User login
HCV Hub
AbbVie
acid
addicted
addiction
adolescent
adult sites
Advocacy
advocacy
agitated states
AJO, postsurgical analgesic, knee, replacement, surgery
alcohol
amphetamine
androgen
antibody
apple cider vinegar
assistance
Assistance
association
at home
attorney
audit
ayurvedic
baby
ban
baricitinib
bed bugs
best
bible
bisexual
black
bleach
blog
bulimia nervosa
buy
cannabis
certificate
certification
certified
cervical cancer, concurrent chemoradiotherapy, intravoxel incoherent motion magnetic resonance imaging, MRI, IVIM, diffusion-weighted MRI, DWI
charlie sheen
cheap
cheapest
child
childhood
childlike
children
chronic fatigue syndrome
Cladribine Tablets
cocaine
cock
combination therapies, synergistic antitumor efficacy, pertuzumab, trastuzumab, ipilimumab, nivolumab, palbociclib, letrozole, lapatinib, docetaxel, trametinib, dabrafenib, carflzomib, lenalidomide
contagious
Cortical Lesions
cream
creams
crime
criminal
cure
dangerous
dangers
dasabuvir
Dasabuvir
dead
deadly
death
dementia
dependence
dependent
depression
dermatillomania
die
diet
direct-acting antivirals
Disability
Discount
discount
dog
drink
drug abuse
drug-induced
dying
eastern medicine
eat
ect
eczema
electroconvulsive therapy
electromagnetic therapy
electrotherapy
epa
epilepsy
erectile dysfunction
explosive disorder
fake
Fake-ovir
fatal
fatalities
fatality
fibromyalgia
financial
Financial
fish oil
food
foods
foundation
free
Gabriel Pardo
gaston
general hospital
genetic
geriatric
Giancarlo Comi
gilead
Gilead
glaucoma
Glenn S. Williams
Glenn Williams
Gloria Dalla Costa
gonorrhea
Greedy
greedy
guns
hallucinations
harvoni
Harvoni
herbal
herbs
heroin
herpes
Hidradenitis Suppurativa,
holistic
home
home remedies
home remedy
homeopathic
homeopathy
hydrocortisone
ice
image
images
job
kid
kids
kill
killer
laser
lawsuit
lawyer
ledipasvir
Ledipasvir
lesbian
lesions
lights
liver
lupus
marijuana
melancholic
memory loss
menopausal
mental retardation
military
milk
moisturizers
monoamine oxidase inhibitor drugs
MRI
MS
murder
national
natural
natural cure
natural cures
natural medications
natural medicine
natural medicines
natural remedies
natural remedy
natural treatment
natural treatments
naturally
Needy
needy
Neurology Reviews
neuropathic
nightclub massacre
nightclub shooting
nude
nudity
nutraceuticals
OASIS
oasis
off label
ombitasvir
Ombitasvir
ombitasvir/paritaprevir/ritonavir with dasabuvir
orlando shooting
overactive thyroid gland
overdose
overdosed
Paolo Preziosa
paritaprevir
Paritaprevir
pediatric
pedophile
photo
photos
picture
post partum
postnatal
pregnancy
pregnant
prenatal
prepartum
prison
program
Program
Protest
protest
psychedelics
pulse nightclub
puppy
purchase
purchasing
rape
recall
recreational drug
Rehabilitation
Retinal Measurements
retrograde ejaculation
risperdal
ritonavir
Ritonavir
ritonavir with dasabuvir
robin williams
sales
sasquatch
schizophrenia
seizure
seizures
sex
sexual
sexy
shock treatment
silver
sleep disorders
smoking
sociopath
sofosbuvir
Sofosbuvir
sovaldi
ssri
store
sue
suicidal
suicide
supplements
support
Support
Support Path
teen
teenage
teenagers
Telerehabilitation
testosterone
Th17
Th17:FoxP3+Treg cell ratio
Th22
toxic
toxin
tragedy
treatment resistant
V Pak
vagina
velpatasvir
Viekira Pa
Viekira Pak
viekira pak
violence
virgin
vitamin
VPak
weight loss
withdrawal
wrinkles
xxx
young adult
young adults
zoloft
financial
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
New antivirals, more screening could slash hepatitis C cases
Hepatitis C could be reduced by 90% or more in the United States by the year 2040 with the use of direct-acting antivirals, near-universal screening, and enhanced treatment capacity, according to a study in Clinical Infectious Diseases.
A research team led by Jeffrey Townsend, Ph.D., of Yale School of Public Health, New Haven, Conn., said that new direct-acting antivirals (DAAs) alone could reduce the prevalence of hepatitis C virus (HCV) by 80% by the year 2040. When near-universal screening and enhanced treatment capacity are added to the equation, HCV could be eliminated in the United States, though cost and reimbursement issues may impede implementation.
“The key finding is that a fourfold increase to the number of patients treated each year could virtually eliminate HCV from the noninjecting population within a decade,” said Dr. Townsend, senior author of the study, in a statement accompanying the study [Clin Infect Dis. 2015. doi: 10.1093/cid/civ894].
First author David Durham, Ph.D., also of the Yale School of Public Health, and his collaborators analyzed currently available data and constructed a sophisticated model to generate projections of how future DAA treatment will change HCV prevalence. Dr. Durham and his colleagues also built models to account for varying levels of screening in the general population and for people who inject drugs (PWIDs).
More than 5 million people with chronic hepatitis C infection are thought to live in the United States, and just about 100,000 of those currently receive treatment each year. The treatment burden and relatively low cure rate of interferon-based therapies have historically been significant impediments for many patients. New DAAs promise a sustained virologic response (SVR) in up to 95% of patients with a well-tolerated, once-daily, one-pill several-week regimen.
Without enhanced screening or treatment rates, the model predicted an 80% decline in U.S. HCV prevalence by the year 2040. The 80% benchmark would be reached by the year 2025 if the annual treatment rate increased to 400,000, with 256,315 fewer HCV-related deaths through 2040. Just doubling the treatment rate to 200,000 patients per year would result in an 80% decrease in HCV prevalence by 2031, with 143,055 fewer deaths by 2040.
However, “more than half of those with chronic HCV are unaware of their status, including up to two-thirds of people who inject drugs,” wrote Dr. Durham and his coauthors. Therefore, enhanced HCV screening, especially among PWIDs, could provide a significant further reduction in morbidity and mortality from HCV.
Targeted screening of PWIDs to achieve a 20% screening rate (compared with the current 4.1%), combined with a treatment rate of at least 30%, would yield a 90% reduction of prevalence in HCV by 2040. Universal screening, combined with a treatment rate of at least 20%, would achieve a 90% reduction in the incidence of new infections by 2040, according to the model.
The drop in prevalence in the models took into account not only an increased SVR rate, but also the reduced transmission rate when more persons with HCV achieve an SVR. This dynamic transmission analysis “captures the impact of treatment on both chronic disease and transmission dynamics, distinguishes screening and treatment as separate but related public health objectives, and accounts for underreporting … of national HCV prevalence,” according to Dr. Durham and his coauthors.
Morbidity and mortality were accounted for by projecting the number of HCV patients in each treatment and screening condition who would spontaneously clear disease, become chronically infected, develop increasing levels of liver disease and cirrhosis, require transplant, become reinfected, or die.
As always, real world considerations temper what’s achievable. For DAAs, a chief factor is the cost of the regimens, which currently hovers around $90,000. “The improvement of health outcomes expected from greater acceptance might be tempered by the high costs of treatment and by limited insurance coverage and willingness to treat PWIDs,” Dr. Durham and his coauthors wrote.
Study limitations included some “simplifying assumptions” in the modeling, which did not account for the varying incidence of fibrosis and transmissibility among different HCV genotypes. Still, wrote Dr. Durham and his collaborators, “our analysis provides a forecast for the potential impact of DAAs in reducing HCV-associated liver disease, demonstrating that achievable expansion of HCV treatment at current screening rates can substantially reduce morbidity and mortality.”
The study was funded by the Notsew Orm Sands Foundation and Merck. Dr. Durham, Dr. Galvani, and Dr. Townsend have consulted for and received research funding from Sanofi Pasteur and Merck. Dr. Elbasha is employed by Merck and holds stock and stock options in the company. The other authors reported no conflicts of interest.
On Twitter @karioakes
Hepatitis C could be reduced by 90% or more in the United States by the year 2040 with the use of direct-acting antivirals, near-universal screening, and enhanced treatment capacity, according to a study in Clinical Infectious Diseases.
A research team led by Jeffrey Townsend, Ph.D., of Yale School of Public Health, New Haven, Conn., said that new direct-acting antivirals (DAAs) alone could reduce the prevalence of hepatitis C virus (HCV) by 80% by the year 2040. When near-universal screening and enhanced treatment capacity are added to the equation, HCV could be eliminated in the United States, though cost and reimbursement issues may impede implementation.
“The key finding is that a fourfold increase to the number of patients treated each year could virtually eliminate HCV from the noninjecting population within a decade,” said Dr. Townsend, senior author of the study, in a statement accompanying the study [Clin Infect Dis. 2015. doi: 10.1093/cid/civ894].
First author David Durham, Ph.D., also of the Yale School of Public Health, and his collaborators analyzed currently available data and constructed a sophisticated model to generate projections of how future DAA treatment will change HCV prevalence. Dr. Durham and his colleagues also built models to account for varying levels of screening in the general population and for people who inject drugs (PWIDs).
More than 5 million people with chronic hepatitis C infection are thought to live in the United States, and just about 100,000 of those currently receive treatment each year. The treatment burden and relatively low cure rate of interferon-based therapies have historically been significant impediments for many patients. New DAAs promise a sustained virologic response (SVR) in up to 95% of patients with a well-tolerated, once-daily, one-pill several-week regimen.
Without enhanced screening or treatment rates, the model predicted an 80% decline in U.S. HCV prevalence by the year 2040. The 80% benchmark would be reached by the year 2025 if the annual treatment rate increased to 400,000, with 256,315 fewer HCV-related deaths through 2040. Just doubling the treatment rate to 200,000 patients per year would result in an 80% decrease in HCV prevalence by 2031, with 143,055 fewer deaths by 2040.
However, “more than half of those with chronic HCV are unaware of their status, including up to two-thirds of people who inject drugs,” wrote Dr. Durham and his coauthors. Therefore, enhanced HCV screening, especially among PWIDs, could provide a significant further reduction in morbidity and mortality from HCV.
Targeted screening of PWIDs to achieve a 20% screening rate (compared with the current 4.1%), combined with a treatment rate of at least 30%, would yield a 90% reduction of prevalence in HCV by 2040. Universal screening, combined with a treatment rate of at least 20%, would achieve a 90% reduction in the incidence of new infections by 2040, according to the model.
The drop in prevalence in the models took into account not only an increased SVR rate, but also the reduced transmission rate when more persons with HCV achieve an SVR. This dynamic transmission analysis “captures the impact of treatment on both chronic disease and transmission dynamics, distinguishes screening and treatment as separate but related public health objectives, and accounts for underreporting … of national HCV prevalence,” according to Dr. Durham and his coauthors.
