INDIANAPOLIS – Obesity adds an estimated $164 million annually to the total hospital cost of major nonbariatric/nonobstetric operative procedures, Dr. Rodney J. Mason reported at the annual meeting of the American Surgical Association.
And that figure, audience members were swift to point out, is a very, very conservative estimate.
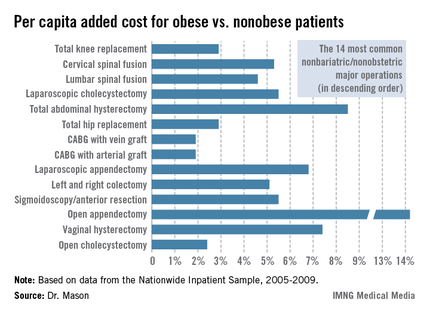
Dr. Mason presented an analysis of national cost estimates for obese vs. nonobese patients who underwent the 14 most common nonbariatric/nonobstetric major surgical procedures in the United States during 2005-2009 (see chart). He used data from the Nationwide Inpatient Sample (NIS) database sponsored by the Agency for Healthcare Research and Quality. The database provides detailed case information, including inpatient charges, from 20% of the nation’s hospitals.
One-quarter of the roughly 48 million hospitalized patients in the NIS database for this 5-year period underwent a major surgical procedure. Ten percent of patients who had 1 of the top 14 surgeries were obese. Dr. Mason and coworkers matched each of the 219,906 obese patients undergoing one of these operations to a nonobese patient who had the same operation; the tight one-to-one matching was based upon demographics and 28 defined comorbid conditions.
Because the NIS database records hospital charges, these charges had to be converted to estimated costs using a widely accepted formula. Once that was accomplished, the resultant annual total national estimated cost for the initial inpatient stay – not including physician costs – for patients undergoing one of the 14 surgical procedures was calculated at $4.38 billion in nonobese patients, compared with $4.55 billion in obese patients, for a $163,609,328 excess (3.7%) in the obese group, according to Dr. Mason of the University of Southern California, Los Angeles.
The mean per capita costs were $648 higher in obese than in nonobese surgical patients. To Dr. Mason’s surprise, this higher inpatient cost in the obese group was not driven by more postoperative complications; indeed, complication rates were equivalent in obese and nonobese patients. Instead, the explanation for the increased costs in the obese group was that they averaged a 0.025-day longer length of stay and they got significantly more secondary therapeutic, but not diagnostic, procedures.
Discussant Edward H. Livingston was sympathetic to the difficulties inherent in reliance upon the NIS database in conducting research, but he pointed out that the NIS is notoriously unreliable in recording obesity. This administrative database relies upon ICD-9 codes for obesity, and there’s good evidence that those codes often simply don’t get entered into the patient’s medical record. He noted that a mere 10% of the millions of surgical patients in the NIS database during the study years were categorized as obese, yet it’s well recognized that fully one-third of Americans are obese and another one-third are overweight. Clearly, then, a great many obese surgery patients were not captured in the study.
As for the study’s conclusion that the increased hospital costs in obese surgical patients were because of greater resource utilization and length of stay, Dr. Livingston said he thinks that’s probably all to the good.
"It may be that obese people do need more time in the hospital to recover and that they may need more resources to avoid more serious complications. We’ve learned how to better manage obese patients, and if those resources hadn’t been invested, then those patients might have done even worse," asserted Dr. Livingston, professor of surgery at the University of Texas Southwestern Medical Center, Dallas.
Taking care of obese patients is the reality of what physicians and surgeons deal with in hospitals now, he observed.
"Bariatric surgery has become the fifth most common operation in general surgery, and because of that we bariatric surgeons have taught everyone in the hospital how to take care of obese patients. We’ve learned over the years that there’s utility in using certain kinds of beds or having lifts available to move patients from one place to another. We’ve developed long instruments for facilitating laparoscopic surgery in obese patients. One of my own greatest learning experiences has been the utility of CPAP to manage morbidly obese patients in the postoperative period to help counter the effects of opiates and respiratory depression. The staff has become aware of how to take care of obese people and how to use medications appropriately in those people. All of that costs money," he said.
"Future research should aim to demonstrate that such costs are appropriate before Medicare does to us what it did with the so-called preventable complications, making a unilateral determination that we have too many complications or are spending too much money," the surgeon cautioned.