A predictive model identifying patients who will survive 2 years without recurrent mitral regurgitation after mitral valve repair has been developed by Dr. Irving L. Kron and his colleagues in the Cardiothoracic Surgical Trials Network.
The model, published in the March issue of the Journal of Thoracic and Cardiovascular Surgery, showed good discrimination (C-statistic = 0.82) and was developed using a subgroup analysis of a recent randomized trial of 251 patients by the CTSN (clinicaltrials.gov NCT00807040). The study also found that basal aneurysms and dyskinesis, which occurred commonly in the patient population, were strongly associated with recurrent moderate or severe MR.
The original trial compared complete chordal-sparing mitral valve (MV) replacement with MV repair with a complete downsized ring in patients with severe ischemic mitral regurgitation (MR). Ring size averaged 28.3 mm in men and 27.3 mm in women.
The subgroup analyzed the characteristics and outcomes of the 116 patients who were randomized to and received mitral valve repair, including 70 men (60%) with an overall mean age of around 69 years (6 of the patients were scheduled for repair, but received replacement instead when repair failed to correct MR in the operating room). Concomitant procedures occurred in 85% of the patients, including coronary bypass grafting (CABG), tricuspid valve repair (11%), atrial ablation (12%), and other (25%) (doi:10.1016/j.jtcvs,2014.10.120).
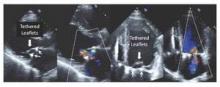
All of the 110 patients receiving successful repair had mild or less MR on intraoperative transesophageal echocardiography after repair. Subsequent transthoracic echocardiography follow-up showed the following MR recurrence for surviving patients: at 30 days: 24.8% moderate, 3.0% severe; at 6 months: 25.5% and 4.3%; at 12 months: 29.7% and 4.4%; and at 24 months: 39.0% and 1.3%. Mitral valve leaflet tethering was found to be the mechanism largely responsible for recurrent mitral regurgitation (Figure 1).
The mortality rate was 14.7% at 1 year, increasing to 19.8% at 2 years.
Overall, during the 2-year follow-up, among the 76 patients who developed moderate/severe MR recurrences or died, there were 53 MR recurrences, 13 MR recurrences plus death, and 10 deaths without recurrence.
The model originally assessed 30 variable candidates. Of these, the final model comprised 10 variables: age, body mass index, sex, race, effective regurgitant orifice area (EROA), basal aneurysm/dyskinesis, New York Heart Association class (NYHA), and prior CABG, percutaneous coronary intervention, or ventricular arrhythmias. None of the baseline echocardiographic measures of MV geometric tethering by themselves were associated with moderate/severe MR, but the presence of basal aneurysm/dyskinesis (52/116 or 45%) was strongly associated with this outcome.
The probabilities of recurrent MR or death estimated from the multivariable model yielded an area under the curve of 0.82; for recurrent MR, the receiver operating characteristic curve had an AUC of 0.83.
“We have developed a model that holds promise for predicting which patients will develop recurrent ischemic MR so that they can be better treated with MV replacement or more complex repair techniques that directly address leaflet tethering,” Dr. Kron and his colleagues concluded.
The study was funded by a cooperative agreement of the National Heart, Lung, and Blood Institute; the Canadian Institutes of Health Research; and the National Institute of Neurological Diseases and Stroke. Dr. Kron reported having no financial disclosures.