1. Fanikos J, Stapinski C, Koo S, et al. Medication errors associated with anticoagulant therapy in the hospital. Am J Cardiol 2004;94:532–5.
2. Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med2011;365:2002–12.
3. Institute for Safe Medication Practices. QuarterWatch. 9 January 2013. Available at http://www.ismp.org/quarterwatch/pdfs/2012Q2.pdf.
4. Hajjar ER, Hanlon JT, Artz MB, Let al. Adverse drug reaction risk factors in older outpatients. Am J Geriatr Pharmacother 2003;1:82–9.
5. Gurwitz JH, Field TS, Harrold LR, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA 2003;289:1107–16.
6. Singh S. Defining ‘elderly’ in clinical practice guidelines for pharmacotherapy. Pharm Pract 2014;12:489.
7. Singh S, Bajorek B. Pharmacotherapy in the aging patient: The impact of age per se (a review). Ageing Res Rev 2015 Jul 28. pii: S1568-1637(15)30008-8.
8. Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the anticoagulation and risk factors in atrial fibrillation (ATRIA) Study. JAMA 2001;285:2370–5.
9. Lip GY, Brechin CM, Lane DA. The global burden of atrial fibrillation and stroke: a systematic review of the epidemiology of atrial fibrillation in regions outside North America and Europe Chest 2012;142:1489–98.
10. Camm AJ, Lip GY, De Caterina R, et al. 2012 Focused update of the ESC guidelines for the management of atrial fibrillation: an update of the 2010 ESC guidelines for the management of atrial fibrillation-developed with the special contribution of the European Heart Rhythm Association Europace 2012;14:1385–413.
11. Kannel WB, Benjamin EJ. Status of the epidemiology of atrial fibrillation. Med Clin North Am 2008;92:17–40.
12. Chugh SS, Havmoeller R, Narayanan K, et al. Worldwide epidemiology of atrial fibrillation: a global burden 2010 study. Circulation 2014;129:837-47.
13. Miyasaka Y, Barnes ME, Gersh BJ, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation 2006;114:119–25.
14. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009;361:1139–51.
15. Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 2011;365:883–91.
16. Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 2011;365:981–92.
17. Apostolakis S, Lane DA, Guo Y, et al. Performance of the HEMORR2HAGES, ATRIA, and HAS-BLED Bleeding Risk–Prediction Scores in Patients With Atrial Fibrillation Undergoing Anticoagulation: The AMADEUS (Evaluating the Use of SR34006 Compared to Warfarin or Acenocoumarol in Patients With Atrial Fibrillation) Study. J Am Coll Cardiol 2012;60:861–7.
18. Fang MC, Go AS, Chang Y, et al. A new risk scheme to predict warfarin-associated hemorrhage: the ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation) study. J Am Coll Cardiol 2011;58:395–401.
19. Pisters R, Lane DA, Nieuwlaat R, et al. A novel user-friendly score (has-bled) to assess 1-year risk of major bleeding in patients with atrial fibrillation: The Euro Heart Survey. Chest 2010;138:1093–100.
20. Heidbuchel H, Verhamme P, Alings M, et al. Updated European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist anticoagulants in patients with non-valvular atrial fibrillation. Europace 2015;17:1467–507.
21. Lip GY, Frison L, Halperin JL, Lane DA. Comparative validation of a novel risk score for predicting bleeding risk in anticoagulated patients with atrial fibrillation: the HAS-BLED (Hypertension, Abnormal Renal/Liver Function, Stroke, Bleeding History or Predisposition, Labile INR, Elderly, Drugs/Alcohol Concomitantly) score. J Am Coll Cardiol 2011;57:173–80.
22. Roldán V, Marín F, Fernández H, et al. Predictive value of the HAS-BLED and ATRIA bleeding scores for the risk of serious bleeding in a "real-world" population with atrial fibrillation receiving anticoagulant therapy. Chest 2013;43:179–84.
23. Robert-Ebadi H, Le Gal G, Righini M. Use of anticoagulants in elderly patients: practical recommendations. Clin Interv Aging 2009;4:165–77.
24. Barcellona D, Contu P, Sorano GG, et al. The management of oral anticoagulant therapy: the patient's point of view. Thromb Haemost 2000;83:49–53.
25. Lancaster TR, Singer DE, Sheehan MA, et al. The impact of long-term warfarin therapy on quality of life. Evidence from a randomized trial. Boston Area Anticoagulation Trial for Atrial Fibrillation Investigators. Arch Intern Med 1991;151:1944–9.
