PARIS – A fast and simple clinically based scoring system enables physicians to determine the chance of a successful outcome for octogenarians undergoing percutaneous coronary intervention, James Cockburn, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
All six elements of the scoring system are readily available either at the time the very elderly patient presents or at diagnostic angiography, noted Dr. Cockburn of Brighton and Sussex University Hospital in Brighton, England.
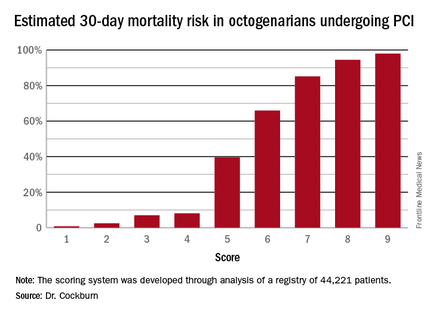
He and his coworkers developed the risk score through analysis of a registry of 44,221 patients aged 80 or older who underwent percutaneous coronary intervention (PCI). The procedural success rate – defined as less than a 30% residual stenosis and TIMI (Thrombolysis in Myocardial Infarction) 3 antegrade blood flow – was 92.3%. The 30-day mortality rate was 3.9%. The investigators teased out a set of easily accessible clinical factors associated with 30-day mortality and came up with a novel risk scoring system using a 9-point scale.
The clinical factors and scoring system are as follows:
• Age. 1 point for being 80-89, and 2 points at age 90 or older.
• Indication for PCI. 1 point for unstable angina/non–ST segment elevation MI, 2 points for STEMI, 0 points for other indications.
• Ventilated preprocedure. 1 point if yes.
• Creatinine level above 200 umol/L. 1 point for yes.
• Preprocedural cardiogenic shock. 2 points for yes.
• Poor left ventricular ejection fraction. If less than 30%, 1 point.
Thus, scores can range from 1 to 9. Dr. Cockburn and his coworkers calculated the risk of 30-day mortality for each possible score. They validated the score by performing a receiver operator curve analysis that showed an area under the curve of 0.83, suggestive of relatively high sensitivity and specificity.
A score of 4 or less suggests a very good chance of survival at 30 days. In contrast, a score of 6 was associated with a two in three chance of death by 30 days. And it’s not hard to reach a 6: A patient who is 90 years old (2 points), presents with STEMI (2 points), and is in cardiogenic shock (2 points) is already there. But if a 90-year-old patient presents with unstable angina and none of the other risk factors, that’s a score of 3 points, with an estimated probability of death at 30 days of only 7%, he noted.
Dr. Cockburn stressed that this risk score should not be used to base decisions on whether to take very elderly patients to the cardiac catheterization laboratory. “It enables you to have a useful conversation with relatives in which you can explain that this is a very high-risk intervention, or perhaps a low-risk intervention,” according to the cardiologist.
Discussants were emphatic in their agreement with Dr. Cockburn that this risk score shouldn’t be utilized to decide who does or doesn’t get PCI. One panelist said that what’s really lacking now in clinical practice – and where that huge British registry database could be helpful – is a scoring system that would predict which patients who don’t present in cardiogenic shock are going to develop it post PCI.
Dr. Cockburn reported having no relevant financial conflicts.