Morbidity and mortality were accounted for by projecting the number of HCV patients in each treatment and screening condition who would spontaneously clear disease, become chronically infected, develop increasing levels of liver disease and cirrhosis, require transplant, become reinfected, or die.
As always, real world considerations temper what’s achievable. For DAAs, a chief factor is the cost of the regimens, which currently hovers around $90,000. “The improvement of health outcomes expected from greater acceptance might be tempered by the high costs of treatment and by limited insurance coverage and willingness to treat PWIDs,” Dr. Durham and his coauthors wrote.
Study limitations included some “simplifying assumptions” in the modeling, which did not account for the varying incidence of fibrosis and transmissibility among different HCV genotypes. Still, wrote Dr. Durham and his collaborators, “our analysis provides a forecast for the potential impact of DAAs in reducing HCV-associated liver disease, demonstrating that achievable expansion of HCV treatment at current screening rates can substantially reduce morbidity and mortality.”
The study was funded by the Notsew Orm Sands Foundation and Merck. Dr. Durham, Dr. Galvani, and Dr. Townsend have consulted for and received research funding from Sanofi Pasteur and Merck. Dr. Elbasha is employed by Merck and holds stock and stock options in the company. The other authors reported no conflicts of interest.
On Twitter @karioakes
Hepatitis C could be reduced by 90% or more in the United States by the year 2040 with the use of direct-acting antivirals, near-universal screening, and enhanced treatment capacity, according to a study in Clinical Infectious Diseases.
A research team led by Jeffrey Townsend, Ph.D., of Yale School of Public Health, New Haven, Conn., said that new direct-acting antivirals (DAAs) alone could reduce the prevalence of hepatitis C virus (HCV) by 80% by the year 2040. When near-universal screening and enhanced treatment capacity are added to the equation, HCV could be eliminated in the United States, though cost and reimbursement issues may impede implementation.
“The key finding is that a fourfold increase to the number of patients treated each year could virtually eliminate HCV from the noninjecting population within a decade,” said Dr. Townsend, senior author of the study, in a statement accompanying the study [Clin Infect Dis. 2015. doi: 10.1093/cid/civ894].
First author David Durham, Ph.D., also of the Yale School of Public Health, and his collaborators analyzed currently available data and constructed a sophisticated model to generate projections of how future DAA treatment will change HCV prevalence. Dr. Durham and his colleagues also built models to account for varying levels of screening in the general population and for people who inject drugs (PWIDs).
More than 5 million people with chronic hepatitis C infection are thought to live in the United States, and just about 100,000 of those currently receive treatment each year. The treatment burden and relatively low cure rate of interferon-based therapies have historically been significant impediments for many patients. New DAAs promise a sustained virologic response (SVR) in up to 95% of patients with a well-tolerated, once-daily, one-pill several-week regimen.
Without enhanced screening or treatment rates, the model predicted an 80% decline in U.S. HCV prevalence by the year 2040. The 80% benchmark would be reached by the year 2025 if the annual treatment rate increased to 400,000, with 256,315 fewer HCV-related deaths through 2040. Just doubling the treatment rate to 200,000 patients per year would result in an 80% decrease in HCV prevalence by 2031, with 143,055 fewer deaths by 2040.
However, “more than half of those with chronic HCV are unaware of their status, including up to two-thirds of people who inject drugs,” wrote Dr. Durham and his coauthors. Therefore, enhanced HCV screening, especially among PWIDs, could provide a significant further reduction in morbidity and mortality from HCV.
Targeted screening of PWIDs to achieve a 20% screening rate (compared with the current 4.1%), combined with a treatment rate of at least 30%, would yield a 90% reduction of prevalence in HCV by 2040. Universal screening, combined with a treatment rate of at least 20%, would achieve a 90% reduction in the incidence of new infections by 2040, according to the model.
The drop in prevalence in the models took into account not only an increased SVR rate, but also the reduced transmission rate when more persons with HCV achieve an SVR. This dynamic transmission analysis “captures the impact of treatment on both chronic disease and transmission dynamics, distinguishes screening and treatment as separate but related public health objectives, and accounts for underreporting … of national HCV prevalence,” according to Dr. Durham and his coauthors.
Morbidity and mortality were accounted for by projecting the number of HCV patients in each treatment and screening condition who would spontaneously clear disease, become chronically infected, develop increasing levels of liver disease and cirrhosis, require transplant, become reinfected, or die.
As always, real world considerations temper what’s achievable. For DAAs, a chief factor is the cost of the regimens, which currently hovers around $90,000. “The improvement of health outcomes expected from greater acceptance might be tempered by the high costs of treatment and by limited insurance coverage and willingness to treat PWIDs,” Dr. Durham and his coauthors wrote.
Study limitations included some “simplifying assumptions” in the modeling, which did not account for the varying incidence of fibrosis and transmissibility among different HCV genotypes. Still, wrote Dr. Durham and his collaborators, “our analysis provides a forecast for the potential impact of DAAs in reducing HCV-associated liver disease, demonstrating that achievable expansion of HCV treatment at current screening rates can substantially reduce morbidity and mortality.”
The study was funded by the Notsew Orm Sands Foundation and Merck. Dr. Durham, Dr. Galvani, and Dr. Townsend have consulted for and received research funding from Sanofi Pasteur and Merck. Dr. Elbasha is employed by Merck and holds stock and stock options in the company. The other authors reported no conflicts of interest.
On Twitter @karioakes
FROM CLINICAL INFECTIOUS DISEASES
Key clinical point: Hepatitis C could be reduced by 90% or more in the United States by the year 2040 with the use of direct-acting antivirals, near-universal screening, and enhanced treatment capacity.
Major finding: Targeted screening of 20% of persons who inject drugs, combined with a 30% treatment rate, would reduce HCV prevalence by 90% by the year 2040.
Data source: Dynamic modeling of HCV prevalence, screening, and treatment, using currently available data to model public health scenarios to the year 2040.
Disclosures: The study was funded by the Notsew Orm Sands Foundation and Merck. Dr. Durham, Dr. Galvani, and Dr. Townsend have consulted for and received research funding from Sanofi Pasteur and Merck. Dr. Elbasha is employed by Merck and holds stock and stock options in the company. The other authors reported no conflicts of interest.
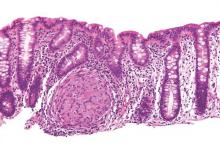
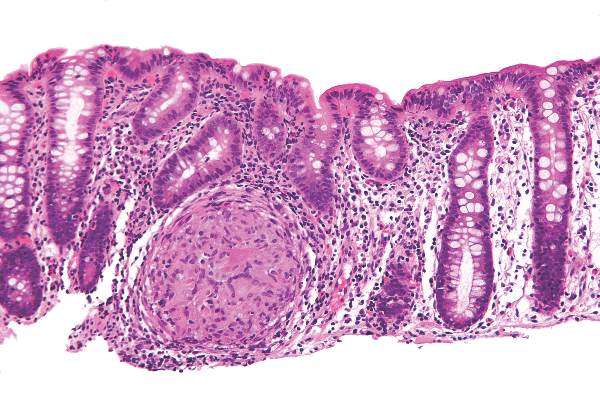
Crohn’s study found no reason to continue immunomodulators after starting anti-TNFs
Baseline exposure to an immunomodulator did not improve the odds of clinical response or remission when starting anti–tumor necrosis factor (anti-TNF) therapy for Crohn’s disease (CD), said authors of a meta-analysis of 11 randomized, controlled trials. Pending better trials, patients with CD and their clinicians will need to carefully weigh the risks and benefits of continuing an immunomodulator when starting anti-TNF therapy, Dr. Jennifer Jones of Dalhousie University in Halifax, Canada and her associates wrote in the December issue of Clinical Gastroenterology and Hepatology.
Intense debate persists about whether patients with CD who have already been exposed to immunomodulators such as azathioprine, 6-mercaptopurine, and methotrexate should stay on them when starting anti-TNF agents. The landmark 2010 SONIC trial could not answer this question because it only enrolled patients who had never received an immunomodulator, and more recent studies (Clin Gastroenterol Hepatol. 2011;9:36-41) have raised concerns about the safety of immunomodulators, the researchers noted. To compare combination immunomodulators and anti-TNF treatment with anti-TNF monotherapy in luminal and fistulizing CD, they analyzed original datasets from 11 randomized, controlled trials published between 1980 and 2008. A total of 625 patients with CD had received an immunomodulator, while 976 patients had not. The investigators excluded trials in which patients were naive to both immunomodulators and anti-TNF agents (Clin Gastroenterol Hepatol. 2015 [doi: 10.1016/j.cgh.2015.06.034]).
In the overall analysis, combination therapy was no better than anti-TNF monotherapy in terms of 6-month remission, maintenance of response, or partial or full fistula closure, Dr. Jones and her associates reported. The same was true for subgroup analyses, but the odds ratio for infliximab reached statistical significance in a sensitivity analysis that included data from the ACCENT 2 (Clin Gastroenterol Hepatol. 2004;2:912-20) trial. “For the infliximab-only analysis, adding ACCENT 2 resulted in minimal change in the point estimate but, as expected, increased the precision of the 95% CIs (the lower CI increased from 0.97 to 1.06), which led to a statistically significant difference in the comparison between infliximab monotherapy and combination therapy,” the researchers commented. While sensitivity analyses have limitations, the finding “does raise the question” of whether the benefits of staying on an immunomodulator depend on the anti-TNF agent, they said.
Combination therapy did not heighten the chances of infusion reactions, malignancies, serious infections, or death, said the investigators. In fact, baseline immunomodulator exposure was associated with fewer injection site reactions among infliximab patients (OR, 0.46; 95% CI, 0.26-0.79). The researchers did not uncover publication bias, and found significant heterogeneity among studies only for the 6-month clinical response endpoint, they added.
The findings “challenge the clinical importance of combination therapy” in the setting of baseline immunomodulator exposure, but “it is hard to ignore the preponderance of data” on anti-TNF pharmacokinetics that support combination therapy over monotherapy, the investigators emphasized. “Whether combination therapy has a greater protective effect against anti-drug antibody development and lower trough levels for all anti-TNF agents or for patients previously exposed to anti-TNF agents is still in question,” they added. They called for a well-designed, randomized, placebo-controlled trial that uses objective measures of disease activity and follow patients long enough to assess efficacy.
The investigators reported no funding sources for the study. Dr. Jones reported having been a speaker for Jansen, Merck, Schering-Plough, Abbott, and AbbVie, and having served on advisory boards for Janssen, Abbott, and Takeda. Nine co-authors reported financial and consulting relationships with Jansen, Merck, Schering-Plough, Abbott, and a number of other pharmaceutical companies.
