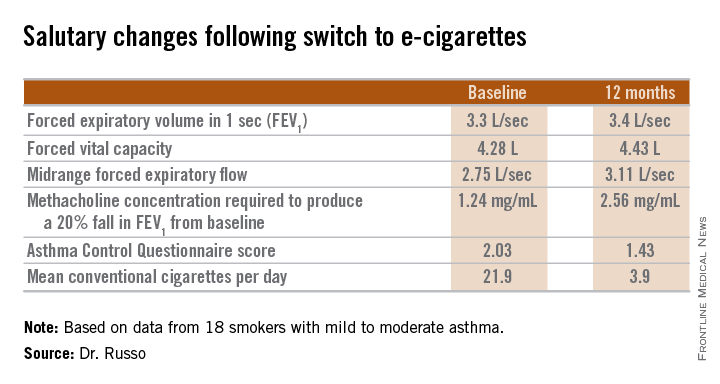
Every one of the objective and subjective measures of asthma status evaluated in the study showed statistically significant improvement 1 year after patients adopted e-cigarettes, and the e-cigarette users’ consumption of conventional cigarettes dropped precipitously, reported Dr. Russo of the University of Catania (Italy).
She and her colleagues in the university asthma clinic have taken to suggesting the use of battery-powered e-cigarettes to their asthmatic smokers who haven’t benefited from or aren’t interested in trying the more conventional approaches to smoking cessation or reduction, including medications. While abstinence from cigarette smoking is best, the available evidence indicates e-cigarettes are at least 95% less harmful than conventional cigarettes in the general population, she said.
The study included 18 smokers with mild to moderate asthma who switched to e-cigarettes and underwent spirometry and other testing at baseline and 6 and 12 months of follow-up. Ten patients switched over to e-cigarettes exclusively, while the other 8 used both conventional and e-cigarettes.
Among the highlights: The mid-range forced expiratory flow (25%-75%) showed a major, clinically important improvement, increasing from 2.75 L/sec to 3.11 L/sec. And patients’ mean self-reported conventional cigarette consumption dropped from 21.9 per day at baseline to 5 at 6 months and 3.9 per day at 12 months.
Among the group at large, no significant change was seen in the frequency of asthma exacerbations resulting in hospitalization. However, among the frequent exacerbators – the six patients with two or more exacerbations during the 6 months prior to baseline – exacerbation frequency was cut in half both 6 and 12 months following the switch to e-cigarettes.
Dr. Russo’s presentation sparked vigorous audience discussion. Several physicians cited a Centers for Disease Control and Prevention warning about the unknowns regarding e-cigarette safety, and one allergist declared he didn’t think physicians should ever encourage patients to smoke anything. But others defended the “lesser of two evils” approach adopted by Dr. Russo and coworkers.
Dr. Russo noted that the prevalence of smoking among asthma patients is similar to that of the general population. She called smoking and asthma “a dangerous liaison.” Smoking accelerates asthma patients’ decline in lung function, worsens persistent airways obstruction, and increases insensitivity to corticosteroids.
Her study was supported by a university grant and the Italian League Against Smoking. She reported having no financial conflicts.