News
FDA approves test to screen donated blood for Zika virus
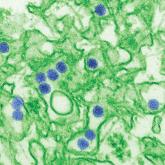
The cobas Zika test is the first test approved for screening the blood supply.

AT AN FDA ADVISORY COMMITTEE MEETING
SILVER SPRING, MD – Universal testing of individual blood donations for the presence of Zika virus was unanimously rejected by voting members of the Food and Drug Administration’s Blood Products Advisory Committee at a December 1 meeting.
Universal individual donor testing, while comprehensive, is resource intensive and places a burden on the blood system that is not outweighed by the benefits, 10 of the 11 committee members concluded. The other committee member could not be reached by phone for this vote.
The committee instead recommended by a vote of 10 to 1 that mini-pool nucleic acid testing (MP-NAT) be performed in all states and territories with known cases of Zika virus infection and the presence of A. aegypti mosquitoes, as well as in states and territories with a high number of travelers from areas with Zika virus infections. Also, the committee members agreed that a trigger needs to be defined for when to undertake universal individual donor nucleic acid testing (ID-NAT) in those areas.
Additionally, the committee agreed that it was not necessary to maintain a Zika virus-negative blood inventory for at-risk patients, such as pregnant women and newborns. Zika virus, a vector-borne disease carried by the Aedes aegypti and Aedes albopictus mosquitoes, has also been transmitted via sexual contact and blood transfusion. Infection has been linked to fetal loss and microcephaly in the offspring of infected pregnant women. Other neurological disorders, including Guillain-Barré Syndrome, also have been linked to Zika virus infection.
Noting the complexity of managing an inventory of tested and non-tested blood, the committee rejected the separate inventory approach by a vote of 9 to 2.*
The panel was clearly divided on the possibility of eliminating all Zika virus testing in some states and territories; 5 members supported this measure, 4 opposed it, and 2 abstained from voting.
The panel unanimously rejected using screening questionnaires to determine whether to selectively test individual at-risk donors in areas with active vector-borne Zika virus infections. This option was considered particularly troublesome, they agreed, because it relies on the use of nonspecific, insensitive, and error-prone questionnaires.
Some level of Zika virus testing is needed to safeguard blood products, the committee said. Eliminating all Zika virus testing of blood products would open the door for infections via transfusion and would diminish preparedness against a potential epidemic, they unanimously determined.
Prior to voting, the committee listened to presentations on the epidemiology of Zika virus infections, the effectiveness of screening tests, and the risk for transmission via transfusion.
Carolyn Gould, MD, of the Centers for Disease Control and Prevention, Atlanta, reported that the number of laboratory-confirmed Zika virus infections in 2016 was 4,830 for travelers to endemic areas and 224 for locally-acquired cases. In 2017, those numbers dropped to 344 confirmed cases for travelers and 2 for locally-acquired cases.
More than 4 million blood donations in the United States and Puerto Rico have been screened for Zika virus RNA using the cobas assay, which is now FDA approved. The overall confirmed positive rate of Zika virus is 0.0007% in donations from the continental United States (29 positive results in 4,341,770 donations) and 0.326% in donations from Puerto Rico (356 out of 111,808 donations) based on data obtained from May 23, 2016 to October 7, 2017, according to Tony Hardiman, Blood Screening, Life Cycle Leader at Roche Molecular Systems.
Of the Zika virus-positive donors who were available for follow up, 23 of 27 had traveled to Zika-active areas, including 3 cases associated with domestic travel to Florida. “I was surprised that 4 of the 29 were from Cuba, but it does seem, as we just saw, (that) an increasing number are coming out from Cuba, from travel to Cuba,” Mr. Hardiman said during his presentation to the committee.
Findings concerning viral RNA duration in blood and other body fluids were presented by Michael Busch, MD of the University of California, San Francisco, who spoke during the public hearing portion of the meeting.**
According to Dr. Busch, blood is likely not infectious to others once donors develop Zika virus-neutralizing antibodies and their viral load levels become very low.
Based on his review of various studies, Dr. Busch concluded that mini-pool testing options with triggers for individual testing are appropriate and effective for detecting Zika virus in endemic areas.
“In Puerto Rico, within a day of picking up a mini-pool positive [result}, we would have ID-NAT in place,” Dr. Busch said. “The mini-pool testing is picking up 90% of those at highest risk.”
The committee recommendations serve as guidance to the FDA, which is not obligated to follow the committee’s recommendations.
*Correction 12/14/17: An earlier version of this story misstated the vote on maintaining a Zika virus-negative blood inventory for at-risk patients. The advisory committee voted against that approach.
**Correction 12/14/17: Dr. Michael Busch's name was misstated in an earlier version of this article.
The cobas Zika test is the first test approved for screening the blood supply.