Source: American Gastroenterological Association
Baseline exposure to an immunomodulator did not improve the odds of clinical response or remission when starting anti–tumor necrosis factor (anti-TNF) therapy for Crohn’s disease (CD), said authors of a meta-analysis of 11 randomized, controlled trials. Pending better trials, patients with CD and their clinicians will need to carefully weigh the risks and benefits of continuing an immunomodulator when starting anti-TNF therapy, Dr. Jennifer Jones of Dalhousie University in Halifax, Canada and her associates wrote in the December issue of Clinical Gastroenterology and Hepatology.
Intense debate persists about whether patients with CD who have already been exposed to immunomodulators such as azathioprine, 6-mercaptopurine, and methotrexate should stay on them when starting anti-TNF agents. The landmark 2010 SONIC trial could not answer this question because it only enrolled patients who had never received an immunomodulator, and more recent studies (Clin Gastroenterol Hepatol. 2011;9:36-41) have raised concerns about the safety of immunomodulators, the researchers noted. To compare combination immunomodulators and anti-TNF treatment with anti-TNF monotherapy in luminal and fistulizing CD, they analyzed original datasets from 11 randomized, controlled trials published between 1980 and 2008. A total of 625 patients with CD had received an immunomodulator, while 976 patients had not. The investigators excluded trials in which patients were naive to both immunomodulators and anti-TNF agents (Clin Gastroenterol Hepatol. 2015 [doi: 10.1016/j.cgh.2015.06.034]).
In the overall analysis, combination therapy was no better than anti-TNF monotherapy in terms of 6-month remission, maintenance of response, or partial or full fistula closure, Dr. Jones and her associates reported. The same was true for subgroup analyses, but the odds ratio for infliximab reached statistical significance in a sensitivity analysis that included data from the ACCENT 2 (Clin Gastroenterol Hepatol. 2004;2:912-20) trial. “For the infliximab-only analysis, adding ACCENT 2 resulted in minimal change in the point estimate but, as expected, increased the precision of the 95% CIs (the lower CI increased from 0.97 to 1.06), which led to a statistically significant difference in the comparison between infliximab monotherapy and combination therapy,” the researchers commented. While sensitivity analyses have limitations, the finding “does raise the question” of whether the benefits of staying on an immunomodulator depend on the anti-TNF agent, they said.
Combination therapy did not heighten the chances of infusion reactions, malignancies, serious infections, or death, said the investigators. In fact, baseline immunomodulator exposure was associated with fewer injection site reactions among infliximab patients (OR, 0.46; 95% CI, 0.26-0.79). The researchers did not uncover publication bias, and found significant heterogeneity among studies only for the 6-month clinical response endpoint, they added.
The findings “challenge the clinical importance of combination therapy” in the setting of baseline immunomodulator exposure, but “it is hard to ignore the preponderance of data” on anti-TNF pharmacokinetics that support combination therapy over monotherapy, the investigators emphasized. “Whether combination therapy has a greater protective effect against anti-drug antibody development and lower trough levels for all anti-TNF agents or for patients previously exposed to anti-TNF agents is still in question,” they added. They called for a well-designed, randomized, placebo-controlled trial that uses objective measures of disease activity and follow patients long enough to assess efficacy.
The investigators reported no funding sources for the study. Dr. Jones reported having been a speaker for Jansen, Merck, Schering-Plough, Abbott, and AbbVie, and having served on advisory boards for Janssen, Abbott, and Takeda. Nine co-authors reported financial and consulting relationships with Jansen, Merck, Schering-Plough, Abbott, and a number of other pharmaceutical companies.
Source: American Gastroenterological Association
Baseline exposure to an immunomodulator did not improve the odds of clinical response or remission when starting anti–tumor necrosis factor (anti-TNF) therapy for Crohn’s disease (CD), said authors of a meta-analysis of 11 randomized, controlled trials. Pending better trials, patients with CD and their clinicians will need to carefully weigh the risks and benefits of continuing an immunomodulator when starting anti-TNF therapy, Dr. Jennifer Jones of Dalhousie University in Halifax, Canada and her associates wrote in the December issue of Clinical Gastroenterology and Hepatology.
Intense debate persists about whether patients with CD who have already been exposed to immunomodulators such as azathioprine, 6-mercaptopurine, and methotrexate should stay on them when starting anti-TNF agents. The landmark 2010 SONIC trial could not answer this question because it only enrolled patients who had never received an immunomodulator, and more recent studies (Clin Gastroenterol Hepatol. 2011;9:36-41) have raised concerns about the safety of immunomodulators, the researchers noted. To compare combination immunomodulators and anti-TNF treatment with anti-TNF monotherapy in luminal and fistulizing CD, they analyzed original datasets from 11 randomized, controlled trials published between 1980 and 2008. A total of 625 patients with CD had received an immunomodulator, while 976 patients had not. The investigators excluded trials in which patients were naive to both immunomodulators and anti-TNF agents (Clin Gastroenterol Hepatol. 2015 [doi: 10.1016/j.cgh.2015.06.034]).
In the overall analysis, combination therapy was no better than anti-TNF monotherapy in terms of 6-month remission, maintenance of response, or partial or full fistula closure, Dr. Jones and her associates reported. The same was true for subgroup analyses, but the odds ratio for infliximab reached statistical significance in a sensitivity analysis that included data from the ACCENT 2 (Clin Gastroenterol Hepatol. 2004;2:912-20) trial. “For the infliximab-only analysis, adding ACCENT 2 resulted in minimal change in the point estimate but, as expected, increased the precision of the 95% CIs (the lower CI increased from 0.97 to 1.06), which led to a statistically significant difference in the comparison between infliximab monotherapy and combination therapy,” the researchers commented. While sensitivity analyses have limitations, the finding “does raise the question” of whether the benefits of staying on an immunomodulator depend on the anti-TNF agent, they said.
Combination therapy did not heighten the chances of infusion reactions, malignancies, serious infections, or death, said the investigators. In fact, baseline immunomodulator exposure was associated with fewer injection site reactions among infliximab patients (OR, 0.46; 95% CI, 0.26-0.79). The researchers did not uncover publication bias, and found significant heterogeneity among studies only for the 6-month clinical response endpoint, they added.
The findings “challenge the clinical importance of combination therapy” in the setting of baseline immunomodulator exposure, but “it is hard to ignore the preponderance of data” on anti-TNF pharmacokinetics that support combination therapy over monotherapy, the investigators emphasized. “Whether combination therapy has a greater protective effect against anti-drug antibody development and lower trough levels for all anti-TNF agents or for patients previously exposed to anti-TNF agents is still in question,” they added. They called for a well-designed, randomized, placebo-controlled trial that uses objective measures of disease activity and follow patients long enough to assess efficacy.
The investigators reported no funding sources for the study. Dr. Jones reported having been a speaker for Jansen, Merck, Schering-Plough, Abbott, and AbbVie, and having served on advisory boards for Janssen, Abbott, and Takeda. Nine co-authors reported financial and consulting relationships with Jansen, Merck, Schering-Plough, Abbott, and a number of other pharmaceutical companies.
Source: American Gastroenterological Association
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Continuing an immunomodulator was no more effective than switching to anti-TNF monotherapy in a meta-analysis of patients with Crohn’s disease.
Major finding: Combination therapy was no more effective than anti-TNF monotherapy in terms of clinical response, remission induction, or fistula closure.
Data source: Meta-analysis of 11 randomized, controlled trials of 1,601 patients with luminal or fistulizing CD.
Disclosures: The investigators reported no funding sources for the study. Dr. Jones reported having been a speaker for Jansen, Merck, Schering-Plough, Abbott, and AbbVie, and serving on advisory boards for Janssen, Abbott, and Takeda. Nine coauthors reported financial and consulting relationships with Jansen, Merck, Schering-Plough, Abbott, and a number of other pharmaceutical companies.
Portal venous blood yielded higher levels of circulating tumor cells
Researchers detected circulating tumor cells (CTCs) in the portal venous blood of all patients with pancreaticobiliary cancer (PBC), but in the peripheral blood of only 22% of patients, according to a small single-center cohort study.
“We have shown that portal venous CTCs are far more common and higher in absolute numbers than peripheral blood CTCs. We also have shown the feasibility of obtaining portal venous CTCs noninvasively via endoscopic ultrasound,” Dr. Daniel Catenacci, Dr. Christopher Chapman, and their associates from the University of Chicago Medicine wrote in the December issue of Gastroenterology. “Portal vein CTCs can be used for molecular characterization of PBCs and share features of metastatic tissue.”
Circulating tumor cells have shown promise in the minimally invasive assessment of solid tumors, but the peripheral bloodstream contains only about one CTC for every 1 billion blood cells, limiting the potential sensitivity of testing. The researchers therefore used EUS guidance to transhepatically collect portal venous blood from 18 patients with PBCs. They quantified CTCs in both their portal venous and peripheral blood by using CellSearch, a commercially available test that uses magnetic beads labeled with antibodies against epithelial cell adhesion molecules. They only counted epithelial-derived cells as CTCs if they were morphologically compatible with tumor cells, CD45-negative, and positive for cytokeratins 8, 18, or 19 and 40,6-diamidino-2-phenylindole (Gastroenterology 2015 [doi: 10.1053/j.gastro.2015.08.050]).
Patients suffered no adverse affects from portal vein sampling, the researchers reported. They detected CTCs in the portal venous blood of all 18 patients, but in the peripheral blood of only four (22%) patients. Average CTC concentrations also were significantly higher in portal venous blood (118.4 ± 36.8 CTCs per 7.5 mL) compared with peripheral blood (0.8 ± 0.4 CTCs per 7.5 mL; P less than .01).
Among nine patients with nonmetastatic, resectable, or borderline-resectable PBC, portal vein CTCs averaged 83.2 per 7.5 mL (median, 62.0), the researchers reported. Whole-genome amplification and KRAS codon sequencing in one patient also showed that CTCs had the same mutations and similar levels of P16, SMAD4, and P53 proteins as tumor cells from a metastatic lymph node.
In addition, magnetic cell sorting identified CTC clusters, which other studies have implicated in the metastatic seeding of distant organs, the researchers said. Indeed, CTCs are now known to include “a heterogeneous population of cells, including apoptotic cells, cells undergoing epithelial-to-mesenchymal transition with loss of epithelial markers, epithelial cells, and cell clusters,” they noted. This heterogeneity might make CTCs useful for studying the pathogenesis and progression of PBCs, as well as for assessing the individual chances of recurrence or metastasis, they added. “Future prospective studies will define the role of portal vein CTCs or predictive biomarkers in the perioperative setting,” the investigators concluded.
The work was funded by the Rolfe Pancreatic Cancer Foundation, officers of the Gerald O. Mann Charitable Foundation, the National Institutes of Health, the University of Chicago Comprehensive Cancer Center, the Cancer Research Foundation, the Alliance for Clinical Trials in Oncology Foundation, and the Live Like Katie Foundation. The researchers reported having no conflicts of interest.
