User login
HCV Hub
AbbVie
acid
addicted
addiction
adolescent
adult sites
Advocacy
advocacy
agitated states
AJO, postsurgical analgesic, knee, replacement, surgery
alcohol
amphetamine
androgen
antibody
apple cider vinegar
assistance
Assistance
association
at home
attorney
audit
ayurvedic
baby
ban
baricitinib
bed bugs
best
bible
bisexual
black
bleach
blog
bulimia nervosa
buy
cannabis
certificate
certification
certified
cervical cancer, concurrent chemoradiotherapy, intravoxel incoherent motion magnetic resonance imaging, MRI, IVIM, diffusion-weighted MRI, DWI
charlie sheen
cheap
cheapest
child
childhood
childlike
children
chronic fatigue syndrome
Cladribine Tablets
cocaine
cock
combination therapies, synergistic antitumor efficacy, pertuzumab, trastuzumab, ipilimumab, nivolumab, palbociclib, letrozole, lapatinib, docetaxel, trametinib, dabrafenib, carflzomib, lenalidomide
contagious
Cortical Lesions
cream
creams
crime
criminal
cure
dangerous
dangers
dasabuvir
Dasabuvir
dead
deadly
death
dementia
dependence
dependent
depression
dermatillomania
die
diet
direct-acting antivirals
Disability
Discount
discount
dog
drink
drug abuse
drug-induced
dying
eastern medicine
eat
ect
eczema
electroconvulsive therapy
electromagnetic therapy
electrotherapy
epa
epilepsy
erectile dysfunction
explosive disorder
fake
Fake-ovir
fatal
fatalities
fatality
fibromyalgia
financial
Financial
fish oil
food
foods
foundation
free
Gabriel Pardo
gaston
general hospital
genetic
geriatric
Giancarlo Comi
gilead
Gilead
glaucoma
Glenn S. Williams
Glenn Williams
Gloria Dalla Costa
gonorrhea
Greedy
greedy
guns
hallucinations
harvoni
Harvoni
herbal
herbs
heroin
herpes
Hidradenitis Suppurativa,
holistic
home
home remedies
home remedy
homeopathic
homeopathy
hydrocortisone
ice
image
images
job
kid
kids
kill
killer
laser
lawsuit
lawyer
ledipasvir
Ledipasvir
lesbian
lesions
lights
liver
lupus
marijuana
melancholic
memory loss
menopausal
mental retardation
military
milk
moisturizers
monoamine oxidase inhibitor drugs
MRI
MS
murder
national
natural
natural cure
natural cures
natural medications
natural medicine
natural medicines
natural remedies
natural remedy
natural treatment
natural treatments
naturally
Needy
needy
Neurology Reviews
neuropathic
nightclub massacre
nightclub shooting
nude
nudity
nutraceuticals
OASIS
oasis
off label
ombitasvir
Ombitasvir
ombitasvir/paritaprevir/ritonavir with dasabuvir
orlando shooting
overactive thyroid gland
overdose
overdosed
Paolo Preziosa
paritaprevir
Paritaprevir
pediatric
pedophile
photo
photos
picture
post partum
postnatal
pregnancy
pregnant
prenatal
prepartum
prison
program
Program
Protest
protest
psychedelics
pulse nightclub
puppy
purchase
purchasing
rape
recall
recreational drug
Rehabilitation
Retinal Measurements
retrograde ejaculation
risperdal
ritonavir
Ritonavir
ritonavir with dasabuvir
robin williams
sales
sasquatch
schizophrenia
seizure
seizures
sex
sexual
sexy
shock treatment
silver
sleep disorders
smoking
sociopath
sofosbuvir
Sofosbuvir
sovaldi
ssri
store
sue
suicidal
suicide
supplements
support
Support
Support Path
teen
teenage
teenagers
Telerehabilitation
testosterone
Th17
Th17:FoxP3+Treg cell ratio
Th22
toxic
toxin
tragedy
treatment resistant
V Pak
vagina
velpatasvir
Viekira Pa
Viekira Pak
viekira pak
violence
virgin
vitamin
VPak
weight loss
withdrawal
wrinkles
xxx
young adult
young adults
zoloft
financial
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
Eradicate HCV in patients with HIV, regardless of fibrosis stage
Eradicating hepatitis C virus in HIV-coinfected patients was associated with a significantly lower risk of diabetes mellitus and possibly chronic renal failure, along with lower rates of deaths, HIV progression, and liver-related events, according to an observational study of 1,625 patients.
“These findings argue for the prescription of HCV therapy regardless of liver fibrosis stage in coinfected patients,” Juan Berenguer, MD, PhD, and his associates at Hospital General Universitario Gregario Marañón, Madrid. Extrahepatic manifestations of HCV infection are numerous and contribute substantially to morbidity and mortality. “To the best of our knowledge, the effect of eradication of HCV on extrahepatic manifestations of HCV has not been systematically studied in HIV/HCV-coinfected patients,” the researchers wrote in Hepatology (Hepatology 2017 Jan 21:doi:10.1002/hep.29071 [Epub ahead of print]).
After a median of 5 years of follow-up, SVR was associated with a 43% decrease in the likelihood of developing diabetes, even after controlling for a host of potential confounders, including Fibrosis-4 score (using 3.25 as the cutoff value), age, sex, history of AIDS, HIV-transmission category, nadir CD4+ T-cell count, antiretroviral therapy, HIV-RNA, HCV genotype, and exposure to specific anti-HIV drugs (adjusted hazard ratio, 0.57; 95% confidence interval, 0.35 to 0.93; P = .02). Sustained viral response also was associated with a lower likelihood of chronic renal failure with borderline statistical significance (aHR, 0.43; 95% CI, 0.17 to 1.09; P = .075).
“In agreement with previous reports from this cohort, we found that treatment response was associated with a decreased hazard of overall and liver-related death, all types of liver-related events, and new AIDS-related conditions,” the researchers noted. These findings underscore the vital importance of HCV therapy for HIV-coinfected patients, regardless of liver fibrosis stage, they emphasized.
The study was funded by Spanish Health Research Funds and AIDS Research Network. The investigators reported having no relevant conflicts of interest.
Eradicating hepatitis C virus in HIV-coinfected patients was associated with a significantly lower risk of diabetes mellitus and possibly chronic renal failure, along with lower rates of deaths, HIV progression, and liver-related events, according to an observational study of 1,625 patients.
“These findings argue for the prescription of HCV therapy regardless of liver fibrosis stage in coinfected patients,” Juan Berenguer, MD, PhD, and his associates at Hospital General Universitario Gregario Marañón, Madrid. Extrahepatic manifestations of HCV infection are numerous and contribute substantially to morbidity and mortality. “To the best of our knowledge, the effect of eradication of HCV on extrahepatic manifestations of HCV has not been systematically studied in HIV/HCV-coinfected patients,” the researchers wrote in Hepatology (Hepatology 2017 Jan 21:doi:10.1002/hep.29071 [Epub ahead of print]).
After a median of 5 years of follow-up, SVR was associated with a 43% decrease in the likelihood of developing diabetes, even after controlling for a host of potential confounders, including Fibrosis-4 score (using 3.25 as the cutoff value), age, sex, history of AIDS, HIV-transmission category, nadir CD4+ T-cell count, antiretroviral therapy, HIV-RNA, HCV genotype, and exposure to specific anti-HIV drugs (adjusted hazard ratio, 0.57; 95% confidence interval, 0.35 to 0.93; P = .02). Sustained viral response also was associated with a lower likelihood of chronic renal failure with borderline statistical significance (aHR, 0.43; 95% CI, 0.17 to 1.09; P = .075).
“In agreement with previous reports from this cohort, we found that treatment response was associated with a decreased hazard of overall and liver-related death, all types of liver-related events, and new AIDS-related conditions,” the researchers noted. These findings underscore the vital importance of HCV therapy for HIV-coinfected patients, regardless of liver fibrosis stage, they emphasized.
The study was funded by Spanish Health Research Funds and AIDS Research Network. The investigators reported having no relevant conflicts of interest.
Eradicating hepatitis C virus in HIV-coinfected patients was associated with a significantly lower risk of diabetes mellitus and possibly chronic renal failure, along with lower rates of deaths, HIV progression, and liver-related events, according to an observational study of 1,625 patients.
“These findings argue for the prescription of HCV therapy regardless of liver fibrosis stage in coinfected patients,” Juan Berenguer, MD, PhD, and his associates at Hospital General Universitario Gregario Marañón, Madrid. Extrahepatic manifestations of HCV infection are numerous and contribute substantially to morbidity and mortality. “To the best of our knowledge, the effect of eradication of HCV on extrahepatic manifestations of HCV has not been systematically studied in HIV/HCV-coinfected patients,” the researchers wrote in Hepatology (Hepatology 2017 Jan 21:doi:10.1002/hep.29071 [Epub ahead of print]).
After a median of 5 years of follow-up, SVR was associated with a 43% decrease in the likelihood of developing diabetes, even after controlling for a host of potential confounders, including Fibrosis-4 score (using 3.25 as the cutoff value), age, sex, history of AIDS, HIV-transmission category, nadir CD4+ T-cell count, antiretroviral therapy, HIV-RNA, HCV genotype, and exposure to specific anti-HIV drugs (adjusted hazard ratio, 0.57; 95% confidence interval, 0.35 to 0.93; P = .02). Sustained viral response also was associated with a lower likelihood of chronic renal failure with borderline statistical significance (aHR, 0.43; 95% CI, 0.17 to 1.09; P = .075).
“In agreement with previous reports from this cohort, we found that treatment response was associated with a decreased hazard of overall and liver-related death, all types of liver-related events, and new AIDS-related conditions,” the researchers noted. These findings underscore the vital importance of HCV therapy for HIV-coinfected patients, regardless of liver fibrosis stage, they emphasized.
The study was funded by Spanish Health Research Funds and AIDS Research Network. The investigators reported having no relevant conflicts of interest.
FROM HEPATOLOGY
Key clinical point. Eradicating hepatitis C virus infection in HIV-coinfected patients is crucial, regardless of fibrosis stage.
Major finding: After a median of 5 years of follow-up, sustained viral response to HCV treatment was associated with a 43% decrease in the likelihood of developing diabetes, even after controlling for fibrosis stage and other potential confounders. Reaching SVR also was associated with decreased rates of renal failure, HIV progression, and mortality.
Data source: An observational study of 1,625 patients with HIV and hepatitis C virus coinfection.
Disclosures: The study was funded by Spanish Health Research Funds and AIDS Research Network. The investigators reported having no relevant conflicts of interest.