26. Devereaux PJ, Anderson DR, Gardner MJ, et al. Differences between perspectives of physicians and patients on anticoagulation in patients with atrial fibrillation: observational study. BMJ 2001;323:1218–22.
27. Giugliano RP, Ruff CT, Braunwald E, Murphy SA. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med 2013;369:2093–104.
28. Barco S, Cheung YW, Eikelboom JW, Coppens M. New oral anticoagulants in elderly patients. Best Pract Res Clin Haematol 2013;26:215–24
29. Eikelboom JW, Wallentin L, Connolly SJ, et al. Risk of bleeding with 2 doses of dabigatran compared with warfarin in older and younger patients with atrial fibrillation: an analysis of the randomized evaluation of long-term anticoagulant therapy (RE-LY) trial. Circulation 2011;123:2363–72.
30. Coppens M, Eikelboom JW, Ezekowitz M, et al. Dabigatran versus warfarin in very elderly patients with atrial fibrillation: results from the RE-LY trial. Abstract. Circulation 2012;126:A15l537.
31. Halperin JL, Wojdyla D, Piccini JP, et al. Efficacy and safety of rivaroxaban compared with warfarin among elderly patients with nonvalvular atrial fibrillation in the ROCKET-AF trial. Abstract. Stroke 2012;43:A148.
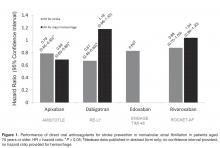
32. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet 2014;383:955–62
33. Clemens A, Strack A, Noack H, et al. Anticoagulant-related gastrointestinal bleeding—could this facilitate early detection of benign or malignant gastrointestinal lesions? Ann Med 2014;46:672–8.
34. Petty GW, Khandheria BK, Whisnant JP, et al. Predictors of cerebrovascular events and death among patients with valvular heart disease: A population-based study. Stroke 2000;31:2628–35.
35. Eikelboom JW, Connolly SJ, Brueckmann M, et al. Dabigatran versus warfarin in patients with mechanical heart valves. N Engl J Med 2013;369:1206–14.
36. Schomburg JL, Medina EM, Lahti MT, Bianco RW. Dabigatran versus warfarin after mechanical mitral valve replacement in the swine model. J Invest Surg 2012;25:150–5.
37. Douketis J, Bell AD, Eikelboom J, Liew A. Approach to the new oral anticoagulants in family practice: part 2: addressing frequently asked questions. Can Fam Physician 2014;60:997–1001.
38. Frost CE, Nepal S, Barrett YC, LaCreta F. Effects of age and gender on the singledose pharmacokinetics (PK) and pharmacodynamics (PD) of apixaban. Abstract. J Thromb Haemost 2009;7(Suppl 2):PP-MO-407..
39. Stangier J, Stahle H, Rathgen K et al. Pharmacokinetics and pharmacodynamics of the direct oral thrombin inhibitor dabigatran in healthy elderly subjects. Clin Pharmacokinet 2008;47:47–59.
40. Kubitza D, Becka M, Mueck W. The effect of extreme age, and gender on the pharmacology and tolerability of rivaroxaban, an oral direct factor Xa inhibitor. Blood 2006;108: Abstract 905.
41. Siegal DM, Crowther MA. Acute management of bleeding in patients on novel oral anticoagulants. Eur Heart J 2013;34:489–98.
42. Evans A, Kalra L. Are the results of randomized controlled trials on anticoagulation in patients with atrial fibrillation generalizable to clinical practice? Arch Intern Med 2001;161:1443–7.
43. Harper P, Young L, Merriman E. Bleeding risk with dabigatran in the frail elderly. N Engl J Med 2012;366:864–6.
44. Graham DJ, Reichman ME, Wernecke M, et al. Cardiovascular, bleeding, and mortality risks in elderly Medicare patients treated with dabigatran or warfarin for nonvalvular atrial fibrillation. Circulation 2015;131:157–64.
45. Avgil-Tsadok M, Jackevicius CA, Essebag V, et al. Dabigatran use in elderly patients with atrial fibrillation. Thromb Haemost 2015;115(1).
46. Uchino K, Hernandez AV. Dabigatran association with higher risk of acute coronary events: meta-analysis of noninferiority randomized controlled trials. Arch Intern Med 2012;172:397–402.
47. Halvorsen S, Atar D, Yang H, et al. Efficacy and safety of apixaban compared with warfarin according to age for stroke prevention in atrial fibrillation: observations from the ARISTOTLE trial. Eur Heart J 2014;35:1864–72.