Source: American Gastroenterological Association
Researchers detected circulating tumor cells (CTCs) in the portal venous blood of all patients with pancreaticobiliary cancer (PBC), but in the peripheral blood of only 22% of patients, according to a small single-center cohort study.
“We have shown that portal venous CTCs are far more common and higher in absolute numbers than peripheral blood CTCs. We also have shown the feasibility of obtaining portal venous CTCs noninvasively via endoscopic ultrasound,” Dr. Daniel Catenacci, Dr. Christopher Chapman, and their associates from the University of Chicago Medicine wrote in the December issue of Gastroenterology. “Portal vein CTCs can be used for molecular characterization of PBCs and share features of metastatic tissue.”
Circulating tumor cells have shown promise in the minimally invasive assessment of solid tumors, but the peripheral bloodstream contains only about one CTC for every 1 billion blood cells, limiting the potential sensitivity of testing. The researchers therefore used EUS guidance to transhepatically collect portal venous blood from 18 patients with PBCs. They quantified CTCs in both their portal venous and peripheral blood by using CellSearch, a commercially available test that uses magnetic beads labeled with antibodies against epithelial cell adhesion molecules. They only counted epithelial-derived cells as CTCs if they were morphologically compatible with tumor cells, CD45-negative, and positive for cytokeratins 8, 18, or 19 and 40,6-diamidino-2-phenylindole (Gastroenterology 2015 [doi: 10.1053/j.gastro.2015.08.050]).
Patients suffered no adverse affects from portal vein sampling, the researchers reported. They detected CTCs in the portal venous blood of all 18 patients, but in the peripheral blood of only four (22%) patients. Average CTC concentrations also were significantly higher in portal venous blood (118.4 ± 36.8 CTCs per 7.5 mL) compared with peripheral blood (0.8 ± 0.4 CTCs per 7.5 mL; P less than .01).
Among nine patients with nonmetastatic, resectable, or borderline-resectable PBC, portal vein CTCs averaged 83.2 per 7.5 mL (median, 62.0), the researchers reported. Whole-genome amplification and KRAS codon sequencing in one patient also showed that CTCs had the same mutations and similar levels of P16, SMAD4, and P53 proteins as tumor cells from a metastatic lymph node.
In addition, magnetic cell sorting identified CTC clusters, which other studies have implicated in the metastatic seeding of distant organs, the researchers said. Indeed, CTCs are now known to include “a heterogeneous population of cells, including apoptotic cells, cells undergoing epithelial-to-mesenchymal transition with loss of epithelial markers, epithelial cells, and cell clusters,” they noted. This heterogeneity might make CTCs useful for studying the pathogenesis and progression of PBCs, as well as for assessing the individual chances of recurrence or metastasis, they added. “Future prospective studies will define the role of portal vein CTCs or predictive biomarkers in the perioperative setting,” the investigators concluded.
The work was funded by the Rolfe Pancreatic Cancer Foundation, officers of the Gerald O. Mann Charitable Foundation, the National Institutes of Health, the University of Chicago Comprehensive Cancer Center, the Cancer Research Foundation, the Alliance for Clinical Trials in Oncology Foundation, and the Live Like Katie Foundation. The researchers reported having no conflicts of interest.
Source: American Gastroenterological Association
Researchers detected circulating tumor cells (CTCs) in the portal venous blood of all patients with pancreaticobiliary cancer (PBC), but in the peripheral blood of only 22% of patients, according to a small single-center cohort study.
“We have shown that portal venous CTCs are far more common and higher in absolute numbers than peripheral blood CTCs. We also have shown the feasibility of obtaining portal venous CTCs noninvasively via endoscopic ultrasound,” Dr. Daniel Catenacci, Dr. Christopher Chapman, and their associates from the University of Chicago Medicine wrote in the December issue of Gastroenterology. “Portal vein CTCs can be used for molecular characterization of PBCs and share features of metastatic tissue.”
Circulating tumor cells have shown promise in the minimally invasive assessment of solid tumors, but the peripheral bloodstream contains only about one CTC for every 1 billion blood cells, limiting the potential sensitivity of testing. The researchers therefore used EUS guidance to transhepatically collect portal venous blood from 18 patients with PBCs. They quantified CTCs in both their portal venous and peripheral blood by using CellSearch, a commercially available test that uses magnetic beads labeled with antibodies against epithelial cell adhesion molecules. They only counted epithelial-derived cells as CTCs if they were morphologically compatible with tumor cells, CD45-negative, and positive for cytokeratins 8, 18, or 19 and 40,6-diamidino-2-phenylindole (Gastroenterology 2015 [doi: 10.1053/j.gastro.2015.08.050]).
Patients suffered no adverse affects from portal vein sampling, the researchers reported. They detected CTCs in the portal venous blood of all 18 patients, but in the peripheral blood of only four (22%) patients. Average CTC concentrations also were significantly higher in portal venous blood (118.4 ± 36.8 CTCs per 7.5 mL) compared with peripheral blood (0.8 ± 0.4 CTCs per 7.5 mL; P less than .01).
Among nine patients with nonmetastatic, resectable, or borderline-resectable PBC, portal vein CTCs averaged 83.2 per 7.5 mL (median, 62.0), the researchers reported. Whole-genome amplification and KRAS codon sequencing in one patient also showed that CTCs had the same mutations and similar levels of P16, SMAD4, and P53 proteins as tumor cells from a metastatic lymph node.
In addition, magnetic cell sorting identified CTC clusters, which other studies have implicated in the metastatic seeding of distant organs, the researchers said. Indeed, CTCs are now known to include “a heterogeneous population of cells, including apoptotic cells, cells undergoing epithelial-to-mesenchymal transition with loss of epithelial markers, epithelial cells, and cell clusters,” they noted. This heterogeneity might make CTCs useful for studying the pathogenesis and progression of PBCs, as well as for assessing the individual chances of recurrence or metastasis, they added. “Future prospective studies will define the role of portal vein CTCs or predictive biomarkers in the perioperative setting,” the investigators concluded.
The work was funded by the Rolfe Pancreatic Cancer Foundation, officers of the Gerald O. Mann Charitable Foundation, the National Institutes of Health, the University of Chicago Comprehensive Cancer Center, the Cancer Research Foundation, the Alliance for Clinical Trials in Oncology Foundation, and the Live Like Katie Foundation. The researchers reported having no conflicts of interest.
Source: American Gastroenterological Association
FROM GASTROENTEROLOGY
Key clinical point: Circulating pancreaticobiliary tumor cells were much more common in portal venous blood than in peripheral blood, and were molecularly similar to tumor tissue.
Major finding: Magnetic cell sorting revealed CTCs in the portal venous blood of all patients, but in the peripheral blood of only 22% of patients.
Data source: Prospective cohort study of 18 patients with pancreaticobiliary cancers, with portal venous blood collected under endoscopic guidance.
Disclosures: The work was funded by the Rolfe Pancreatic Cancer Foundation, officers of the Gerald O. Mann Charitable Foundation, the National Institutes of Health, the University of Chicago Comprehensive Cancer Center, the Cancer Research Foundation, the Alliance for Clinical Trials in Oncology Foundation, and the Live Like Katie Foundation. The investigators reported having no conflicts of interest.
Proportion of HCV patients in U.S. with cirrhosis climbing
SAN FRANCISCO – The prevalence of cirrhosis among patients in the United States infected with hepatitis C virus (HCV) is rising steeply, according to data presented at the annual meeting of the American Association for the Study of Liver Diseases (AASLD).
“While the overall prevalence of HCV in the United States has declined, the number of HCV patients with cirrhosis has risen significantly. As many patients with HCV are asymptomatic and unaware of their infection, the data underline the need for systematic HCV surveillance,” reported Dr. Prowpanga Udompop, a postdoctoral research fellow in gastroenterology at Stanford (Calif.) University.
In this study, the rates of cirrhosis were calculated from National Health and Nutrition Examination Survey (NHANES) data by using two surrogate indicators, the aspartate amino transferase to platelet ratio index (APRI) and the FIB-4 score. The rates of HCV and cirrhosis among those with HCV were compared for three eras, 1988-1994, 1999-2006, and 2007-2012.
A steady decline in HCV prevalence among the NHANES survey participants was observed over these three eras, falling from 1.5% in the first era to 1.2% in the second era and 1.0% in the third.
In contrast, the prevalence of cirrhosis among patients infected with HCV, according to estimates based on conventional APRI and FIB-4 thresholds for a high probability of cirrhosis, climbed steadily over this same period. By APRI score, the estimated prevalence of cirrhosis climbed from 6.6% in the first era to 7.6% and 17% in the next two eras, respectively. By FIB-4, the estimated rates, showing a very similar pattern and proportionality, rose sequentially from 8.6% to 10% and then to 16%.
In a logistic regression analysis, increasing age and increasing rates of diabetes mellitus among the HCV patients correlated with a rising prevalence of cirrhosis. For example, by odds ratio (OR), the risk of cirrhosis in those with diabetes was more than doubled as calculated with APRI score (OR, 2.33; 95% CI, 1.01-5.04) and more than tripled as calculated with FIB-4 (3.37; 95% CI, 1.24-9.5). Obesity was also strongly correlated with cirrhosis by APRI score (OR, 2.95; 95% CI, 1.15-7.57).
Neither race nor drinking status was significantly correlated with the increasing rates of cirrhosis as observed across the three eras using APRI score or the FIB-4 index.
The rapid and ongoing increase in the prevalence of cirrhosis in patients with HCV has important clinical implications, according to Dr. Udompap. By her estimates, 15% of HCV-infected patients aware of their diagnosis have cirrhosis, but the prevalence may be as high as 20% in those who are asymptomatic and undiagnosed.
Moreover, these rates are likely to continue to increase because of the increasing age and rising rates of obesity and diabetes among both the general population and patients infected with HCV. All three factors appear to contribute to the risk of HCV-associated cirrhosis. This suggests that although the national burden of HCV is declining, the rates of end-stage liver complications may increase without efforts to screen and initiate therapies that provide high rates of sustained virologic response.
“These data reinforce current guidelines for screening asymptomatic individuals and for systematic assessment for liver fibrosis in those diagnosed with HCV,” Dr. Udompap reported.
SAN FRANCISCO – The prevalence of cirrhosis among patients in the United States infected with hepatitis C virus (HCV) is rising steeply, according to data presented at the annual meeting of the American Association for the Study of Liver Diseases (AASLD).
“While the overall prevalence of HCV in the United States has declined, the number of HCV patients with cirrhosis has risen significantly. As many patients with HCV are asymptomatic and unaware of their infection, the data underline the need for systematic HCV surveillance,” reported Dr. Prowpanga Udompop, a postdoctoral research fellow in gastroenterology at Stanford (Calif.) University.
In this study, the rates of cirrhosis were calculated from National Health and Nutrition Examination Survey (NHANES) data by using two surrogate indicators, the aspartate amino transferase to platelet ratio index (APRI) and the FIB-4 score. The rates of HCV and cirrhosis among those with HCV were compared for three eras, 1988-1994, 1999-2006, and 2007-2012.