Initial HCV test results are false positive in almost half of general population
Nearly half of patients in the general population who test positive for hepatitis C virus (HCV) do not have the disease, according to Dr. Anne Moorman and her associates.
From a sample of 22,359 National Health and Nutrition Examination Study participants, 479 people received positive HCV antibody test results from 2007 to 2012. Of this group, 477 participants underwent further follow-up testing using a recombinant immunoblot assay. RIBA testing confirmed positive test results for 323 participants, while 105 patients received negative test results and 49 received indeterminate test results.
“False-positive antibody assays may occur with great frequency, emphasizing the need for “reflex” HCV RNA testing to ascertain current infection status,” the investigators noted.
Find the full study in the Journal of Clinical Virology (doi: 10.1016/j.jcv.2017.01.007).
Nearly half of patients in the general population who test positive for hepatitis C virus (HCV) do not have the disease, according to Dr. Anne Moorman and her associates.
From a sample of 22,359 National Health and Nutrition Examination Study participants, 479 people received positive HCV antibody test results from 2007 to 2012. Of this group, 477 participants underwent further follow-up testing using a recombinant immunoblot assay. RIBA testing confirmed positive test results for 323 participants, while 105 patients received negative test results and 49 received indeterminate test results.
“False-positive antibody assays may occur with great frequency, emphasizing the need for “reflex” HCV RNA testing to ascertain current infection status,” the investigators noted.
Find the full study in the Journal of Clinical Virology (doi: 10.1016/j.jcv.2017.01.007).
Nearly half of patients in the general population who test positive for hepatitis C virus (HCV) do not have the disease, according to Dr. Anne Moorman and her associates.
From a sample of 22,359 National Health and Nutrition Examination Study participants, 479 people received positive HCV antibody test results from 2007 to 2012. Of this group, 477 participants underwent further follow-up testing using a recombinant immunoblot assay. RIBA testing confirmed positive test results for 323 participants, while 105 patients received negative test results and 49 received indeterminate test results.
“False-positive antibody assays may occur with great frequency, emphasizing the need for “reflex” HCV RNA testing to ascertain current infection status,” the investigators noted.
Find the full study in the Journal of Clinical Virology (doi: 10.1016/j.jcv.2017.01.007).
FROM JOURNAL OF CLINICAL VIROLOGY
The Liver Meeting 2016 debrief – key abstracts
BOSTON – Amid a plethora of quality research, several abstracts stood out at the annual meeting of the American Association for the Study of Liver Diseases, Arun J. Sanyal, MD, said during the final debrief.
He focused first on nonalcoholic fatty liver disease (NAFLD), which has lacked rigorous studies of disease evolution. Consequently, “current therapeutic development is based on small retrospective data sets with heterogenous populations,” Dr. Sanyal said. Therefore, he and his associates correlated serial biopsies with clinical data (abstract 37). The results confirmed the waxing and waning nature of NAFLD and linked regressing or progressive fibrosis to several factors, including NAFLD Disease Activity score (NAS). NAFLD and nonalcoholic steatohepatitis (NASH) are “not two different diseases, it’s the same disease,” Dr. Sanyal said. “Establishing disease activity as a driver of disease progression is highly relevant for development of noninvasive biomarkers, and also gives us a foundation for the development of clinical trials in this space.”
Several studies of NASH biomarkers yielded notable results at the meeting. In the largest study to date of circulating microRNAs as markers of NASH, (LB2) the miRNAs 34a, 122a, and 200a distinguished patients with and without NAS scores of at least 4 and at least stage 2 fibrosis with areas under the receiver operating characteristic curve (AUROC) between 0.59 and 0.80. “MicroRNAs appear promising, but likely need to be combined with additional biomarkers,” Dr. Sanyal said.
He also noted a study (abstract 40) in which metabolomics of liquid biopsies comprehensively evaluated NAFLD, including fibrosis stage, with AUROCs up to 0.95. Metabolomics “holds promise as a diagnostic tool that can be operationalized for point-of-care testing,” he said.
When it comes to NAFLD, hepatologists “often struggle with what to tell our patients about alcohol,” Dr. Sanyal said. To help clarify the issue, abstract 31 compared NAFLD patients who did or did not report habitually consuming up to two drinks a day in formal prospective questionnaires. After adjustment for baseline histology, abstainers and modest drinkers did not differ on any measure of histologic change, except that abstainers had a greater decrease in steatosis on follow-up biopsy. These findings negate several retrospective studies by suggesting that alcohol consumption does not positively affect the trajectory of NAFLD, Dr. Sanyal concluded.
Many new compounds for treating NASH are in early development, he noted. Among those further along the pipeline, the immunomodulator and CCR2/CCR5 inhibitor cenicriviroc (CVC) missed its primary endpoint (improved NAS and no worsening of fibrosis) but was associated with significantly improved fibrosis without worsening of NASH in the phase 2b CENTAUR study (LB1).
“We also saw highly promising evidence for the effects of ASK1 [apoptosis signal regulating kinase] inhibition on hepatic fibrosis and disease activity in NASH,” Dr. Sanyal added. In a randomized phase II trial (LB3), the ASK1 inhibitor GS-4997 was associated with significant improvement in fibrosis without worsening of NASH when given in combination with simtuzumab, and also improved liver stiffness and magnetic resonance imaging–estimated proton density fat fraction (MRI-PDFF). “These very promising and exciting results need confirmation in more advanced, placebo-controlled trials,” Dr. Sanyal said.
Studies of alcohol use disorders of the liver confirmed that prednisolone has marginal benefits, that the benefits of steroids in general are offset by sepsis, and that pentoxifylline produced no mortality benefit, Dr. Sanyal noted. In studies of primary biliary cirrhosis, the farnesoid-X receptor agonist obeticholic acid (OCA), which was approved by the Food and Drug Administration in 2016, was associated with significantly improved AST to Platelet Ratio Index (APRI) and liver stiffness measures by transient elastography at doses of 10 mg or titrated from 5 mg to 10 mg, with or without ursodeoxycholic acid (abstract 209). In another study, patients with PBC who received norUDCA, a side chain–shortened version of UDCA, experienced decreases in serum ALP levels that were dose dependent and differed significantly from trends in the placebo group (abstract 210).
In another study, the investigational ileal bile acid transporter inhibitor GSK2330672 was associated with significant reductions in itch, compared with placebo, and with lower serum bile acids among pruritic PBC patients (abstract 205). Treatment was associated with diarrhea, but it was usually mild and transient.
Dr. Sanyal concluded by reviewing several studies of cirrhosis and hepatic encephalopathy. In a prospective randomized controlled trial (abstract 247), lactulose with albumin significantly outperformed lactulose monotherapy for reversing hepatic encephalopathy, reducing hospital stays, and preventing mortality, especially sepsis-related death.
In another multicenter, 24-week, phase IV open-label study (abstract 248), 25% of patients experienced breakthrough hepatic encephalopathy when treated with rifaximin monotherapy, compared with only 14% of patients who received both rifaximin and lactulose.
Finally, in a phase II trial (abstract 2064), rifaximin immediate-release (40 mg) significantly outperformed placebo in terms of cirrhosis-related mortality, hospitalizations for cirrhosis, and breakthrough hepatic encephalopathy. The takeaways? “Use albumin with lactulose for acute hepatic encephalopathy,” Dr. Sanyal said. “Rifaximin with lactulose is better than rifaximin alone for secondary prophylaxis, and rifaximin immediate-release may decrease the need for hospitalization and the first bout of hepatic encephalopathy.”
The Liver Meeting next convenes October 20-24, 2017, in Washington, D.C.
Dr. Sanyal disclosed ties to Genfit, NewCo, Akarna, Elsevier, UptoDate, Novartis, Pfizer, Lilly, Astra Zeneca, and a number of other companies.
BOSTON – Amid a plethora of quality research, several abstracts stood out at the annual meeting of the American Association for the Study of Liver Diseases, Arun J. Sanyal, MD, said during the final debrief.
He focused first on nonalcoholic fatty liver disease (NAFLD), which has lacked rigorous studies of disease evolution. Consequently, “current therapeutic development is based on small retrospective data sets with heterogenous populations,” Dr. Sanyal said. Therefore, he and his associates correlated serial biopsies with clinical data (abstract 37). The results confirmed the waxing and waning nature of NAFLD and linked regressing or progressive fibrosis to several factors, including NAFLD Disease Activity score (NAS). NAFLD and nonalcoholic steatohepatitis (NASH) are “not two different diseases, it’s the same disease,” Dr. Sanyal said. “Establishing disease activity as a driver of disease progression is highly relevant for development of noninvasive biomarkers, and also gives us a foundation for the development of clinical trials in this space.”
Several studies of NASH biomarkers yielded notable results at the meeting. In the largest study to date of circulating microRNAs as markers of NASH, (LB2) the miRNAs 34a, 122a, and 200a distinguished patients with and without NAS scores of at least 4 and at least stage 2 fibrosis with areas under the receiver operating characteristic curve (AUROC) between 0.59 and 0.80. “MicroRNAs appear promising, but likely need to be combined with additional biomarkers,” Dr. Sanyal said.
He also noted a study (abstract 40) in which metabolomics of liquid biopsies comprehensively evaluated NAFLD, including fibrosis stage, with AUROCs up to 0.95. Metabolomics “holds promise as a diagnostic tool that can be operationalized for point-of-care testing,” he said.
When it comes to NAFLD, hepatologists “often struggle with what to tell our patients about alcohol,” Dr. Sanyal said. To help clarify the issue, abstract 31 compared NAFLD patients who did or did not report habitually consuming up to two drinks a day in formal prospective questionnaires. After adjustment for baseline histology, abstainers and modest drinkers did not differ on any measure of histologic change, except that abstainers had a greater decrease in steatosis on follow-up biopsy. These findings negate several retrospective studies by suggesting that alcohol consumption does not positively affect the trajectory of NAFLD, Dr. Sanyal concluded.
Many new compounds for treating NASH are in early development, he noted. Among those further along the pipeline, the immunomodulator and CCR2/CCR5 inhibitor cenicriviroc (CVC) missed its primary endpoint (improved NAS and no worsening of fibrosis) but was associated with significantly improved fibrosis without worsening of NASH in the phase 2b CENTAUR study (LB1).
“We also saw highly promising evidence for the effects of ASK1 [apoptosis signal regulating kinase] inhibition on hepatic fibrosis and disease activity in NASH,” Dr. Sanyal added. In a randomized phase II trial (LB3), the ASK1 inhibitor GS-4997 was associated with significant improvement in fibrosis without worsening of NASH when given in combination with simtuzumab, and also improved liver stiffness and magnetic resonance imaging–estimated proton density fat fraction (MRI-PDFF). “These very promising and exciting results need confirmation in more advanced, placebo-controlled trials,” Dr. Sanyal said.
