TUCSON – A bold effort to jump-start research on the prevention of Alzheimer’s disease is getting underway, energized by promising means for identifying people at risk for the disease and by preventive measures that could potentially slow disease progression.
The Alzheimer’s Prevention Initiative, the brainchild of Dr. Eric M. Reiman and his colleagues at the Banner Alzheimer’s Institute in Phoenix, has obtained funding from the National Institute on Aging and other government agencies, the pharmaceutical industry, and philanthropic organizations.
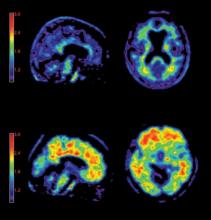
Numerous promising investigational disease-modifying and risk-reduction interventions are ready for clinical testing. Genetic studies are providing new treatment targets. And work on brain imaging techniques and biomarkers such as the cerebrospinal fluid tau protein/beta-amyloid 1:42 ratio has progressed to the point they can be used to measure the success of interventions in presymptomatic individuals without waiting for onset of full-blown Alzheimer’s disease, Dr. Reiman explained at the psychopharmacology review, sponsored by the University of Arizona.
At the same time, the Food and Drug Administration is being more open minded than in the past about what it’ll take to get a new Alzheimer’s drug approved. Imaging and biomarker findings are now likely to be deemed acceptable evidence for approving an indication of "slows disease progression."
In anticipation of a coming new era of Alzheimer’s dementia research, the National Institutes of Health and the Alzheimer’s Association in coming months will release proposed new diagnostic criteria for dementia from Alzheimer’s disease, the first in 26 years. They will also propose new diagnostic criteria for mild cognitive impairment from Alzheimer’s disease, and research criteria – not for use in clinical practice – for preclinical Alzheimer’s disease based upon biomarker changes prior to symptom onset, according to Dr. Reiman, who is executive director of the Banner Alzheimer’s Institute as well as professor of psychiatry at the University of Arizona, Tucson.
He predicted that within the next several months, the FDA will approve florbetapir-PET as the first brain amyloid imaging technique, with marketing approval of several other amyloid imaging techniques to follow over the next several years.
The approved indication will be to rule out Alzheimer’s dementia – not to rule it in – since amyloid plaque is present in 30% of cognitively normal individuals. This is not an imaging technique intended for healthy people to predict their risk; rather, its greatest utility will be in situations when physicians are least certain about the diagnosis of Alzheimer’s disease, as in patients who may be in the earliest clinical stages or who have atypical features, explained Dr. Reiman, who has been involved in pivotal clinical trials of florbetapir PET.
Enrollment is underway for the first two clinical trials being conducted by the Alzheimer’s Prevention Initiative. Each of the studies is recruiting large populations of presymptomatic individuals at the highest imminent genetic risk for developing symptomatic Alzheimer’s disease. One study will enroll 2,000 residents of the Medellin, Colombia, area, home to the world’s largest kindred of carriers of the E280A PS1 mutation, which confers extreme high risk for early-onset Alzheimer’s disease. Participants must be close to the median age of clinical onset of E280A PS1-related Alzheimer’s disease, which is 47 years.
The other study will enroll roughly 50,000 North Americans aged 60-80 years, who will undergo ApoE genotyping. Those with two copies of the ApoE e4 allele are known to have a 91% risk of developing Alzheimer’s disease at a median age of onset of 68 years, while individuals with one copy have a 47% risk of Alzheimer’s dementia at an average age of onset of 75 years. Two copies are present in 3% of the North American population, while a single copy is present in 24%. The intervention arm of this study will consist of participants having two copies of ApoE e4.
These two studies will constitute the first real test of the amyloid hypothesis of Alzheimer’s dementia. Although probably 70% of researchers believe accumulation of some form of amyloid plays a critical early role in the development of Alzheimer’s disease, that hypothesis remains unproven as yet, Dr. Reiman noted.
An Alzheimer’s Prevention Initiative advisory panel comprising academic and pharmaceutical industry researchers is now in the process of selecting the first candidate amyloid-modifying preventive therapies for testing in these two studies. Participants will undergo serial brain amyloid imaging and biomarker measurements to evaluate treatment efficacy.
There are a plethora of amyloid-modifying interventions to choose from. These include dozens of investigational beta- and gamma-secretase inhibitors and antiaggregation medications, as well as active and passive amyloid immunization therapies.