A steady decline in HCV prevalence among the NHANES survey participants was observed over these three eras, falling from 1.5% in the first era to 1.2% in the second era and 1.0% in the third.
In contrast, the prevalence of cirrhosis among patients infected with HCV, according to estimates based on conventional APRI and FIB-4 thresholds for a high probability of cirrhosis, climbed steadily over this same period. By APRI score, the estimated prevalence of cirrhosis climbed from 6.6% in the first era to 7.6% and 17% in the next two eras, respectively. By FIB-4, the estimated rates, showing a very similar pattern and proportionality, rose sequentially from 8.6% to 10% and then to 16%.
In a logistic regression analysis, increasing age and increasing rates of diabetes mellitus among the HCV patients correlated with a rising prevalence of cirrhosis. For example, by odds ratio (OR), the risk of cirrhosis in those with diabetes was more than doubled as calculated with APRI score (OR, 2.33; 95% CI, 1.01-5.04) and more than tripled as calculated with FIB-4 (3.37; 95% CI, 1.24-9.5). Obesity was also strongly correlated with cirrhosis by APRI score (OR, 2.95; 95% CI, 1.15-7.57).
Neither race nor drinking status was significantly correlated with the increasing rates of cirrhosis as observed across the three eras using APRI score or the FIB-4 index.
The rapid and ongoing increase in the prevalence of cirrhosis in patients with HCV has important clinical implications, according to Dr. Udompap. By her estimates, 15% of HCV-infected patients aware of their diagnosis have cirrhosis, but the prevalence may be as high as 20% in those who are asymptomatic and undiagnosed.
Moreover, these rates are likely to continue to increase because of the increasing age and rising rates of obesity and diabetes among both the general population and patients infected with HCV. All three factors appear to contribute to the risk of HCV-associated cirrhosis. This suggests that although the national burden of HCV is declining, the rates of end-stage liver complications may increase without efforts to screen and initiate therapies that provide high rates of sustained virologic response.
“These data reinforce current guidelines for screening asymptomatic individuals and for systematic assessment for liver fibrosis in those diagnosed with HCV,” Dr. Udompap reported.
SAN FRANCISCO – The prevalence of cirrhosis among patients in the United States infected with hepatitis C virus (HCV) is rising steeply, according to data presented at the annual meeting of the American Association for the Study of Liver Diseases (AASLD).
“While the overall prevalence of HCV in the United States has declined, the number of HCV patients with cirrhosis has risen significantly. As many patients with HCV are asymptomatic and unaware of their infection, the data underline the need for systematic HCV surveillance,” reported Dr. Prowpanga Udompop, a postdoctoral research fellow in gastroenterology at Stanford (Calif.) University.
In this study, the rates of cirrhosis were calculated from National Health and Nutrition Examination Survey (NHANES) data by using two surrogate indicators, the aspartate amino transferase to platelet ratio index (APRI) and the FIB-4 score. The rates of HCV and cirrhosis among those with HCV were compared for three eras, 1988-1994, 1999-2006, and 2007-2012.
A steady decline in HCV prevalence among the NHANES survey participants was observed over these three eras, falling from 1.5% in the first era to 1.2% in the second era and 1.0% in the third.
In contrast, the prevalence of cirrhosis among patients infected with HCV, according to estimates based on conventional APRI and FIB-4 thresholds for a high probability of cirrhosis, climbed steadily over this same period. By APRI score, the estimated prevalence of cirrhosis climbed from 6.6% in the first era to 7.6% and 17% in the next two eras, respectively. By FIB-4, the estimated rates, showing a very similar pattern and proportionality, rose sequentially from 8.6% to 10% and then to 16%.
In a logistic regression analysis, increasing age and increasing rates of diabetes mellitus among the HCV patients correlated with a rising prevalence of cirrhosis. For example, by odds ratio (OR), the risk of cirrhosis in those with diabetes was more than doubled as calculated with APRI score (OR, 2.33; 95% CI, 1.01-5.04) and more than tripled as calculated with FIB-4 (3.37; 95% CI, 1.24-9.5). Obesity was also strongly correlated with cirrhosis by APRI score (OR, 2.95; 95% CI, 1.15-7.57).
Neither race nor drinking status was significantly correlated with the increasing rates of cirrhosis as observed across the three eras using APRI score or the FIB-4 index.
The rapid and ongoing increase in the prevalence of cirrhosis in patients with HCV has important clinical implications, according to Dr. Udompap. By her estimates, 15% of HCV-infected patients aware of their diagnosis have cirrhosis, but the prevalence may be as high as 20% in those who are asymptomatic and undiagnosed.
Moreover, these rates are likely to continue to increase because of the increasing age and rising rates of obesity and diabetes among both the general population and patients infected with HCV. All three factors appear to contribute to the risk of HCV-associated cirrhosis. This suggests that although the national burden of HCV is declining, the rates of end-stage liver complications may increase without efforts to screen and initiate therapies that provide high rates of sustained virologic response.
“These data reinforce current guidelines for screening asymptomatic individuals and for systematic assessment for liver fibrosis in those diagnosed with HCV,” Dr. Udompap reported.
AT THE LIVER MEETING 2015
Key clinical point: Despite a national decline in the prevalence of hepatitis C virus infection, the prevalence of cirrhosis among HCV-infected patients is climbing.
Major finding: The estimated prevalence of cirrhosis in HCV-infected patients has climbed from 6.6% in the early 1990s to more than 17% in the present era.
Data source: A retrospective cohort study performed with a large database.
Disclosures: Dr. Udompap reported no relevant financial relationships.
Short-course DAA regimens for HCV provide limited cure rates
Shorter-course treatment with combinations of three or four different direct-acting antiviral agents achieved sustain viral response in 12 weeks (SVR12) in less than a third of patients with hepatitis C virus infection in an open-label, non-randomized, phase 2a proof-of-concept study.
SVR12 was achieved in 10 of 25 (40%) treatment-naive patients without cirrhosis who were treated with a 3-drug regimen consisting of ledipasvir and sofosbuvir plus GS-9451 (an NS3/4A protease inhibitor) for 4 weeks, and in 5 of 25 (20%) of 25 treatment-naive patients without cirrhosis treated with ledipasvir and sofosbuvir plus GS9451 and GS-9669 (a nonnucleoside NS5B polymerase inhibitor) for 4 weeks, Dr. Anita Kohli of the National Institutes of Health Clinical Center, Bethesda, Md. and her colleagues reported Nov. 23 in Annals of Internal Medicine.
“Given the high cost of DAAs, the medical care required, and the improvements in patient adherence with reductions in treatment duration, attempts to evaluate shorter courses of therapy could have important clinical and public health implications,” Dr. Kohli noted.
Lower baseline HCV viral load, younger age, and HCV genotype 1b were associated with SVR12 with this shortened (vs. the usual 6 weeks) course of direct-acting antiviral (DAA) therapy. Adverse events were mainly mild fatigue, diarrhea, and headaches occurring in 48% and 72% of patients in the 3- and 4-drug regimen groups, respectively, Dr. Kohli said (Ann Intern Med. 2015 Nov. 23[doi:10.7326/M15-0642).
“Sixty-eight percent (34 of 50) of patients had viral relapse, the majority (68%) by posttreatment week 4. Thus, a treatment duration of 4 weeks with 3 or 4 potent DAAs is not sufficient to cure HCV infection in most patients,” she wrote, noting, however, that “some patients are capable of achieving SVR with 4 weeks of therapy, which could be attributable to the presence of several favorable factors, such as early fibrosis, low viral burden, and absence of [resistance-associated variants].
This study was funded in part by the NIH and the German Research Foundation. Study medications were provided by Gilead Sciences. Dr. Kohli reported having no other disclosures. Multiple authors reported other disclosures, including employment and/or stock ownership with Gilead Sciences, research and other funding from Gilead Sciences, and/or stock ownership in Merck, Pfizer, and Johnson & Johnson.
Shorter-course treatment with combinations of three or four different direct-acting antiviral agents achieved sustain viral response in 12 weeks (SVR12) in less than a third of patients with hepatitis C virus infection in an open-label, non-randomized, phase 2a proof-of-concept study.
SVR12 was achieved in 10 of 25 (40%) treatment-naive patients without cirrhosis who were treated with a 3-drug regimen consisting of ledipasvir and sofosbuvir plus GS-9451 (an NS3/4A protease inhibitor) for 4 weeks, and in 5 of 25 (20%) of 25 treatment-naive patients without cirrhosis treated with ledipasvir and sofosbuvir plus GS9451 and GS-9669 (a nonnucleoside NS5B polymerase inhibitor) for 4 weeks, Dr. Anita Kohli of the National Institutes of Health Clinical Center, Bethesda, Md. and her colleagues reported Nov. 23 in Annals of Internal Medicine.
“Given the high cost of DAAs, the medical care required, and the improvements in patient adherence with reductions in treatment duration, attempts to evaluate shorter courses of therapy could have important clinical and public health implications,” Dr. Kohli noted.
Lower baseline HCV viral load, younger age, and HCV genotype 1b were associated with SVR12 with this shortened (vs. the usual 6 weeks) course of direct-acting antiviral (DAA) therapy. Adverse events were mainly mild fatigue, diarrhea, and headaches occurring in 48% and 72% of patients in the 3- and 4-drug regimen groups, respectively, Dr. Kohli said (Ann Intern Med. 2015 Nov. 23[doi:10.7326/M15-0642).
“Sixty-eight percent (34 of 50) of patients had viral relapse, the majority (68%) by posttreatment week 4. Thus, a treatment duration of 4 weeks with 3 or 4 potent DAAs is not sufficient to cure HCV infection in most patients,” she wrote, noting, however, that “some patients are capable of achieving SVR with 4 weeks of therapy, which could be attributable to the presence of several favorable factors, such as early fibrosis, low viral burden, and absence of [resistance-associated variants].
This study was funded in part by the NIH and the German Research Foundation. Study medications were provided by Gilead Sciences. Dr. Kohli reported having no other disclosures. Multiple authors reported other disclosures, including employment and/or stock ownership with Gilead Sciences, research and other funding from Gilead Sciences, and/or stock ownership in Merck, Pfizer, and Johnson & Johnson.
Shorter-course treatment with combinations of three or four different direct-acting antiviral agents achieved sustain viral response in 12 weeks (SVR12) in less than a third of patients with hepatitis C virus infection in an open-label, non-randomized, phase 2a proof-of-concept study.
SVR12 was achieved in 10 of 25 (40%) treatment-naive patients without cirrhosis who were treated with a 3-drug regimen consisting of ledipasvir and sofosbuvir plus GS-9451 (an NS3/4A protease inhibitor) for 4 weeks, and in 5 of 25 (20%) of 25 treatment-naive patients without cirrhosis treated with ledipasvir and sofosbuvir plus GS9451 and GS-9669 (a nonnucleoside NS5B polymerase inhibitor) for 4 weeks, Dr. Anita Kohli of the National Institutes of Health Clinical Center, Bethesda, Md. and her colleagues reported Nov. 23 in Annals of Internal Medicine.