Studies of alcohol use disorders of the liver confirmed that prednisolone has marginal benefits, that the benefits of steroids in general are offset by sepsis, and that pentoxifylline produced no mortality benefit, Dr. Sanyal noted. In studies of primary biliary cirrhosis, the farnesoid-X receptor agonist obeticholic acid (OCA), which was approved by the Food and Drug Administration in 2016, was associated with significantly improved AST to Platelet Ratio Index (APRI) and liver stiffness measures by transient elastography at doses of 10 mg or titrated from 5 mg to 10 mg, with or without ursodeoxycholic acid (abstract 209). In another study, patients with PBC who received norUDCA, a side chain–shortened version of UDCA, experienced decreases in serum ALP levels that were dose dependent and differed significantly from trends in the placebo group (abstract 210).
In another study, the investigational ileal bile acid transporter inhibitor GSK2330672 was associated with significant reductions in itch, compared with placebo, and with lower serum bile acids among pruritic PBC patients (abstract 205). Treatment was associated with diarrhea, but it was usually mild and transient.
Dr. Sanyal concluded by reviewing several studies of cirrhosis and hepatic encephalopathy. In a prospective randomized controlled trial (abstract 247), lactulose with albumin significantly outperformed lactulose monotherapy for reversing hepatic encephalopathy, reducing hospital stays, and preventing mortality, especially sepsis-related death.
In another multicenter, 24-week, phase IV open-label study (abstract 248), 25% of patients experienced breakthrough hepatic encephalopathy when treated with rifaximin monotherapy, compared with only 14% of patients who received both rifaximin and lactulose.
Finally, in a phase II trial (abstract 2064), rifaximin immediate-release (40 mg) significantly outperformed placebo in terms of cirrhosis-related mortality, hospitalizations for cirrhosis, and breakthrough hepatic encephalopathy. The takeaways? “Use albumin with lactulose for acute hepatic encephalopathy,” Dr. Sanyal said. “Rifaximin with lactulose is better than rifaximin alone for secondary prophylaxis, and rifaximin immediate-release may decrease the need for hospitalization and the first bout of hepatic encephalopathy.”
The Liver Meeting next convenes October 20-24, 2017, in Washington, D.C.
Dr. Sanyal disclosed ties to Genfit, NewCo, Akarna, Elsevier, UptoDate, Novartis, Pfizer, Lilly, Astra Zeneca, and a number of other companies.
BOSTON – Amid a plethora of quality research, several abstracts stood out at the annual meeting of the American Association for the Study of Liver Diseases, Arun J. Sanyal, MD, said during the final debrief.
He focused first on nonalcoholic fatty liver disease (NAFLD), which has lacked rigorous studies of disease evolution. Consequently, “current therapeutic development is based on small retrospective data sets with heterogenous populations,” Dr. Sanyal said. Therefore, he and his associates correlated serial biopsies with clinical data (abstract 37). The results confirmed the waxing and waning nature of NAFLD and linked regressing or progressive fibrosis to several factors, including NAFLD Disease Activity score (NAS). NAFLD and nonalcoholic steatohepatitis (NASH) are “not two different diseases, it’s the same disease,” Dr. Sanyal said. “Establishing disease activity as a driver of disease progression is highly relevant for development of noninvasive biomarkers, and also gives us a foundation for the development of clinical trials in this space.”
Several studies of NASH biomarkers yielded notable results at the meeting. In the largest study to date of circulating microRNAs as markers of NASH, (LB2) the miRNAs 34a, 122a, and 200a distinguished patients with and without NAS scores of at least 4 and at least stage 2 fibrosis with areas under the receiver operating characteristic curve (AUROC) between 0.59 and 0.80. “MicroRNAs appear promising, but likely need to be combined with additional biomarkers,” Dr. Sanyal said.
He also noted a study (abstract 40) in which metabolomics of liquid biopsies comprehensively evaluated NAFLD, including fibrosis stage, with AUROCs up to 0.95. Metabolomics “holds promise as a diagnostic tool that can be operationalized for point-of-care testing,” he said.
When it comes to NAFLD, hepatologists “often struggle with what to tell our patients about alcohol,” Dr. Sanyal said. To help clarify the issue, abstract 31 compared NAFLD patients who did or did not report habitually consuming up to two drinks a day in formal prospective questionnaires. After adjustment for baseline histology, abstainers and modest drinkers did not differ on any measure of histologic change, except that abstainers had a greater decrease in steatosis on follow-up biopsy. These findings negate several retrospective studies by suggesting that alcohol consumption does not positively affect the trajectory of NAFLD, Dr. Sanyal concluded.
Many new compounds for treating NASH are in early development, he noted. Among those further along the pipeline, the immunomodulator and CCR2/CCR5 inhibitor cenicriviroc (CVC) missed its primary endpoint (improved NAS and no worsening of fibrosis) but was associated with significantly improved fibrosis without worsening of NASH in the phase 2b CENTAUR study (LB1).
“We also saw highly promising evidence for the effects of ASK1 [apoptosis signal regulating kinase] inhibition on hepatic fibrosis and disease activity in NASH,” Dr. Sanyal added. In a randomized phase II trial (LB3), the ASK1 inhibitor GS-4997 was associated with significant improvement in fibrosis without worsening of NASH when given in combination with simtuzumab, and also improved liver stiffness and magnetic resonance imaging–estimated proton density fat fraction (MRI-PDFF). “These very promising and exciting results need confirmation in more advanced, placebo-controlled trials,” Dr. Sanyal said.
Studies of alcohol use disorders of the liver confirmed that prednisolone has marginal benefits, that the benefits of steroids in general are offset by sepsis, and that pentoxifylline produced no mortality benefit, Dr. Sanyal noted. In studies of primary biliary cirrhosis, the farnesoid-X receptor agonist obeticholic acid (OCA), which was approved by the Food and Drug Administration in 2016, was associated with significantly improved AST to Platelet Ratio Index (APRI) and liver stiffness measures by transient elastography at doses of 10 mg or titrated from 5 mg to 10 mg, with or without ursodeoxycholic acid (abstract 209). In another study, patients with PBC who received norUDCA, a side chain–shortened version of UDCA, experienced decreases in serum ALP levels that were dose dependent and differed significantly from trends in the placebo group (abstract 210).
In another study, the investigational ileal bile acid transporter inhibitor GSK2330672 was associated with significant reductions in itch, compared with placebo, and with lower serum bile acids among pruritic PBC patients (abstract 205). Treatment was associated with diarrhea, but it was usually mild and transient.
Dr. Sanyal concluded by reviewing several studies of cirrhosis and hepatic encephalopathy. In a prospective randomized controlled trial (abstract 247), lactulose with albumin significantly outperformed lactulose monotherapy for reversing hepatic encephalopathy, reducing hospital stays, and preventing mortality, especially sepsis-related death.
In another multicenter, 24-week, phase IV open-label study (abstract 248), 25% of patients experienced breakthrough hepatic encephalopathy when treated with rifaximin monotherapy, compared with only 14% of patients who received both rifaximin and lactulose.
Finally, in a phase II trial (abstract 2064), rifaximin immediate-release (40 mg) significantly outperformed placebo in terms of cirrhosis-related mortality, hospitalizations for cirrhosis, and breakthrough hepatic encephalopathy. The takeaways? “Use albumin with lactulose for acute hepatic encephalopathy,” Dr. Sanyal said. “Rifaximin with lactulose is better than rifaximin alone for secondary prophylaxis, and rifaximin immediate-release may decrease the need for hospitalization and the first bout of hepatic encephalopathy.”
The Liver Meeting next convenes October 20-24, 2017, in Washington, D.C.
Dr. Sanyal disclosed ties to Genfit, NewCo, Akarna, Elsevier, UptoDate, Novartis, Pfizer, Lilly, Astra Zeneca, and a number of other companies.
AT THE LIVER MEETING 2016
HCV patients with early-stage hepatocellular carcinoma can achieve SVR
BOSTON – Among patients with hepatocellular carcinoma (HCC), rates of sustained viral response (SVR) to direct-acting regimens for hepatitis C virus were 79% for genotype 1, 69% for genotype 2, and 47% for genotype 3 infections, reported George N. Ioannou, MD.
“These rates are lower than in patients who do not have hepatocellular carcinoma [HCC], but are still remarkably high,” Dr. Ioannou said during an oral presentation at the annual meeting of the American Association for the Study of Liver Diseases. “Antiviral therapy should be considered in patients with early-stage hepatocellular carcinoma, ideally after adequate locoregional treatments.”
The study included Veterans Affairs Health Care System data on 17,487 recipients of direct-acting anti-HCV regimens. When patients did not have HCC, SVR rates were 93% for genotype 1 infection, 87% for genotype 2 (GT2), and 76% for GT3. Among the 624 (3.6%) patients with a history of HCC, 142 underwent antiviral treatment after transplantation and 482 received other types of cancer therapy.
Why HCC is associated with lower SVR in HCV patients remains unclear, Dr. Ioannou noted. Age does not seem to explain the effect, and neither does sex, race, or ethnicity; cirrhosis or decompensated cirrhosis; renal disease; diabetes; HCV viral load; genotype or subgenotype; HCV regimen; or treatment experience, he said.
Dr. Ioannou noted several study limitations. Nine percent of patients lacked data on SVR, and the imputation to correct for this lowered SVR rates by about 1%-2%. The dataset also did not include information on HCC tumor size or number, and the researchers have not yet examined how antiviral therapy affects the likelihood of de novo HCC, recurrent HCC, or progression of cirrhosis and liver dysfunction.
The Veterans Affairs Office of Research and Development sponsored the study. Dr. Ioannou had no disclosures.
BOSTON – Among patients with hepatocellular carcinoma (HCC), rates of sustained viral response (SVR) to direct-acting regimens for hepatitis C virus were 79% for genotype 1, 69% for genotype 2, and 47% for genotype 3 infections, reported George N. Ioannou, MD.
“These rates are lower than in patients who do not have hepatocellular carcinoma [HCC], but are still remarkably high,” Dr. Ioannou said during an oral presentation at the annual meeting of the American Association for the Study of Liver Diseases. “Antiviral therapy should be considered in patients with early-stage hepatocellular carcinoma, ideally after adequate locoregional treatments.”
The study included Veterans Affairs Health Care System data on 17,487 recipients of direct-acting anti-HCV regimens. When patients did not have HCC, SVR rates were 93% for genotype 1 infection, 87% for genotype 2 (GT2), and 76% for GT3. Among the 624 (3.6%) patients with a history of HCC, 142 underwent antiviral treatment after transplantation and 482 received other types of cancer therapy.
