PALM BEACH, Fla. - Neuropathic diabetic foot ulcers can be treated with revascularization, but successful surgery doesn't always translate into good long-term outcomes, a study has shown.
In the review of 917 such ulcers, the 219 revascularized lesions had no better healing or survival outcomes than that of ischemic wounds that were not revascularized, Dr. Spence Taylor said at the annual meeting of the Southern Surgical Association. Just 35% of the revascularized ulcers healed completely, and 32% of the patients eventually needed an amputation.
"Assessing this treatment, we must conclude that while revascularization is important to wound healing, favorable functional outcomes can't be assumed," said Dr. Taylor of the Greenville (S.C.) Hospital System. "This suggests that we should realign our financial incentives [away from procedures and] toward foot care and wound prevention, affording a better opportunity of prevention and preservation of functional outcomes."
Dr. Taylor and his colleagues presented a review of 917 limbs with new diabetic foot ulcers that occurred among 706 patients. Most of the patients (87%) had type 2 diabetes, and more than half (52%) were smokers. Other comorbidities included hyperlipidemia (53%), hypertension (90%), and end-stage renal disease (26%).
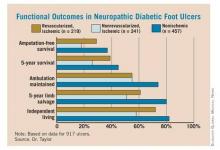
Of the 917 ulcers, 457 were nonischemic and 460 were ischemic. Of the ischemic lesions, 241 were not revascularized and 219 were – 137 by angioplasty and 82 by open surgery. Outcomes measured included primary healing, functional healing (defined as healing to clinical insignificance), limb salvage, amputation-free survival, 5-year survival, and maintenance of ambulation and independent living.
Overall, the data showed primary wound healing in 27%, functional healing in 53%, minor amputations in 28%, and major amputations in 20% of patients. The time to achieve healing was 7-8 months.
For patients with the revascularized ulcers, the 5-year survival rate was 39%, and 5-year limb salvage rate was 61%. The 5-year rate of amputation-free survival was 29%, while 55% of patients maintained ambulation and 72% maintained independent living at 5 years.
When the investigators compared the different groups (nonischemic, revascularized ischemic, and nonrevascularized ischemic), they found no significant differences in the rate of wound healing. But ischemia was a significant predictor of poor functional outcomes, which revascularization did not completely mitigate. "Ischemic patients had twice as many amputations and 50% higher mortality than nonischemic patients, whether they were revascularized or not. It was quite remarkable morbidity," Dr. Taylor said.
The presence of ischemia conferred a 26% increase in the risk of death by 5 years. Also, patients with end-stage renal disease were 2.5 times more likely to die than were those without. However, functional healing was associated with a 42% decreased risk of death.
Those same factors were independent predictors of amputation-free survival. Ischemia conferred a 57% increased risk of losing a limb, while end-stage renal disease doubled that risk. Functional healing, however, decreased the risk of amputation by 58%.
"Patients who were able to heal their wound significantly outperformed those who did not – not only for limb salvage and survival, which is intuitive, but also for amputation-free survival and maintenance of ambulation and independent living status, which is not intuitive," Dr. Taylor said. "The poorest outcomes were in ischemic nonrevascularized patients, whose 5-year mortality was 75% and amputation-free survival only 18% – as bad as any cancer outcomes presented at this meeting."
Conventional wisdom holds that patients who do have revascularization will almost always heal their ulcers. Therefore, Dr. Taylor said, reimbursement has been structured to favor surgical intervention rather than diabetic foot care and prevention.
"Reimbursement is very robust for procedures, while for wound care, it barely covers the cost, implying that revascularization does all the heavy lifting."
His review shows that this is not always the case. "Our functional outcomes were disappointing at best and really reflect an opportunity for improvement. Realigning the financial incentives toward foot wound care and prevention may give us a better opportunity to make these improvements."
Dr. Taylor had no financial disclosures.