“Given the high cost of DAAs, the medical care required, and the improvements in patient adherence with reductions in treatment duration, attempts to evaluate shorter courses of therapy could have important clinical and public health implications,” Dr. Kohli noted.
Lower baseline HCV viral load, younger age, and HCV genotype 1b were associated with SVR12 with this shortened (vs. the usual 6 weeks) course of direct-acting antiviral (DAA) therapy. Adverse events were mainly mild fatigue, diarrhea, and headaches occurring in 48% and 72% of patients in the 3- and 4-drug regimen groups, respectively, Dr. Kohli said (Ann Intern Med. 2015 Nov. 23[doi:10.7326/M15-0642).
“Sixty-eight percent (34 of 50) of patients had viral relapse, the majority (68%) by posttreatment week 4. Thus, a treatment duration of 4 weeks with 3 or 4 potent DAAs is not sufficient to cure HCV infection in most patients,” she wrote, noting, however, that “some patients are capable of achieving SVR with 4 weeks of therapy, which could be attributable to the presence of several favorable factors, such as early fibrosis, low viral burden, and absence of [resistance-associated variants].
This study was funded in part by the NIH and the German Research Foundation. Study medications were provided by Gilead Sciences. Dr. Kohli reported having no other disclosures. Multiple authors reported other disclosures, including employment and/or stock ownership with Gilead Sciences, research and other funding from Gilead Sciences, and/or stock ownership in Merck, Pfizer, and Johnson & Johnson.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Four weeks of three- or four-agent DAA therapy was well tolerated, but less than a third of non cirrhotic patients with hepatitis C virus genotype 1 infection achieved sustained virologic response at 12 weeks.
Major finding: Only 30% of study subjects achieved SVR12.
Data source: An open-label, non-randomized, phase 2a proof-of-concept study of 50 patients.
Disclosures: This study was funded in part by the NIH and the German Research Foundation. Study medications were provided by Gilead Sciences. Dr. Kohli reported having no other disclosures. Multiple authors reported other disclosures, including employment and/or stock ownership with Gilead Sciences, research and other funding from Gilead Sciences, and/or stock ownership in Merck, Pfizer, and Johnson & Johnson.
VIDEO: U.S. hepatitis C treatment capacity falls short of need
SAN FRANCISCO – The U.S. health care system’s capacity to treat patients who need hepatitis C treatment has improved since 2014, but it still falls far short of what’s needed, according to an analysis presented at the annual meeting of the American Association for the Study of Liver Diseases.
Despite recent improvements, it would still take at least 6 years to treat the majority of patients in need of hepatitis C therapy, explained Jagpreet Chhatwal, Ph.D., of Massachusetts General Hospital, Boston. “Even in the [direct-acting antiviral] era, the burden of hepatitis C remains substantial for a disease for which we have a cure.”
To predict trends in hepatitis C treatment, Dr. Chhatwal and his colleagues developed a mathematical model of health care factors, such as changing treatment regimens, screening policies, and widened insurance coverage.
“We wanted to put all of these different components together to project how the disease burden would change in the near future, and how the disease burden would look if we increased the treatment capacity for hepatitis C,” he said.
In an interview, Dr. Chhatwal discussed his findings and how capacity changes could affect the speed with which those in need receive necessary hepatitis C treatment.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – The U.S. health care system’s capacity to treat patients who need hepatitis C treatment has improved since 2014, but it still falls far short of what’s needed, according to an analysis presented at the annual meeting of the American Association for the Study of Liver Diseases.
Despite recent improvements, it would still take at least 6 years to treat the majority of patients in need of hepatitis C therapy, explained Jagpreet Chhatwal, Ph.D., of Massachusetts General Hospital, Boston. “Even in the [direct-acting antiviral] era, the burden of hepatitis C remains substantial for a disease for which we have a cure.”
To predict trends in hepatitis C treatment, Dr. Chhatwal and his colleagues developed a mathematical model of health care factors, such as changing treatment regimens, screening policies, and widened insurance coverage.
“We wanted to put all of these different components together to project how the disease burden would change in the near future, and how the disease burden would look if we increased the treatment capacity for hepatitis C,” he said.
In an interview, Dr. Chhatwal discussed his findings and how capacity changes could affect the speed with which those in need receive necessary hepatitis C treatment.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – The U.S. health care system’s capacity to treat patients who need hepatitis C treatment has improved since 2014, but it still falls far short of what’s needed, according to an analysis presented at the annual meeting of the American Association for the Study of Liver Diseases.
Despite recent improvements, it would still take at least 6 years to treat the majority of patients in need of hepatitis C therapy, explained Jagpreet Chhatwal, Ph.D., of Massachusetts General Hospital, Boston. “Even in the [direct-acting antiviral] era, the burden of hepatitis C remains substantial for a disease for which we have a cure.”
To predict trends in hepatitis C treatment, Dr. Chhatwal and his colleagues developed a mathematical model of health care factors, such as changing treatment regimens, screening policies, and widened insurance coverage.
“We wanted to put all of these different components together to project how the disease burden would change in the near future, and how the disease burden would look if we increased the treatment capacity for hepatitis C,” he said.
In an interview, Dr. Chhatwal discussed his findings and how capacity changes could affect the speed with which those in need receive necessary hepatitis C treatment.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE LIVER MEETING 2015
AASLD: Pilot study shows value of response-guided therapy for HCV GT1b
SAN FRANCISCO – Response-guided therapy using all-oral, triple direct-acting antiviral (DAA) therapy appears useful for shortening the duration of treatment in noncirrhotic patients with hepatitis C virus genotype 1b infection, according to findings from the randomized proof-of-concept SODAPI study.
The findings of the open-label study strongly suggest that administration of potent triple regimens containing NS3, NS5A, and NS5B HCV inhibitors leads to rapid virologic response within 2 days in a majority of treated patients, Dr. George K. Lau of Emory University, Atlanta, reported at the annual meeting of the American Association for the Study of Liver Diseases.
Study subjects were 26 Chinese patients who received either sofosbuvir, ledipasvir, and asunaprevir (group 1, 12 patients); sofosbuvir, daclatasvir, and simeprevir (group 2, 6 patients); or sofosbuvir, daclatasvir, and asunaprevir (group 3, 8 patients) at approved doses. Those who achieved rapid virologic response remained on the regimen for 3 weeks; those who did not were treated for 8-12 weeks.
Rapid virologic response was achieved by 6 of 12 group 1 patients, 6 of 6 group 2 patients, and 6 of 8 group 3 patients. Baseline viral load was lower in those with rapid virologic response vs. those without (5.96 vs. 7.00 log10 IU/mL), Dr. Lau noted.
All 18 subjects with rapid virologic response and 3 weeks of treatment achieved the primary endpoint of plasma HCV RNA below the detectable limit at 12 weeks (SVR12). Median time to plasma HCV RNA less than 25 IU/mL was shortest in group 1 vs. group 3, he said.
Treatment was well tolerated; no patients discontinued therapy and no significant adverse events were reported.
Patients in the study were noncirrhotic patients with chronic hepatitis C genotype 1b infection with a median age of 34 years, median body mass index of 21.7 kg/m2, and baseline mean HCV RNA of 6.55 log10 IU/mL. Six were men, 12 were women.
DAAs have a high cure rate and favorable tolerability in persons infected with hepatitis C virus, but shorter courses could improve adherence and affordability and could increase accessibility to DAAs, Dr. Lau said.
He and his colleagues “postulated that the addition of an NS3 protease inhibitor to dual NS5A-NS5B (nucleoside) inhibitors would enhance antiviral efficacy and reduce treatment duration to 3 weeks in those with a rapid virologic response defined as plasma HCV RNA less than 500 IU/mL by day 2.”
Based on these positive early findings, future studies exploring this response-guided approach to therapy are recommended, as this approach has the potential to reduce therapy duration and drug costs, and to improve accessibility and adherence, he concluded.
Dr. Lau is a consultant for Roche and Novartis.
SAN FRANCISCO – Response-guided therapy using all-oral, triple direct-acting antiviral (DAA) therapy appears useful for shortening the duration of treatment in noncirrhotic patients with hepatitis C virus genotype 1b infection, according to findings from the randomized proof-of-concept SODAPI study.
The findings of the open-label study strongly suggest that administration of potent triple regimens containing NS3, NS5A, and NS5B HCV inhibitors leads to rapid virologic response within 2 days in a majority of treated patients, Dr. George K. Lau of Emory University, Atlanta, reported at the annual meeting of the American Association for the Study of Liver Diseases.
Study subjects were 26 Chinese patients who received either sofosbuvir, ledipasvir, and asunaprevir (group 1, 12 patients); sofosbuvir, daclatasvir, and simeprevir (group 2, 6 patients); or sofosbuvir, daclatasvir, and asunaprevir (group 3, 8 patients) at approved doses. Those who achieved rapid virologic response remained on the regimen for 3 weeks; those who did not were treated for 8-12 weeks.
Rapid virologic response was achieved by 6 of 12 group 1 patients, 6 of 6 group 2 patients, and 6 of 8 group 3 patients. Baseline viral load was lower in those with rapid virologic response vs. those without (5.96 vs. 7.00 log10 IU/mL), Dr. Lau noted.
All 18 subjects with rapid virologic response and 3 weeks of treatment achieved the primary endpoint of plasma HCV RNA below the detectable limit at 12 weeks (SVR12). Median time to plasma HCV RNA less than 25 IU/mL was shortest in group 1 vs. group 3, he said.
Treatment was well tolerated; no patients discontinued therapy and no significant adverse events were reported.
Patients in the study were noncirrhotic patients with chronic hepatitis C genotype 1b infection with a median age of 34 years, median body mass index of 21.7 kg/m2, and baseline mean HCV RNA of 6.55 log10 IU/mL. Six were men, 12 were women.
DAAs have a high cure rate and favorable tolerability in persons infected with hepatitis C virus, but shorter courses could improve adherence and affordability and could increase accessibility to DAAs, Dr. Lau said.
He and his colleagues “postulated that the addition of an NS3 protease inhibitor to dual NS5A-NS5B (nucleoside) inhibitors would enhance antiviral efficacy and reduce treatment duration to 3 weeks in those with a rapid virologic response defined as plasma HCV RNA less than 500 IU/mL by day 2.”
Based on these positive early findings, future studies exploring this response-guided approach to therapy are recommended, as this approach has the potential to reduce therapy duration and drug costs, and to improve accessibility and adherence, he concluded.
Dr. Lau is a consultant for Roche and Novartis.
SAN FRANCISCO – Response-guided therapy using all-oral, triple direct-acting antiviral (DAA) therapy appears useful for shortening the duration of treatment in noncirrhotic patients with hepatitis C virus genotype 1b infection, according to findings from the randomized proof-of-concept SODAPI study.