Why HCC is associated with lower SVR in HCV patients remains unclear, Dr. Ioannou noted. Age does not seem to explain the effect, and neither does sex, race, or ethnicity; cirrhosis or decompensated cirrhosis; renal disease; diabetes; HCV viral load; genotype or subgenotype; HCV regimen; or treatment experience, he said.
Dr. Ioannou noted several study limitations. Nine percent of patients lacked data on SVR, and the imputation to correct for this lowered SVR rates by about 1%-2%. The dataset also did not include information on HCC tumor size or number, and the researchers have not yet examined how antiviral therapy affects the likelihood of de novo HCC, recurrent HCC, or progression of cirrhosis and liver dysfunction.
The Veterans Affairs Office of Research and Development sponsored the study. Dr. Ioannou had no disclosures.
BOSTON – Among patients with hepatocellular carcinoma (HCC), rates of sustained viral response (SVR) to direct-acting regimens for hepatitis C virus were 79% for genotype 1, 69% for genotype 2, and 47% for genotype 3 infections, reported George N. Ioannou, MD.
“These rates are lower than in patients who do not have hepatocellular carcinoma [HCC], but are still remarkably high,” Dr. Ioannou said during an oral presentation at the annual meeting of the American Association for the Study of Liver Diseases. “Antiviral therapy should be considered in patients with early-stage hepatocellular carcinoma, ideally after adequate locoregional treatments.”
The study included Veterans Affairs Health Care System data on 17,487 recipients of direct-acting anti-HCV regimens. When patients did not have HCC, SVR rates were 93% for genotype 1 infection, 87% for genotype 2 (GT2), and 76% for GT3. Among the 624 (3.6%) patients with a history of HCC, 142 underwent antiviral treatment after transplantation and 482 received other types of cancer therapy.
Why HCC is associated with lower SVR in HCV patients remains unclear, Dr. Ioannou noted. Age does not seem to explain the effect, and neither does sex, race, or ethnicity; cirrhosis or decompensated cirrhosis; renal disease; diabetes; HCV viral load; genotype or subgenotype; HCV regimen; or treatment experience, he said.
Dr. Ioannou noted several study limitations. Nine percent of patients lacked data on SVR, and the imputation to correct for this lowered SVR rates by about 1%-2%. The dataset also did not include information on HCC tumor size or number, and the researchers have not yet examined how antiviral therapy affects the likelihood of de novo HCC, recurrent HCC, or progression of cirrhosis and liver dysfunction.
The Veterans Affairs Office of Research and Development sponsored the study. Dr. Ioannou had no disclosures.
AT THE LIVER MEETING
Key clinical point: Consider direct-acting antiviral therapy in HCV-infected patients with early-stage HCC.
Major finding: Rates of sustained viral response were 79% in HCC patients with GT1 HCV infection, 69% in GT2 patients, and 47% in GT3 patients.
Data source: An analysis of Veterans Affairs Health Care System data on 17,487 recipients of direct-acting antiviral regimens, including 624 patients with HCC.
Disclosures: The Veterans Affairs Office of Research and Development sponsored the study.
Tumor boards linked to improved survival in hepatocellular carcinoma
BOSTON – Veterans were about 13% less likely to die within 5 years of hepatocellular carcinoma diagnosis when multidisciplinary tumor boards managed their care than if they did not, according to a large, multicenter observational study.
Seeing a hepatologist or surgeon within 30 days of diagnosis also significantly improved 5-year overall survival, even after controlling for age, race, Charlson-Deyo comorbidity index, Barcelona Clinic Liver Cancer (BCLC) stage, academic center and geographic region of care, and the distance patients lived from the nearest Veterans Affairs transplant center, Marina Serper, MD, reported at the annual meeting of the American Association for the Study of Liver Diseases. “More studies are needed to understand how to best use multidisciplinary tumor boards to improve the care of patients with hepatocellular carcinoma,” she said.
Outcomes data for hepatocellular carcinoma mostly come from clinical trials; transplant centers; and Surveillance, Epidemiology, and End Results-Medicare analyses, noted Dr. Serper of the University of Pennsylvania in Philadelphia.
For a better look at veterans, she and her associates combined administrative, laboratory, and death data with medical chart reviews and information from the Organ Procurement and Transplantation Network’s Standard Transplant Analysis and Research file. The initial cohort included more than 6,800 veterans whose ICD-9CM diagnosis code indicated a malignant hepatic neoplasm. Excluding patients with neoplasms such as cholangiocarcinoma and those managed outside the VA left 3,989 VA patients with hepatocellular carcinoma.
In the multivariable analysis, use of multidisciplinary tumor boards was associated with a statistically significant 13% improvement in 5-year overall survival (hazard ratio, 0.87; 95% confidence interval, 0.81-0.94; P less than .001). Improved survival also was linked with seeing certain specialists within 30 days of diagnosis, including hepatologists (HR, 0.77; P less than .001) and surgeons (HR, 0.72; P less than .001). Consulting with a hepatologist within 30 days of diagnosis, however, did not improve the chances of receiving curative therapy, such as liver transplantation, resection, local ablation, transarterial chemoembolization, or Y-90 radioembolization.
Care also varied substantially geographically and by academic affiliation, Dr. Serper noted. “Treatment of hepatocellular carcinoma is complex, as it depends as much on liver function as it does on tumor staging,” she emphasized. “Studies to improve multidisciplinary approaches for hepatocellular carcinoma in the community are needed to increase rates of curative therapy and improve clinical outcomes.”
Patients in this study averaged 62 years of age at diagnosis, 54% were white, 36% were within Milan criteria, and 45% had a Child-Turcotte-Pugh score of B or higher. Nearly 18% had macrovascular invasion at diagnosis, and 7% had metastatic disease. Nearly two-thirds of patients were BCLC stage A or B at diagnosis, and more than a third had underlying alcohol misuse and chronic hepatitis C virus infection.
The work was funded by unrestricted grants from Bayer Healthcare Pharmaceuticals and the VA’s HIV, Hepatitis and Public Health Pathogens Programs. The investigators had no relevant financial disclosures.
BOSTON – Veterans were about 13% less likely to die within 5 years of hepatocellular carcinoma diagnosis when multidisciplinary tumor boards managed their care than if they did not, according to a large, multicenter observational study.
Seeing a hepatologist or surgeon within 30 days of diagnosis also significantly improved 5-year overall survival, even after controlling for age, race, Charlson-Deyo comorbidity index, Barcelona Clinic Liver Cancer (BCLC) stage, academic center and geographic region of care, and the distance patients lived from the nearest Veterans Affairs transplant center, Marina Serper, MD, reported at the annual meeting of the American Association for the Study of Liver Diseases. “More studies are needed to understand how to best use multidisciplinary tumor boards to improve the care of patients with hepatocellular carcinoma,” she said.
Outcomes data for hepatocellular carcinoma mostly come from clinical trials; transplant centers; and Surveillance, Epidemiology, and End Results-Medicare analyses, noted Dr. Serper of the University of Pennsylvania in Philadelphia.
For a better look at veterans, she and her associates combined administrative, laboratory, and death data with medical chart reviews and information from the Organ Procurement and Transplantation Network’s Standard Transplant Analysis and Research file. The initial cohort included more than 6,800 veterans whose ICD-9CM diagnosis code indicated a malignant hepatic neoplasm. Excluding patients with neoplasms such as cholangiocarcinoma and those managed outside the VA left 3,989 VA patients with hepatocellular carcinoma.
In the multivariable analysis, use of multidisciplinary tumor boards was associated with a statistically significant 13% improvement in 5-year overall survival (hazard ratio, 0.87; 95% confidence interval, 0.81-0.94; P less than .001). Improved survival also was linked with seeing certain specialists within 30 days of diagnosis, including hepatologists (HR, 0.77; P less than .001) and surgeons (HR, 0.72; P less than .001). Consulting with a hepatologist within 30 days of diagnosis, however, did not improve the chances of receiving curative therapy, such as liver transplantation, resection, local ablation, transarterial chemoembolization, or Y-90 radioembolization.
Care also varied substantially geographically and by academic affiliation, Dr. Serper noted. “Treatment of hepatocellular carcinoma is complex, as it depends as much on liver function as it does on tumor staging,” she emphasized. “Studies to improve multidisciplinary approaches for hepatocellular carcinoma in the community are needed to increase rates of curative therapy and improve clinical outcomes.”
Patients in this study averaged 62 years of age at diagnosis, 54% were white, 36% were within Milan criteria, and 45% had a Child-Turcotte-Pugh score of B or higher. Nearly 18% had macrovascular invasion at diagnosis, and 7% had metastatic disease. Nearly two-thirds of patients were BCLC stage A or B at diagnosis, and more than a third had underlying alcohol misuse and chronic hepatitis C virus infection.
The work was funded by unrestricted grants from Bayer Healthcare Pharmaceuticals and the VA’s HIV, Hepatitis and Public Health Pathogens Programs. The investigators had no relevant financial disclosures.
BOSTON – Veterans were about 13% less likely to die within 5 years of hepatocellular carcinoma diagnosis when multidisciplinary tumor boards managed their care than if they did not, according to a large, multicenter observational study.
Seeing a hepatologist or surgeon within 30 days of diagnosis also significantly improved 5-year overall survival, even after controlling for age, race, Charlson-Deyo comorbidity index, Barcelona Clinic Liver Cancer (BCLC) stage, academic center and geographic region of care, and the distance patients lived from the nearest Veterans Affairs transplant center, Marina Serper, MD, reported at the annual meeting of the American Association for the Study of Liver Diseases. “More studies are needed to understand how to best use multidisciplinary tumor boards to improve the care of patients with hepatocellular carcinoma,” she said.
Outcomes data for hepatocellular carcinoma mostly come from clinical trials; transplant centers; and Surveillance, Epidemiology, and End Results-Medicare analyses, noted Dr. Serper of the University of Pennsylvania in Philadelphia.
For a better look at veterans, she and her associates combined administrative, laboratory, and death data with medical chart reviews and information from the Organ Procurement and Transplantation Network’s Standard Transplant Analysis and Research file. The initial cohort included more than 6,800 veterans whose ICD-9CM diagnosis code indicated a malignant hepatic neoplasm. Excluding patients with neoplasms such as cholangiocarcinoma and those managed outside the VA left 3,989 VA patients with hepatocellular carcinoma.
In the multivariable analysis, use of multidisciplinary tumor boards was associated with a statistically significant 13% improvement in 5-year overall survival (hazard ratio, 0.87; 95% confidence interval, 0.81-0.94; P less than .001). Improved survival also was linked with seeing certain specialists within 30 days of diagnosis, including hepatologists (HR, 0.77; P less than .001) and surgeons (HR, 0.72; P less than .001). Consulting with a hepatologist within 30 days of diagnosis, however, did not improve the chances of receiving curative therapy, such as liver transplantation, resection, local ablation, transarterial chemoembolization, or Y-90 radioembolization.
Care also varied substantially geographically and by academic affiliation, Dr. Serper noted. “Treatment of hepatocellular carcinoma is complex, as it depends as much on liver function as it does on tumor staging,” she emphasized. “Studies to improve multidisciplinary approaches for hepatocellular carcinoma in the community are needed to increase rates of curative therapy and improve clinical outcomes.”
Patients in this study averaged 62 years of age at diagnosis, 54% were white, 36% were within Milan criteria, and 45% had a Child-Turcotte-Pugh score of B or higher. Nearly 18% had macrovascular invasion at diagnosis, and 7% had metastatic disease. Nearly two-thirds of patients were BCLC stage A or B at diagnosis, and more than a third had underlying alcohol misuse and chronic hepatitis C virus infection.
The work was funded by unrestricted grants from Bayer Healthcare Pharmaceuticals and the VA’s HIV, Hepatitis and Public Health Pathogens Programs. The investigators had no relevant financial disclosures.
AT THE LIVER MEETING 2016
Key clinical point: The use of multidisciplinary tumor boards was associated with significantly improved overall survival in patients with hepatocellular carcinoma.
Major finding: The risk of death within 5 years dropped by about 13% (hazard ratio, 0.87; 95% confidence interval, 0.81-0.94; P less than .001).
Data source: A retrospective study of 3,989 Veterans Affairs patients with hepatocellular carcinoma.
Disclosures: The work was funded by unrestricted grants from Bayer Healthcare Pharmaceuticals and the VA’s HIV, Hepatitis and Public Health Pathogens Programs. The investigators had no relevant financial disclosures.
VIDEO: PBC patients with compensated cirrhosis fare well on obeticholic acid
BOSTON – Patients with primary biliary cholangitis (PBC) who have compensated cirrhosis fared just as well on obeticholic acid (OCA) as did PBC patients without cirrhosis, according to an analysis of data from POISE, the pivotal clinical trial for approval of OCA for PBC.
The POISE trial included 36 individuals with PBC and compensated cirrhosis, since cirrhosis “is an endpoint for virtually all liver diseases,” John Vierling, MD, said in a video interview at the meeting.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
To see how this group fared, Dr. Vierling and his coinvestigators performed a post hoc analysis of the POISE data to examine OCA’s safety and efficacy for patients with compensated cirrhosis. Patients with decompensated cirrhosis were not included in the trial.
Dr. Vierling, chief of hepatology at Baylor College of Medicine, Houston, noted that investigators worked hard to set the bar high for inclusion in the group with cirrhosis, to achieve very high specificity. “We did this by using very stringent criteria of liver biopsy, or transient elastography adjusted for a very high range of kilopascals required to diagnose cirrhosis in cholestatic patients,” he said. To be included, patients also had to have elevated total bilirubin levels and a baseline alkaline phosphatase level greater than five times the upper limit of normal.
Statistically, the patients were evenly distributed across the placebo arm and the two treatment arms, one of which dosed OCA at 10 mg/day; the other treatment arm had flexible dosing at 5-10 mg/day.
The POISE trial used a composite primary efficacy endpoint of achieving an alkaline phosphatase (ALP) less than 1.67 times the upper limit of normal, with total bilirubin within normal limits, and at least a 15% reduction in ALP.
“Significantly more OCA-treated patients with cirrhosis achieved the primary composite endpoint compared to placebo,” Dr. Vierling and his coauthors wrote in a poster presented at the annual meeting for the American Association for the Study of Liver Diseases. The difference was individually significant for all three values that made up the composite primary endpoint as well.
Secondary endpoints included gamma-glutamyltransferase, alanine aminotrasferase, and aspartate aminotransferase, all of which were significantly reduced among patients taking OCA. Patients on placebo saw these values rise over the time period of the study.
There were no new safety signals seen in the post hoc analysis of the group with cirrhosis that were not seen in the trial at large, said Dr. Vierling. Two individuals in the subgroup dropped out of the trial because of pruritis, a similar proportion to that seen in the full trial population.
The drug’s manufacturer, Intercept Pharmaceuticals, is working with the Food and Drug Administration to establish appropriate doses and intervals for obeticholic acid so it may be used safely in individuals with decompensated cirrhosis, said Dr. Vierling.
Obeticholic acid, a farnesoid-X receptor agonist, is an approved agent to use as add-on therapy to ursodeoxycholic acid (UDCA), or as monotherapy for patients who can’t tolerate UDCA.
Dr. Vierling disclosed financial relationships with Intercept Pharmaceuticals and with several other pharmaceutical companies. The study was funded by Intercept Pharmaceuticals.
koakes@frontlinemedcom.com
On Twitter @karioakes
BOSTON – Patients with primary biliary cholangitis (PBC) who have compensated cirrhosis fared just as well on obeticholic acid (OCA) as did PBC patients without cirrhosis, according to an analysis of data from POISE, the pivotal clinical trial for approval of OCA for PBC.
The POISE trial included 36 individuals with PBC and compensated cirrhosis, since cirrhosis “is an endpoint for virtually all liver diseases,” John Vierling, MD, said in a video interview at the meeting.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
To see how this group fared, Dr. Vierling and his coinvestigators performed a post hoc analysis of the POISE data to examine OCA’s safety and efficacy for patients with compensated cirrhosis. Patients with decompensated cirrhosis were not included in the trial.
Dr. Vierling, chief of hepatology at Baylor College of Medicine, Houston, noted that investigators worked hard to set the bar high for inclusion in the group with cirrhosis, to achieve very high specificity. “We did this by using very stringent criteria of liver biopsy, or transient elastography adjusted for a very high range of kilopascals required to diagnose cirrhosis in cholestatic patients,” he said. To be included, patients also had to have elevated total bilirubin levels and a baseline alkaline phosphatase level greater than five times the upper limit of normal.
Statistically, the patients were evenly distributed across the placebo arm and the two treatment arms, one of which dosed OCA at 10 mg/day; the other treatment arm had flexible dosing at 5-10 mg/day.
The POISE trial used a composite primary efficacy endpoint of achieving an alkaline phosphatase (ALP) less than 1.67 times the upper limit of normal, with total bilirubin within normal limits, and at least a 15% reduction in ALP.
“Significantly more OCA-treated patients with cirrhosis achieved the primary composite endpoint compared to placebo,” Dr. Vierling and his coauthors wrote in a poster presented at the annual meeting for the American Association for the Study of Liver Diseases. The difference was individually significant for all three values that made up the composite primary endpoint as well.
Secondary endpoints included gamma-glutamyltransferase, alanine aminotrasferase, and aspartate aminotransferase, all of which were significantly reduced among patients taking OCA. Patients on placebo saw these values rise over the time period of the study.
There were no new safety signals seen in the post hoc analysis of the group with cirrhosis that were not seen in the trial at large, said Dr. Vierling. Two individuals in the subgroup dropped out of the trial because of pruritis, a similar proportion to that seen in the full trial population.
The drug’s manufacturer, Intercept Pharmaceuticals, is working with the Food and Drug Administration to establish appropriate doses and intervals for obeticholic acid so it may be used safely in individuals with decompensated cirrhosis, said Dr. Vierling.
Obeticholic acid, a farnesoid-X receptor agonist, is an approved agent to use as add-on therapy to ursodeoxycholic acid (UDCA), or as monotherapy for patients who can’t tolerate UDCA.
Dr. Vierling disclosed financial relationships with Intercept Pharmaceuticals and with several other pharmaceutical companies. The study was funded by Intercept Pharmaceuticals.
koakes@frontlinemedcom.com
On Twitter @karioakes
BOSTON – Patients with primary biliary cholangitis (PBC) who have compensated cirrhosis fared just as well on obeticholic acid (OCA) as did PBC patients without cirrhosis, according to an analysis of data from POISE, the pivotal clinical trial for approval of OCA for PBC.
The POISE trial included 36 individuals with PBC and compensated cirrhosis, since cirrhosis “is an endpoint for virtually all liver diseases,” John Vierling, MD, said in a video interview at the meeting.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
To see how this group fared, Dr. Vierling and his coinvestigators performed a post hoc analysis of the POISE data to examine OCA’s safety and efficacy for patients with compensated cirrhosis. Patients with decompensated cirrhosis were not included in the trial.
Dr. Vierling, chief of hepatology at Baylor College of Medicine, Houston, noted that investigators worked hard to set the bar high for inclusion in the group with cirrhosis, to achieve very high specificity. “We did this by using very stringent criteria of liver biopsy, or transient elastography adjusted for a very high range of kilopascals required to diagnose cirrhosis in cholestatic patients,” he said. To be included, patients also had to have elevated total bilirubin levels and a baseline alkaline phosphatase level greater than five times the upper limit of normal.
Statistically, the patients were evenly distributed across the placebo arm and the two treatment arms, one of which dosed OCA at 10 mg/day; the other treatment arm had flexible dosing at 5-10 mg/day.
The POISE trial used a composite primary efficacy endpoint of achieving an alkaline phosphatase (ALP) less than 1.67 times the upper limit of normal, with total bilirubin within normal limits, and at least a 15% reduction in ALP.
“Significantly more OCA-treated patients with cirrhosis achieved the primary composite endpoint compared to placebo,” Dr. Vierling and his coauthors wrote in a poster presented at the annual meeting for the American Association for the Study of Liver Diseases. The difference was individually significant for all three values that made up the composite primary endpoint as well.
Secondary endpoints included gamma-glutamyltransferase, alanine aminotrasferase, and aspartate aminotransferase, all of which were significantly reduced among patients taking OCA. Patients on placebo saw these values rise over the time period of the study.
There were no new safety signals seen in the post hoc analysis of the group with cirrhosis that were not seen in the trial at large, said Dr. Vierling. Two individuals in the subgroup dropped out of the trial because of pruritis, a similar proportion to that seen in the full trial population.
The drug’s manufacturer, Intercept Pharmaceuticals, is working with the Food and Drug Administration to establish appropriate doses and intervals for obeticholic acid so it may be used safely in individuals with decompensated cirrhosis, said Dr. Vierling.
Obeticholic acid, a farnesoid-X receptor agonist, is an approved agent to use as add-on therapy to ursodeoxycholic acid (UDCA), or as monotherapy for patients who can’t tolerate UDCA.