The findings of the open-label study strongly suggest that administration of potent triple regimens containing NS3, NS5A, and NS5B HCV inhibitors leads to rapid virologic response within 2 days in a majority of treated patients, Dr. George K. Lau of Emory University, Atlanta, reported at the annual meeting of the American Association for the Study of Liver Diseases.
Study subjects were 26 Chinese patients who received either sofosbuvir, ledipasvir, and asunaprevir (group 1, 12 patients); sofosbuvir, daclatasvir, and simeprevir (group 2, 6 patients); or sofosbuvir, daclatasvir, and asunaprevir (group 3, 8 patients) at approved doses. Those who achieved rapid virologic response remained on the regimen for 3 weeks; those who did not were treated for 8-12 weeks.
Rapid virologic response was achieved by 6 of 12 group 1 patients, 6 of 6 group 2 patients, and 6 of 8 group 3 patients. Baseline viral load was lower in those with rapid virologic response vs. those without (5.96 vs. 7.00 log10 IU/mL), Dr. Lau noted.
All 18 subjects with rapid virologic response and 3 weeks of treatment achieved the primary endpoint of plasma HCV RNA below the detectable limit at 12 weeks (SVR12). Median time to plasma HCV RNA less than 25 IU/mL was shortest in group 1 vs. group 3, he said.
Treatment was well tolerated; no patients discontinued therapy and no significant adverse events were reported.
Patients in the study were noncirrhotic patients with chronic hepatitis C genotype 1b infection with a median age of 34 years, median body mass index of 21.7 kg/m2, and baseline mean HCV RNA of 6.55 log10 IU/mL. Six were men, 12 were women.
DAAs have a high cure rate and favorable tolerability in persons infected with hepatitis C virus, but shorter courses could improve adherence and affordability and could increase accessibility to DAAs, Dr. Lau said.
He and his colleagues “postulated that the addition of an NS3 protease inhibitor to dual NS5A-NS5B (nucleoside) inhibitors would enhance antiviral efficacy and reduce treatment duration to 3 weeks in those with a rapid virologic response defined as plasma HCV RNA less than 500 IU/mL by day 2.”
Based on these positive early findings, future studies exploring this response-guided approach to therapy are recommended, as this approach has the potential to reduce therapy duration and drug costs, and to improve accessibility and adherence, he concluded.
Dr. Lau is a consultant for Roche and Novartis.
AT THE LIVER MEETING 2015
Key clinical point: Response-guided therapy using all-oral, triple direct-acting antiviral therapy appears useful for shortening the duration of treatment in noncirrhotic patients with hepatitis C virus genotype 1b infection according to a proof-of-concept study.
Major finding: Rapid virologic response was achieved by 6 of 12 group 1 patients, 6 of 6 group 2 patients, and 6 of 8 group 3 patients; all 18 subjects with rapid virologic response achieved SVR12.
Data source: A randomized, open-label pilot study of 26 patients.
Disclosures: Dr. Lau is a consultant for Roche and Novartis.
Elevated liver cancer risk after HCV cure may justify surveillance
SAN FRANCISCO – The risk of hepatocellular carcinoma remains sufficiently high in some subgroups who have achieved sustained virologic response to treatment to justify continued cancer surveillance, according to findings from a large cohort study presented at the annual meeting of the American Association for the Study of Liver Diseases.
The risk of hepatocellular carcinoma (HCC) after sustained virologic response (SVR) was relatively elevated in those who were infected with genotype 3 of the hepatitis C virus (HCV), those with diabetes, and those older than 65 years. But those who had cirrhosis at the time of SVR appear to have the highest risk and need for continued surveillance, reported Dr. Hashem B. El-Serag, chief of the gastroenterology and hepatology section at Baylor College of Medicine, Houston.
In this study, data from the national Veterans Affairs (VA) health system were available for 10,730 patients who achieved SVR. When compared to 11,290 patients who did not achieve SVR, the risk of HCC was reduced by two thirds (hazard ratio, 0.358), but Dr. El-Serag labeled this finding “old news.” Instead, his focus was on the 100 cases of HCC identified after SVR over the course of 30,000 patient-years of follow-up.
While the annualized overall incidence of HCC after SVR was 0.32%, incidence rates ranged greatly by subgroup. For those with genotype 3 HCV at the time of SVR, the incidence was 0.558 cancers/year (versus 0.334 for genotype 1). A similar increase in HCC was observed in patients with diabetes (0.558/year). The rate climbed to 0.953/year for those who were age 65 years or older at the time of SVR.
The incidence of HCC was 1.54%/year in those with cirrhosis at the time of SVR, which was the highest rate among subgroups evaluated. This figure is notable because guidelines suggest that surveillance for HCC is justified for patients with an estimated annual risk of 1.5% per year, according to Dr. El-Serag.
“The presence of cirrhosis at SVR carried a 4.45 increase in the adjusted hazard ratio for HCC when compared to the absence of cirrhosis [P less than .0001],” he reported. Being 65 and older was associated with a nearly fivefold increase in hazard ratio of HCC compared with younger patients (HR 4.69; P = .0003), while the presence of diabetes was associated with a nearly twofold risk (HR 2.07; P = .0001).
It is notable that no concentration of cases of HCC was observed over the course of follow-up. Rather, there was a relatively equal distribution over time.
In addition to the known limitations of cohort studies, Dr. El-Serag cautioned that almost all SVRs in this database were achieved with interferon-based therapies. This is important, because the risk for HCC may differ when SVR is achieved with the newer direct-acting antivirals (DAAs). Another limitation is that most patients in the VA database are male.
However, the data strongly suggest that HCC risk after SVR differs markedly among subpopulations of HCV patients. While these findings have implications for considering continued surveillance of HCC, they also may be meaningful for timing of HCV therapy.
“It is obvious that if you treat and cure [patients early in the course of their disease and while they are young], your risk of HCC is much lower than if you treat late and old,” said Dr. El-Serag.
This is the first study to evaluate risk of HCC after SVR in a large and diverse population, according to Dr. El-Serag. The moderator of the oral session in which the report was presented, Dr. Joseph K. Lim, director of the viral hepatitis program at Yale University, New Haven, Conn., characterized the findings as “incredibly important.” Despite the frequency with which SVR is now being achieved with DAAs, these data confirm that some groups of patients may remain at substantial risk of HCV complications even after successful therapy.
Dr. El-Serag reeported that he has a financial relationship with Gilead.
SAN FRANCISCO – The risk of hepatocellular carcinoma remains sufficiently high in some subgroups who have achieved sustained virologic response to treatment to justify continued cancer surveillance, according to findings from a large cohort study presented at the annual meeting of the American Association for the Study of Liver Diseases.
The risk of hepatocellular carcinoma (HCC) after sustained virologic response (SVR) was relatively elevated in those who were infected with genotype 3 of the hepatitis C virus (HCV), those with diabetes, and those older than 65 years. But those who had cirrhosis at the time of SVR appear to have the highest risk and need for continued surveillance, reported Dr. Hashem B. El-Serag, chief of the gastroenterology and hepatology section at Baylor College of Medicine, Houston.
In this study, data from the national Veterans Affairs (VA) health system were available for 10,730 patients who achieved SVR. When compared to 11,290 patients who did not achieve SVR, the risk of HCC was reduced by two thirds (hazard ratio, 0.358), but Dr. El-Serag labeled this finding “old news.” Instead, his focus was on the 100 cases of HCC identified after SVR over the course of 30,000 patient-years of follow-up.
While the annualized overall incidence of HCC after SVR was 0.32%, incidence rates ranged greatly by subgroup. For those with genotype 3 HCV at the time of SVR, the incidence was 0.558 cancers/year (versus 0.334 for genotype 1). A similar increase in HCC was observed in patients with diabetes (0.558/year). The rate climbed to 0.953/year for those who were age 65 years or older at the time of SVR.
The incidence of HCC was 1.54%/year in those with cirrhosis at the time of SVR, which was the highest rate among subgroups evaluated. This figure is notable because guidelines suggest that surveillance for HCC is justified for patients with an estimated annual risk of 1.5% per year, according to Dr. El-Serag.
“The presence of cirrhosis at SVR carried a 4.45 increase in the adjusted hazard ratio for HCC when compared to the absence of cirrhosis [P less than .0001],” he reported. Being 65 and older was associated with a nearly fivefold increase in hazard ratio of HCC compared with younger patients (HR 4.69; P = .0003), while the presence of diabetes was associated with a nearly twofold risk (HR 2.07; P = .0001).
It is notable that no concentration of cases of HCC was observed over the course of follow-up. Rather, there was a relatively equal distribution over time.
In addition to the known limitations of cohort studies, Dr. El-Serag cautioned that almost all SVRs in this database were achieved with interferon-based therapies. This is important, because the risk for HCC may differ when SVR is achieved with the newer direct-acting antivirals (DAAs). Another limitation is that most patients in the VA database are male.
However, the data strongly suggest that HCC risk after SVR differs markedly among subpopulations of HCV patients. While these findings have implications for considering continued surveillance of HCC, they also may be meaningful for timing of HCV therapy.
“It is obvious that if you treat and cure [patients early in the course of their disease and while they are young], your risk of HCC is much lower than if you treat late and old,” said Dr. El-Serag.
This is the first study to evaluate risk of HCC after SVR in a large and diverse population, according to Dr. El-Serag. The moderator of the oral session in which the report was presented, Dr. Joseph K. Lim, director of the viral hepatitis program at Yale University, New Haven, Conn., characterized the findings as “incredibly important.” Despite the frequency with which SVR is now being achieved with DAAs, these data confirm that some groups of patients may remain at substantial risk of HCV complications even after successful therapy.
Dr. El-Serag reeported that he has a financial relationship with Gilead.
SAN FRANCISCO – The risk of hepatocellular carcinoma remains sufficiently high in some subgroups who have achieved sustained virologic response to treatment to justify continued cancer surveillance, according to findings from a large cohort study presented at the annual meeting of the American Association for the Study of Liver Diseases.
The risk of hepatocellular carcinoma (HCC) after sustained virologic response (SVR) was relatively elevated in those who were infected with genotype 3 of the hepatitis C virus (HCV), those with diabetes, and those older than 65 years. But those who had cirrhosis at the time of SVR appear to have the highest risk and need for continued surveillance, reported Dr. Hashem B. El-Serag, chief of the gastroenterology and hepatology section at Baylor College of Medicine, Houston.
In this study, data from the national Veterans Affairs (VA) health system were available for 10,730 patients who achieved SVR. When compared to 11,290 patients who did not achieve SVR, the risk of HCC was reduced by two thirds (hazard ratio, 0.358), but Dr. El-Serag labeled this finding “old news.” Instead, his focus was on the 100 cases of HCC identified after SVR over the course of 30,000 patient-years of follow-up.