Dr. Vierling disclosed financial relationships with Intercept Pharmaceuticals and with several other pharmaceutical companies. The study was funded by Intercept Pharmaceuticals.
koakes@frontlinemedcom.com
On Twitter @karioakes
EXPERT ANALYSIS FROM THE LIVER MEETING
SNP predicts liver cancer in hepatitis C patients regardless of SVR
BOSTON – rs4836493, a single nucleotide polymorphism of the gene encoding chondroitin sulfate synthase-3, significantly predicted hepatocellular carcinoma among patients with HCV even when they achieved sustained virologic response on pegylated interferon, according to a genome-wide association study.
The next step is to determine whether rs4836493 predicts liver cancer after SVR on the new direct-acting antiviral regimens, Basile Njei, MD, MPH, said during an oral presentation at the annual meeting of the American Association for the Study of Liver Diseases.
Cirrhotic patients face about a 2%-7% annual risk of hepatocellular carcinoma, noted Dr. Njei of Yale University, New Haven, Conn. “Recent studies show that people with HCV may still develop hepatocellular carcinoma even after achieving SVR,” he said.
To look for genetic predictors of this outcome, he and his associates genotyped 958 patients with HCV and advanced hepatic fibrosis from the Hepatitis C Antiviral Long-term Treatment against Cirrhosis (HALT-C) study. This trial had evaluated long-term, low-dose pegylated interferon therapy (90 mcg per week for 3.5 years) as a means of keeping fibrosis from progressing among HCV patients who had failed peginterferon and ribavirin therapy.
A total of 63% of patients had cirrhosis, and 55 (5.7%) developed biopsy or imaging-confirmed hepatocellular carcinoma over a median of 80 months of follow-up, Dr. Njei said. After the researchers controlled for age, sex, Ishak fibrosis score, and SVR status, rs4836493 predicted hepatocellular carcinoma with a highly significant P value of .000004.
This SNP is located on the CHSY3 gene, which plays a role in the chondroitin polymerization, tissue development, and morphogenesis, according to Dr. Njei. Notably, the gene has been implicated in the biology of colorectal tumors, he added.
Dr. Njei and his associates genotyped patients by using the 610-Quad platform, which contains more than 600,000 SNPs. They double-checked results and conducted more genetic analyses using PLINK 1.9, a free, open-source software program for genome-wide association data. Three-quarters of patients in the study were white, 72% were male, and median age at enrollment was 50 years, he noted.
Linking a single SNP to liver cancer despite SVR is a striking finding, but it is also preliminary, Dr. Njei cautioned. “The SNP identified in our discovery genome-wide association study needs future replication and validation in patients who achieve SVR after receiving the new direct-acting antiviral therapies,” he said.
The National Institutes of Health provided partial funding. Dr. Njei and his coinvestigators had no relevant financial conflicts of interest.
BOSTON – rs4836493, a single nucleotide polymorphism of the gene encoding chondroitin sulfate synthase-3, significantly predicted hepatocellular carcinoma among patients with HCV even when they achieved sustained virologic response on pegylated interferon, according to a genome-wide association study.
The next step is to determine whether rs4836493 predicts liver cancer after SVR on the new direct-acting antiviral regimens, Basile Njei, MD, MPH, said during an oral presentation at the annual meeting of the American Association for the Study of Liver Diseases.
Cirrhotic patients face about a 2%-7% annual risk of hepatocellular carcinoma, noted Dr. Njei of Yale University, New Haven, Conn. “Recent studies show that people with HCV may still develop hepatocellular carcinoma even after achieving SVR,” he said.
To look for genetic predictors of this outcome, he and his associates genotyped 958 patients with HCV and advanced hepatic fibrosis from the Hepatitis C Antiviral Long-term Treatment against Cirrhosis (HALT-C) study. This trial had evaluated long-term, low-dose pegylated interferon therapy (90 mcg per week for 3.5 years) as a means of keeping fibrosis from progressing among HCV patients who had failed peginterferon and ribavirin therapy.
A total of 63% of patients had cirrhosis, and 55 (5.7%) developed biopsy or imaging-confirmed hepatocellular carcinoma over a median of 80 months of follow-up, Dr. Njei said. After the researchers controlled for age, sex, Ishak fibrosis score, and SVR status, rs4836493 predicted hepatocellular carcinoma with a highly significant P value of .000004.
This SNP is located on the CHSY3 gene, which plays a role in the chondroitin polymerization, tissue development, and morphogenesis, according to Dr. Njei. Notably, the gene has been implicated in the biology of colorectal tumors, he added.
Dr. Njei and his associates genotyped patients by using the 610-Quad platform, which contains more than 600,000 SNPs. They double-checked results and conducted more genetic analyses using PLINK 1.9, a free, open-source software program for genome-wide association data. Three-quarters of patients in the study were white, 72% were male, and median age at enrollment was 50 years, he noted.
Linking a single SNP to liver cancer despite SVR is a striking finding, but it is also preliminary, Dr. Njei cautioned. “The SNP identified in our discovery genome-wide association study needs future replication and validation in patients who achieve SVR after receiving the new direct-acting antiviral therapies,” he said.
The National Institutes of Health provided partial funding. Dr. Njei and his coinvestigators had no relevant financial conflicts of interest.
BOSTON – rs4836493, a single nucleotide polymorphism of the gene encoding chondroitin sulfate synthase-3, significantly predicted hepatocellular carcinoma among patients with HCV even when they achieved sustained virologic response on pegylated interferon, according to a genome-wide association study.
The next step is to determine whether rs4836493 predicts liver cancer after SVR on the new direct-acting antiviral regimens, Basile Njei, MD, MPH, said during an oral presentation at the annual meeting of the American Association for the Study of Liver Diseases.
Cirrhotic patients face about a 2%-7% annual risk of hepatocellular carcinoma, noted Dr. Njei of Yale University, New Haven, Conn. “Recent studies show that people with HCV may still develop hepatocellular carcinoma even after achieving SVR,” he said.
To look for genetic predictors of this outcome, he and his associates genotyped 958 patients with HCV and advanced hepatic fibrosis from the Hepatitis C Antiviral Long-term Treatment against Cirrhosis (HALT-C) study. This trial had evaluated long-term, low-dose pegylated interferon therapy (90 mcg per week for 3.5 years) as a means of keeping fibrosis from progressing among HCV patients who had failed peginterferon and ribavirin therapy.
A total of 63% of patients had cirrhosis, and 55 (5.7%) developed biopsy or imaging-confirmed hepatocellular carcinoma over a median of 80 months of follow-up, Dr. Njei said. After the researchers controlled for age, sex, Ishak fibrosis score, and SVR status, rs4836493 predicted hepatocellular carcinoma with a highly significant P value of .000004.
This SNP is located on the CHSY3 gene, which plays a role in the chondroitin polymerization, tissue development, and morphogenesis, according to Dr. Njei. Notably, the gene has been implicated in the biology of colorectal tumors, he added.
Dr. Njei and his associates genotyped patients by using the 610-Quad platform, which contains more than 600,000 SNPs. They double-checked results and conducted more genetic analyses using PLINK 1.9, a free, open-source software program for genome-wide association data. Three-quarters of patients in the study were white, 72% were male, and median age at enrollment was 50 years, he noted.
Linking a single SNP to liver cancer despite SVR is a striking finding, but it is also preliminary, Dr. Njei cautioned. “The SNP identified in our discovery genome-wide association study needs future replication and validation in patients who achieve SVR after receiving the new direct-acting antiviral therapies,” he said.
The National Institutes of Health provided partial funding. Dr. Njei and his coinvestigators had no relevant financial conflicts of interest.
AT THE LIVER MEETING 2016
Key clinical point: A single nucleotide polymorphism of the CHSY3 gene predicted liver cancer in patients who successfully completed treatment for chronic hepatitis C virus infection.
Major finding: After researchers controlled for sustained virologic response and other confounders, the rs4836493 variant predicted hepatocellular carcinoma with a P value of .000004.
Data source: A genome-wide association study of 958 HCV patients with advanced hepatic fibrosis from the HALT-C trial.
Disclosures: The National Institutes of Health provided partial funding. Dr. Njei and his coinvestigators had no relevant financial conflicts of interest.
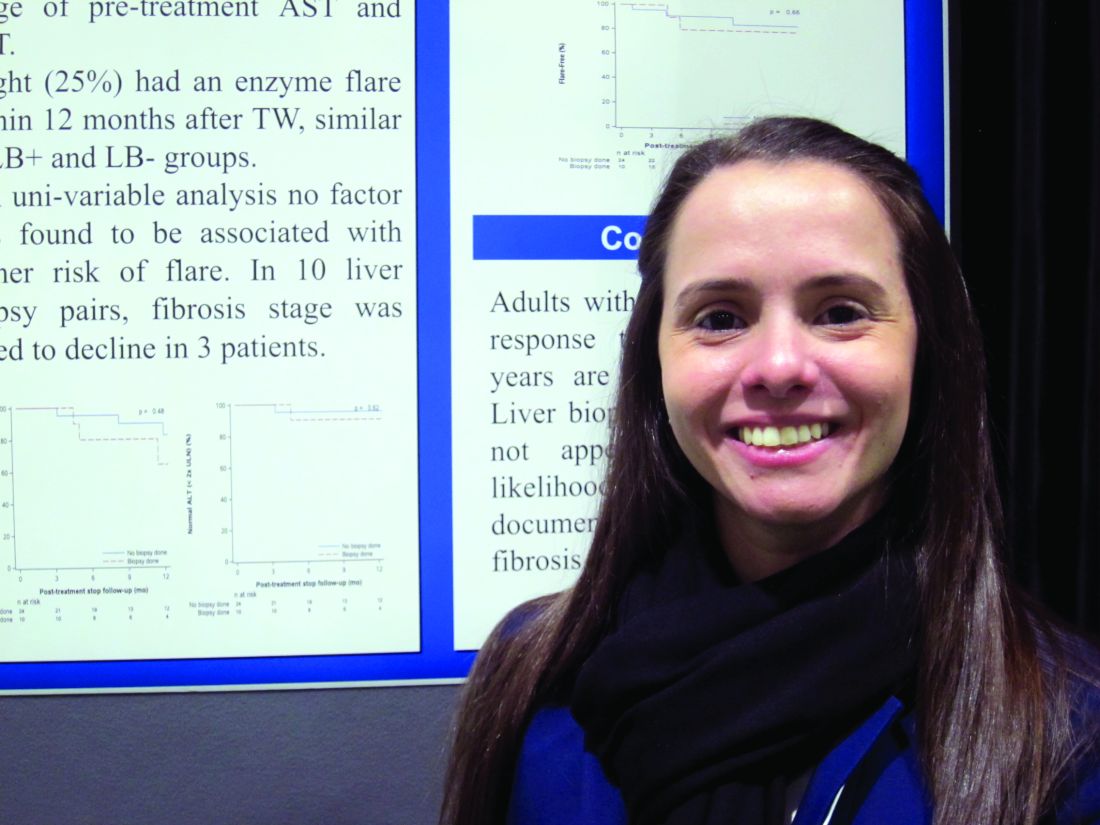
Treatment withdrawal without prior liver biopsy found safe in well-controlled autoimmune hepatitis
BOSTON – Although current guidance calls for a liver biopsy prior to treatment withdrawal in autoimmune hepatitis (AIH), a retrospective observational analysis conducted by researchers from the Cleveland Clinic offers a different view.
“Maybe not everyone needs a liver biopsy before withdrawing treatment,” Yilien Alonso, MD, an internist at the Cleveland Clinic in Weston, Fla., said in an interview at the annual meeting of the American Association for the Study of Liver Diseases.
Both the European Association for Study of the Liver and the AASLD recommend liver biopsy prior to treatment withdrawal in AIH, but the expensive procedure is not without risk of morbidity and mortality. Dr. Alonso and her coinvestigators reviewed the records of 508 AIH patients seen at their institution between January 2001 and April 2015. After excluding the records of patients who’d had juvenile onset of AIH, or who were treated with agents other than corticosteroids and azathioprine, the researchers found 34 adults with similar pretreatment profiles who’d had treatment withdrawal after 2 years of excellent response to treatment, 10 of whom had a liver biopsy prior to treatment withdrawal.
The outcomes at 1 year post treatment withdrawal for all 34 were similar, with no difference in flare rates or reinitiation of treatment. In those who’d had the second liver biopsy, the fibrosis stage was noted at 1 year to have declined in three patients.
“If you have a stable patient population that you are tracking every 3-6 months, we don’t see why you can’t stop the treatment without having to have another invasive procedure,” Dr. Alonso said.
BOSTON – Although current guidance calls for a liver biopsy prior to treatment withdrawal in autoimmune hepatitis (AIH), a retrospective observational analysis conducted by researchers from the Cleveland Clinic offers a different view.
“Maybe not everyone needs a liver biopsy before withdrawing treatment,” Yilien Alonso, MD, an internist at the Cleveland Clinic in Weston, Fla., said in an interview at the annual meeting of the American Association for the Study of Liver Diseases.
Both the European Association for Study of the Liver and the AASLD recommend liver biopsy prior to treatment withdrawal in AIH, but the expensive procedure is not without risk of morbidity and mortality. Dr. Alonso and her coinvestigators reviewed the records of 508 AIH patients seen at their institution between January 2001 and April 2015. After excluding the records of patients who’d had juvenile onset of AIH, or who were treated with agents other than corticosteroids and azathioprine, the researchers found 34 adults with similar pretreatment profiles who’d had treatment withdrawal after 2 years of excellent response to treatment, 10 of whom had a liver biopsy prior to treatment withdrawal.
The outcomes at 1 year post treatment withdrawal for all 34 were similar, with no difference in flare rates or reinitiation of treatment. In those who’d had the second liver biopsy, the fibrosis stage was noted at 1 year to have declined in three patients.
“If you have a stable patient population that you are tracking every 3-6 months, we don’t see why you can’t stop the treatment without having to have another invasive procedure,” Dr. Alonso said.
BOSTON – Although current guidance calls for a liver biopsy prior to treatment withdrawal in autoimmune hepatitis (AIH), a retrospective observational analysis conducted by researchers from the Cleveland Clinic offers a different view.
“Maybe not everyone needs a liver biopsy before withdrawing treatment,” Yilien Alonso, MD, an internist at the Cleveland Clinic in Weston, Fla., said in an interview at the annual meeting of the American Association for the Study of Liver Diseases.
Both the European Association for Study of the Liver and the AASLD recommend liver biopsy prior to treatment withdrawal in AIH, but the expensive procedure is not without risk of morbidity and mortality. Dr. Alonso and her coinvestigators reviewed the records of 508 AIH patients seen at their institution between January 2001 and April 2015. After excluding the records of patients who’d had juvenile onset of AIH, or who were treated with agents other than corticosteroids and azathioprine, the researchers found 34 adults with similar pretreatment profiles who’d had treatment withdrawal after 2 years of excellent response to treatment, 10 of whom had a liver biopsy prior to treatment withdrawal.
The outcomes at 1 year post treatment withdrawal for all 34 were similar, with no difference in flare rates or reinitiation of treatment. In those who’d had the second liver biopsy, the fibrosis stage was noted at 1 year to have declined in three patients.
“If you have a stable patient population that you are tracking every 3-6 months, we don’t see why you can’t stop the treatment without having to have another invasive procedure,” Dr. Alonso said.
AT THE LIVER MEETING 2016
Key clinical point:
Major finding: Flare rates were similar post treatment withdrawal at 1 year in autoimmune hepatitis patients with and without a prior liver biopsy.
Data source: Retrospective observational analysis of 34 adults with well-controlled autoimmune hepatitis given treatment withdrawal with and without liver biopsy in large academic practice.
Disclosures: Dr. Alonso did not have any relevant disclosures.
VIDEO: Don’t be surprised by weight gain in men after HCV cure
BOSTON – In the new era of direct-acting antiviral (DAA) therapy, physicians will be seeing more and more patients who have achieved a cure of their hepatitis C virus (HCV). Once freed from the burden of a chronic illness, patients feel better and may eat better. Unexpected weight gain and potential associated health effects may be the next set of challenges patients and their physicians will face.
A single-center retrospective study of patients who had achieved sustained virologic response (SVR) after treatment for HCV found a small but significant weight gain in men, but not women. Additionally, according to noninvasive assessments, liver fat increased significantly in men, but not women, after SVR was achieved.
In a study of 63 patients (42 male, 67%) who received DAA treatment for HCV, mean weight gain for men after SVR was 2.8 pounds (range, –26 to +17; P = .0459), and body mass index (BMI) increased by a mean 0.50 kg/m2 (range, –3.6 to +3.33; P = .0176). No significant change was seen for women when pre- and posttreatment measures were compared.
Isaac Wasserman, a medical student at Mount Sinai Medical Center, New York, presented the results of the single-center retrospective study in a poster presentation at the annual meeting of the American Association for the Study of Liver Diseases.
To assess changes in liver fat, Mr. Wasserman and his coinvestigator used results of pre- and posttreatment transient elastography with controlled attenuation parameter (CAP). CAP measures the degree to which the ultrasound signal is attenuated by liver fat, he explained in a video interview.
For men, hepatic steatosis increased by this measure, with CAP measurements up by a mean 18 dB/m (range, –106 to +128, P = .0314). Mr. Wasserman and his colleagues wrote, “The change in liver fat was large enough to push 11% of the cohort (n = 7 of 63) into advanced steatosis (CAP greater than 300 dB/m).” Again, the women studied had no significant posttreatment change in liver fat.
Post-SVR weight gain appeared to be the culprit in the increased fat seen in the posttreatment livers. Mr. Wasserman and his colleagues in the abstract accompanying the presentation, “Changes in weight were positively correlated with changes in liver fat (P = .006).”
Mr. Wasserman said that he and his coinvestigators believe that social, and not biochemical or mechanistic, reasons underlie the weight gain and increased hepatic steatosis. They are planning further investigation of social and economic factors that may underlie the difference seen in this study, and hope to continue and expand data acquisition to validate their findings.
Mr. Wasserman reported no conflicts of interest or outside sources of funding for the study.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @karioakes
BOSTON – In the new era of direct-acting antiviral (DAA) therapy, physicians will be seeing more and more patients who have achieved a cure of their hepatitis C virus (HCV). Once freed from the burden of a chronic illness, patients feel better and may eat better. Unexpected weight gain and potential associated health effects may be the next set of challenges patients and their physicians will face.
A single-center retrospective study of patients who had achieved sustained virologic response (SVR) after treatment for HCV found a small but significant weight gain in men, but not women. Additionally, according to noninvasive assessments, liver fat increased significantly in men, but not women, after SVR was achieved.
In a study of 63 patients (42 male, 67%) who received DAA treatment for HCV, mean weight gain for men after SVR was 2.8 pounds (range, –26 to +17; P = .0459), and body mass index (BMI) increased by a mean 0.50 kg/m2 (range, –3.6 to +3.33; P = .0176). No significant change was seen for women when pre- and posttreatment measures were compared.
Isaac Wasserman, a medical student at Mount Sinai Medical Center, New York, presented the results of the single-center retrospective study in a poster presentation at the annual meeting of the American Association for the Study of Liver Diseases.
To assess changes in liver fat, Mr. Wasserman and his coinvestigator used results of pre- and posttreatment transient elastography with controlled attenuation parameter (CAP). CAP measures the degree to which the ultrasound signal is attenuated by liver fat, he explained in a video interview.
For men, hepatic steatosis increased by this measure, with CAP measurements up by a mean 18 dB/m (range, –106 to +128, P = .0314). Mr. Wasserman and his colleagues wrote, “The change in liver fat was large enough to push 11% of the cohort (n = 7 of 63) into advanced steatosis (CAP greater than 300 dB/m).” Again, the women studied had no significant posttreatment change in liver fat.
Post-SVR weight gain appeared to be the culprit in the increased fat seen in the posttreatment livers. Mr. Wasserman and his colleagues in the abstract accompanying the presentation, “Changes in weight were positively correlated with changes in liver fat (P = .006).”
Mr. Wasserman said that he and his coinvestigators believe that social, and not biochemical or mechanistic, reasons underlie the weight gain and increased hepatic steatosis. They are planning further investigation of social and economic factors that may underlie the difference seen in this study, and hope to continue and expand data acquisition to validate their findings.
Mr. Wasserman reported no conflicts of interest or outside sources of funding for the study.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @karioakes
BOSTON – In the new era of direct-acting antiviral (DAA) therapy, physicians will be seeing more and more patients who have achieved a cure of their hepatitis C virus (HCV). Once freed from the burden of a chronic illness, patients feel better and may eat better. Unexpected weight gain and potential associated health effects may be the next set of challenges patients and their physicians will face.
A single-center retrospective study of patients who had achieved sustained virologic response (SVR) after treatment for HCV found a small but significant weight gain in men, but not women. Additionally, according to noninvasive assessments, liver fat increased significantly in men, but not women, after SVR was achieved.
In a study of 63 patients (42 male, 67%) who received DAA treatment for HCV, mean weight gain for men after SVR was 2.8 pounds (range, –26 to +17; P = .0459), and body mass index (BMI) increased by a mean 0.50 kg/m2 (range, –3.6 to +3.33; P = .0176). No significant change was seen for women when pre- and posttreatment measures were compared.