While the annualized overall incidence of HCC after SVR was 0.32%, incidence rates ranged greatly by subgroup. For those with genotype 3 HCV at the time of SVR, the incidence was 0.558 cancers/year (versus 0.334 for genotype 1). A similar increase in HCC was observed in patients with diabetes (0.558/year). The rate climbed to 0.953/year for those who were age 65 years or older at the time of SVR.
The incidence of HCC was 1.54%/year in those with cirrhosis at the time of SVR, which was the highest rate among subgroups evaluated. This figure is notable because guidelines suggest that surveillance for HCC is justified for patients with an estimated annual risk of 1.5% per year, according to Dr. El-Serag.
“The presence of cirrhosis at SVR carried a 4.45 increase in the adjusted hazard ratio for HCC when compared to the absence of cirrhosis [P less than .0001],” he reported. Being 65 and older was associated with a nearly fivefold increase in hazard ratio of HCC compared with younger patients (HR 4.69; P = .0003), while the presence of diabetes was associated with a nearly twofold risk (HR 2.07; P = .0001).
It is notable that no concentration of cases of HCC was observed over the course of follow-up. Rather, there was a relatively equal distribution over time.
In addition to the known limitations of cohort studies, Dr. El-Serag cautioned that almost all SVRs in this database were achieved with interferon-based therapies. This is important, because the risk for HCC may differ when SVR is achieved with the newer direct-acting antivirals (DAAs). Another limitation is that most patients in the VA database are male.
However, the data strongly suggest that HCC risk after SVR differs markedly among subpopulations of HCV patients. While these findings have implications for considering continued surveillance of HCC, they also may be meaningful for timing of HCV therapy.
“It is obvious that if you treat and cure [patients early in the course of their disease and while they are young], your risk of HCC is much lower than if you treat late and old,” said Dr. El-Serag.
This is the first study to evaluate risk of HCC after SVR in a large and diverse population, according to Dr. El-Serag. The moderator of the oral session in which the report was presented, Dr. Joseph K. Lim, director of the viral hepatitis program at Yale University, New Haven, Conn., characterized the findings as “incredibly important.” Despite the frequency with which SVR is now being achieved with DAAs, these data confirm that some groups of patients may remain at substantial risk of HCV complications even after successful therapy.
Dr. El-Serag reeported that he has a financial relationship with Gilead.
AT THE LIVER MEETING 2015
Key clinical point: Elevated rates of hepatocellular carcinoma (HCC) remain elevated in patients with hepatitis C virus infection who achieved a sustained virologic response.
Major finding: In a VA database, the overall risk of HCC after SVR was 0.3% per year but was higher among the elderly, those with diabetes, and those with cirrhosis.
Data source: Retrospective cohort study performed with a large database.
Disclosures: Dr. El-Serag has a financial relationship with Gilead.
Transplant waiting-list registrations dropped after direct acting–antiviral approval
SAN FRANCISCO – The number of new waiting-list registrations for liver transplantation among patients with hepatitis C virus declined significantly after the introduction of second-generation direct-acting antiviral agents, according to a review of United Network for Organ Sharing data.
New waiting-list registrations (NWRs) through March 31, 2015 – based on the most recent data available as of September 2015 – ranged from 740 to 976 per month between August 2012 and March 2015, and a review of the data show that HCV-specific NWRs declined by 23% overall in the 15 months after the Food and Drug Administration approved simeprevir (Nov. 22, 2013) and sofosbuvir (Dec. 6, 2013) vs. the 15 months prior (from 34.8% to 26.8%), Dr. Ryan B. Perumpail reported at the annual meeting of the American Association for the Study of Liver Diseases.
Further, the proportion of HCV patients without hepatocellular carcinoma among new waiting-list registrations declined by 33% (from 23.0% to 15.4%) and there was a significant decline in NWRs for liver transplants in nonhepatocellular-carcinoma HCV patients from January 2014 to March 2015 (153 per month) vs. August 2012 to October 2013 (mean 188 per month), for a mean difference of 35.0, said Dr. Perumpail of Stanford University Medical Center, Palo Alto, Calif.
Among the HCV-related NWRs for liver transplantation, the proportion without hepatocellular carcinoma declined 12.5% (from 66.3% to 58.0%).
Direct-acting antiviral therapy has been prioritized in patients with HCV-related cirrhosis in an effort to slow clinical disease progress and to induce regression of hepatic histologic damage, Dr. Perumpail explained.
Thought limited by the retrospective design of the study, the findings suggest that the use of direct-acting antivirals contributed to a downward trend in NWRs for liver transplantation among HCV patients without hepatocellular carcinoma.
Dr. Perumpail reported having no disclosures.
SAN FRANCISCO – The number of new waiting-list registrations for liver transplantation among patients with hepatitis C virus declined significantly after the introduction of second-generation direct-acting antiviral agents, according to a review of United Network for Organ Sharing data.
New waiting-list registrations (NWRs) through March 31, 2015 – based on the most recent data available as of September 2015 – ranged from 740 to 976 per month between August 2012 and March 2015, and a review of the data show that HCV-specific NWRs declined by 23% overall in the 15 months after the Food and Drug Administration approved simeprevir (Nov. 22, 2013) and sofosbuvir (Dec. 6, 2013) vs. the 15 months prior (from 34.8% to 26.8%), Dr. Ryan B. Perumpail reported at the annual meeting of the American Association for the Study of Liver Diseases.
Further, the proportion of HCV patients without hepatocellular carcinoma among new waiting-list registrations declined by 33% (from 23.0% to 15.4%) and there was a significant decline in NWRs for liver transplants in nonhepatocellular-carcinoma HCV patients from January 2014 to March 2015 (153 per month) vs. August 2012 to October 2013 (mean 188 per month), for a mean difference of 35.0, said Dr. Perumpail of Stanford University Medical Center, Palo Alto, Calif.
Among the HCV-related NWRs for liver transplantation, the proportion without hepatocellular carcinoma declined 12.5% (from 66.3% to 58.0%).
Direct-acting antiviral therapy has been prioritized in patients with HCV-related cirrhosis in an effort to slow clinical disease progress and to induce regression of hepatic histologic damage, Dr. Perumpail explained.
Thought limited by the retrospective design of the study, the findings suggest that the use of direct-acting antivirals contributed to a downward trend in NWRs for liver transplantation among HCV patients without hepatocellular carcinoma.
Dr. Perumpail reported having no disclosures.
SAN FRANCISCO – The number of new waiting-list registrations for liver transplantation among patients with hepatitis C virus declined significantly after the introduction of second-generation direct-acting antiviral agents, according to a review of United Network for Organ Sharing data.
New waiting-list registrations (NWRs) through March 31, 2015 – based on the most recent data available as of September 2015 – ranged from 740 to 976 per month between August 2012 and March 2015, and a review of the data show that HCV-specific NWRs declined by 23% overall in the 15 months after the Food and Drug Administration approved simeprevir (Nov. 22, 2013) and sofosbuvir (Dec. 6, 2013) vs. the 15 months prior (from 34.8% to 26.8%), Dr. Ryan B. Perumpail reported at the annual meeting of the American Association for the Study of Liver Diseases.
Further, the proportion of HCV patients without hepatocellular carcinoma among new waiting-list registrations declined by 33% (from 23.0% to 15.4%) and there was a significant decline in NWRs for liver transplants in nonhepatocellular-carcinoma HCV patients from January 2014 to March 2015 (153 per month) vs. August 2012 to October 2013 (mean 188 per month), for a mean difference of 35.0, said Dr. Perumpail of Stanford University Medical Center, Palo Alto, Calif.
Among the HCV-related NWRs for liver transplantation, the proportion without hepatocellular carcinoma declined 12.5% (from 66.3% to 58.0%).
Direct-acting antiviral therapy has been prioritized in patients with HCV-related cirrhosis in an effort to slow clinical disease progress and to induce regression of hepatic histologic damage, Dr. Perumpail explained.
Thought limited by the retrospective design of the study, the findings suggest that the use of direct-acting antivirals contributed to a downward trend in NWRs for liver transplantation among HCV patients without hepatocellular carcinoma.
Dr. Perumpail reported having no disclosures.
AT THE LIVER MEETING 2015
Key clinical point: New waiting-list registrations for liver transplantation in patients with hepatitis C virus declined significantly after introduction of second-generation direct-acting antiviral agents.
Major finding: HCV-specific waiting-list registrations declined by 23% in the 15 months after vs. before FDA approval of simeprevir and sofosbuvir (34.8% vs. 26.8%).
Data source: A review of United Network for Organ Sharing data.
Disclosures: Dr. Perumpail reported having no disclosures.
VIDEO: 12-week HCV retreatment effective if short course fails
SAN FRANCISCO – Can patients who fail short-course treatment for hepatitis C and show high levels of resistance to an antiviral drug still respond to standard 12-week therapy?
“There were initially some data that retreatment might not be as good,” explained Dr. Eleanor Wilson of the University of Maryland, Baltimore.
In the SYNERGY trial, patients underwent short-course therapy with three or four directly acting antivirals. Those who failed the short-course therapies had the opportunity to re-enroll for 12-week standard-of-care therapy. Dr. Wilson and her colleagues studied patients who failed short-course therapy but then underwent 12-week HCV treatment.
In an interview at the annual meeting of the American Association for the Study of Liver Diseases, Dr. Wilson discussed her findings and whether retreatment for 12 weeks was effective, particularly in patients with high levels of resistance to ledipasvir.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – Can patients who fail short-course treatment for hepatitis C and show high levels of resistance to an antiviral drug still respond to standard 12-week therapy?
“There were initially some data that retreatment might not be as good,” explained Dr. Eleanor Wilson of the University of Maryland, Baltimore.
In the SYNERGY trial, patients underwent short-course therapy with three or four directly acting antivirals. Those who failed the short-course therapies had the opportunity to re-enroll for 12-week standard-of-care therapy. Dr. Wilson and her colleagues studied patients who failed short-course therapy but then underwent 12-week HCV treatment.
In an interview at the annual meeting of the American Association for the Study of Liver Diseases, Dr. Wilson discussed her findings and whether retreatment for 12 weeks was effective, particularly in patients with high levels of resistance to ledipasvir.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – Can patients who fail short-course treatment for hepatitis C and show high levels of resistance to an antiviral drug still respond to standard 12-week therapy?
“There were initially some data that retreatment might not be as good,” explained Dr. Eleanor Wilson of the University of Maryland, Baltimore.
In the SYNERGY trial, patients underwent short-course therapy with three or four directly acting antivirals. Those who failed the short-course therapies had the opportunity to re-enroll for 12-week standard-of-care therapy. Dr. Wilson and her colleagues studied patients who failed short-course therapy but then underwent 12-week HCV treatment.
In an interview at the annual meeting of the American Association for the Study of Liver Diseases, Dr. Wilson discussed her findings and whether retreatment for 12 weeks was effective, particularly in patients with high levels of resistance to ledipasvir.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE LIVER MEETING 2015