Isaac Wasserman, a medical student at Mount Sinai Medical Center, New York, presented the results of the single-center retrospective study in a poster presentation at the annual meeting of the American Association for the Study of Liver Diseases.
To assess changes in liver fat, Mr. Wasserman and his coinvestigator used results of pre- and posttreatment transient elastography with controlled attenuation parameter (CAP). CAP measures the degree to which the ultrasound signal is attenuated by liver fat, he explained in a video interview.
For men, hepatic steatosis increased by this measure, with CAP measurements up by a mean 18 dB/m (range, –106 to +128, P = .0314). Mr. Wasserman and his colleagues wrote, “The change in liver fat was large enough to push 11% of the cohort (n = 7 of 63) into advanced steatosis (CAP greater than 300 dB/m).” Again, the women studied had no significant posttreatment change in liver fat.
Post-SVR weight gain appeared to be the culprit in the increased fat seen in the posttreatment livers. Mr. Wasserman and his colleagues in the abstract accompanying the presentation, “Changes in weight were positively correlated with changes in liver fat (P = .006).”
Mr. Wasserman said that he and his coinvestigators believe that social, and not biochemical or mechanistic, reasons underlie the weight gain and increased hepatic steatosis. They are planning further investigation of social and economic factors that may underlie the difference seen in this study, and hope to continue and expand data acquisition to validate their findings.
Mr. Wasserman reported no conflicts of interest or outside sources of funding for the study.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @karioakes
AT THE LIVER MEETING
Lack of health literacy and normal routine implicated in hepatitis B virus treatment nonadherence
BOSTON – Lack of health literacy, lack of routine, and being a nonnative speaker of English were predictors of treatment nonadherence in one-quarter of adults with hepatitis B virus in Australia, according to a study.
“Clinicians don’t know this is happening. We overlook it. Because it’s just one tablet a day, we think it’s quite easy, but when I took up this project, I completely underestimated the complexity of adherence and how many different factors can play into why a patient does or doesn’t adhere,” Suzanne Sheppard-Law, RN, MPH, PhD, a senior research fellow at the University of Technology Sydney, said in an interview about her prize-winning poster presentation at this year’s annual meeting of the American Association for the Study of Liver Diseases.
The findings grew from Dr. Sheppard-Law’s clinical practice where she noticed a trend in some patients whose treatment regimen would lose efficacy over time. When switched to other therapies, the pattern would be repeated. Dr. Sheppard-Law interviewed 29 of these patients in person to see if there were commonalities she could address.
“The deeper I dug, the more it all unfolded before me,” she said. It turned out that patients who’d been endorsing adherence were not. In some cases, patients were skipping their medications for days at a time.
This informal study lead to a more formal one focused on a patient’s level of health literacy. Dr. Sheppard-Law and her colleagues examined factors the World Health Organization says are implicated in adherence, including ones that are social and economic, and others that are related to clinical worker interactions, health systems, individual therapy and condition, and patient considerations. They conducted in-person interviews and worked with the patients as they completed the Newest Vital Sign health literacy survey online.
Just over a fifth of respondents said they followed a regular routine when taking their medication, such as taking it at a certain time every day; however, three-quarters of those surveyed said they didn’t think having a routine made any difference (P less than .001). Half of respondents were prescribed at least one additional daily medication to their antiretroviral pill. A third had no idea what type of medication was prescribed for their hepatitis B.
Whether the person was proficient in English, and the impact this had on perceived communication between the patient and clinician was another factor, as most of the patients in the study were immigrants to Australia who’d been living there, on average, about 19 years. Only 27% of the study group reported that they spoke English at home as their primary language.
“It has to be individually focused, person-centered care, is the conclusion I came to,” Dr. Sheppard-Law said. Although her findings do not indicate a need for more resources in the clinic, she did say that clinicians could help patients by asking them to repeat back to them what they have heard.
“I don’t believe it has to be more resource intense; you just need to be sure the patient understands at the beginning what they need to do. Then you have a better chance [they will adhere],” she said. Because patients with poor health literacy are unlikely to tell their clinician that they do not fully grasp what they are being told about their condition and their treatment, Dr. Sheppard-Law suggested asking patients at the end of their consultation to detail what their routine will be, what they will do if they lose their prescription, what they will do if they run out of medication, and asking if they understand that their medication must be taken daily. “They need to understand it’s not okay to skip a day,” she said. “It’s our responsibility to ensure they know that.”
wmcknight@frontlinemedcom.com
On Twitter @whitneymcknight
BOSTON – Lack of health literacy, lack of routine, and being a nonnative speaker of English were predictors of treatment nonadherence in one-quarter of adults with hepatitis B virus in Australia, according to a study.
“Clinicians don’t know this is happening. We overlook it. Because it’s just one tablet a day, we think it’s quite easy, but when I took up this project, I completely underestimated the complexity of adherence and how many different factors can play into why a patient does or doesn’t adhere,” Suzanne Sheppard-Law, RN, MPH, PhD, a senior research fellow at the University of Technology Sydney, said in an interview about her prize-winning poster presentation at this year’s annual meeting of the American Association for the Study of Liver Diseases.
The findings grew from Dr. Sheppard-Law’s clinical practice where she noticed a trend in some patients whose treatment regimen would lose efficacy over time. When switched to other therapies, the pattern would be repeated. Dr. Sheppard-Law interviewed 29 of these patients in person to see if there were commonalities she could address.
“The deeper I dug, the more it all unfolded before me,” she said. It turned out that patients who’d been endorsing adherence were not. In some cases, patients were skipping their medications for days at a time.
This informal study lead to a more formal one focused on a patient’s level of health literacy. Dr. Sheppard-Law and her colleagues examined factors the World Health Organization says are implicated in adherence, including ones that are social and economic, and others that are related to clinical worker interactions, health systems, individual therapy and condition, and patient considerations. They conducted in-person interviews and worked with the patients as they completed the Newest Vital Sign health literacy survey online.
Just over a fifth of respondents said they followed a regular routine when taking their medication, such as taking it at a certain time every day; however, three-quarters of those surveyed said they didn’t think having a routine made any difference (P less than .001). Half of respondents were prescribed at least one additional daily medication to their antiretroviral pill. A third had no idea what type of medication was prescribed for their hepatitis B.
Whether the person was proficient in English, and the impact this had on perceived communication between the patient and clinician was another factor, as most of the patients in the study were immigrants to Australia who’d been living there, on average, about 19 years. Only 27% of the study group reported that they spoke English at home as their primary language.
“It has to be individually focused, person-centered care, is the conclusion I came to,” Dr. Sheppard-Law said. Although her findings do not indicate a need for more resources in the clinic, she did say that clinicians could help patients by asking them to repeat back to them what they have heard.
“I don’t believe it has to be more resource intense; you just need to be sure the patient understands at the beginning what they need to do. Then you have a better chance [they will adhere],” she said. Because patients with poor health literacy are unlikely to tell their clinician that they do not fully grasp what they are being told about their condition and their treatment, Dr. Sheppard-Law suggested asking patients at the end of their consultation to detail what their routine will be, what they will do if they lose their prescription, what they will do if they run out of medication, and asking if they understand that their medication must be taken daily. “They need to understand it’s not okay to skip a day,” she said. “It’s our responsibility to ensure they know that.”
wmcknight@frontlinemedcom.com
On Twitter @whitneymcknight
BOSTON – Lack of health literacy, lack of routine, and being a nonnative speaker of English were predictors of treatment nonadherence in one-quarter of adults with hepatitis B virus in Australia, according to a study.
“Clinicians don’t know this is happening. We overlook it. Because it’s just one tablet a day, we think it’s quite easy, but when I took up this project, I completely underestimated the complexity of adherence and how many different factors can play into why a patient does or doesn’t adhere,” Suzanne Sheppard-Law, RN, MPH, PhD, a senior research fellow at the University of Technology Sydney, said in an interview about her prize-winning poster presentation at this year’s annual meeting of the American Association for the Study of Liver Diseases.
The findings grew from Dr. Sheppard-Law’s clinical practice where she noticed a trend in some patients whose treatment regimen would lose efficacy over time. When switched to other therapies, the pattern would be repeated. Dr. Sheppard-Law interviewed 29 of these patients in person to see if there were commonalities she could address.
“The deeper I dug, the more it all unfolded before me,” she said. It turned out that patients who’d been endorsing adherence were not. In some cases, patients were skipping their medications for days at a time.
This informal study lead to a more formal one focused on a patient’s level of health literacy. Dr. Sheppard-Law and her colleagues examined factors the World Health Organization says are implicated in adherence, including ones that are social and economic, and others that are related to clinical worker interactions, health systems, individual therapy and condition, and patient considerations. They conducted in-person interviews and worked with the patients as they completed the Newest Vital Sign health literacy survey online.
Just over a fifth of respondents said they followed a regular routine when taking their medication, such as taking it at a certain time every day; however, three-quarters of those surveyed said they didn’t think having a routine made any difference (P less than .001). Half of respondents were prescribed at least one additional daily medication to their antiretroviral pill. A third had no idea what type of medication was prescribed for their hepatitis B.
Whether the person was proficient in English, and the impact this had on perceived communication between the patient and clinician was another factor, as most of the patients in the study were immigrants to Australia who’d been living there, on average, about 19 years. Only 27% of the study group reported that they spoke English at home as their primary language.
“It has to be individually focused, person-centered care, is the conclusion I came to,” Dr. Sheppard-Law said. Although her findings do not indicate a need for more resources in the clinic, she did say that clinicians could help patients by asking them to repeat back to them what they have heard.
“I don’t believe it has to be more resource intense; you just need to be sure the patient understands at the beginning what they need to do. Then you have a better chance [they will adhere],” she said. Because patients with poor health literacy are unlikely to tell their clinician that they do not fully grasp what they are being told about their condition and their treatment, Dr. Sheppard-Law suggested asking patients at the end of their consultation to detail what their routine will be, what they will do if they lose their prescription, what they will do if they run out of medication, and asking if they understand that their medication must be taken daily. “They need to understand it’s not okay to skip a day,” she said. “It’s our responsibility to ensure they know that.”
wmcknight@frontlinemedcom.com
On Twitter @whitneymcknight
AT THE LIVER MEETING 2016
Key clinical point:
Major finding: A quarter of adults with hepatitis B virus were treatment noncompliant in the past 30 days.
Data source: In-person and online survey of 277 adults with hepatitis B virus.
Disclosures: Dr. Sheppard-Law did not have any relevant disclosures.