48. Lega JC, Bertoletti L, Gremillet C, et al. Consistency of safety profile of new oral anticoagulants in patients with renal failure. J Thromb Haemost 2014;12:337–43.
49. Ng KH, Hart RG, Eikelboom JW. Anticoagulation in patients aged ≥ 75 years with atrial fibrillation: role of novel oral anticoagulants. Cardiol Ther 2013;2:135–49.
50. Kato ET, Guigliano RP, Ruff CT, et al. Efficacy and safety of edoxaban for the management of elderly patients with atrial fibrillation: Engage-AF TIMI 48. Circulation 2014;130:A16612.
51. Tripodi A. The laboratory and the new oral anticoagulants. Clin Chem 2013;59:353–62.
52. Tripodi A, Di Iorio G, Lippi G, et al. Position paper on laboratory testing for patients taking new oral anticoagulants. Consensus document of FCSA, SIMeL, SIBioC and CISMEL. Clin Chem Lab Med 2012;50:2137-40.
53. Heidbuchel H, Verhamme P, Alings M, et al. European Heart Rhythm Association Practical Guide on the use of new oral anticoagulants in patients with non-valvular atrial fibrillation. Europace 2013;15:625–51.
54. Chin PK, Wright DF, Patterson DM, et al. A proposal for dose-adjustment of dabigatran etexilate in atrial fibrillation guided by thrombin time. Br J Clin Pharmacol 2014;78:599–609.
55. Miyares MA, Davis K. Newer oral anticoagulants: a review of laboratory monitoring options and reversal agents in the hemorrhagic patient. Am J Health Syst Pharm 2012;69:1473–84.
56. Xarelto [package insert]. Titusville, NJ. Janssen Pharmaceuticals. September 2014.
57. Eliquis [package insert]. Princeton, NJ: Bristol-Meyers Squibb. June 2015.
58. Pradaxa [package insert]. Ridgefield, CT: Boehringer Ingelheim Pharmaceuticals. October 2010.
59. Savaysa [package insert]. Parsippany, NJ: Daiichi Sankyo. September 2015.
60. Michels WM, Grootendorst DC, Verduijn M, et al. Performance of the Cockcroft-Gault, MDRD, and new CKDEPI formulas in relation to GFR, age, and body size. Clin J Am Soc Nephrol 2010;5: 1003–9.
61. Poulsen BK, Grove EL, Husted SE. New oral anticoagulants: a review of the literature with particular emphasis on patients with impaired renal function. Drugs 2012;72:1739–53.
62. Hariharan S, Madabushi R. Clinical pharmacology basis of deriving dosing recommendations for dabigatran in patients with severe renal impairment. J Clin Pharmacol 2012;52:119S–25S.
63. Lehr T, Haertter S, Liesenfeld KH, et al. Dabigatran etexilate in atrial fibrillation patients with severe renal impairment: dose identification using pharmacokinetic modeling and simulation. J Clin Pharmacol 2012;52:1373–8.
64. Fox KAA, Piccini JP, Wojdyla D, et al. Prevention of stroke and systemic embolism with rivaroxaban compared with warfarin in patients with non-valvular atrial fibrillation and moderate renal impairment. Eur Heart J 2011;32:2387–94.
65. Pengo V, Crippa L, Falanga A et al. Questions and answers on the use of dabigatran and perspectives on the use of other new oral anticoagulants in patients with atrial fibrillation. A consensus document of the Italian Federation of Thrombosis Centers (FCSA). Thromb Haemost 2011;106:868–76.
66. Atkin PA, Veitch PC, Veitch EM, Ogle SJ. The epidemiology of serious adverse drug reactions among the elderly. Drugs Aging 1999;14:141–52.
67. Qato DM, Alexander GC, Conti RM, et al. Use of prescription and over-the-counter medications and dietary supplements among older adults in the United States. JAMA 2008;300:2867–78.
68. Skov J, Bladbjerg EM, Sidelmann J, et al. Plenty of pills: polypharmacy prevails in patients of a Danish anticoagulant clinic. Eur J Clin Pharmacol 2011;67:1169–74.
69. Ukena C, Bohm M, Schirmer SH. Hot topics in cardiology: data from IABP-SHOCK II, TRILOGY-ACS, WOEST, ALTIDUDE, FAME II and more. Clin Res Cardiol 2012;101):861–74.
70. Dewilde, Willem JM, Oirbans T, et al. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trial. Lancet;381:1107–15.
71. Shah SV, Gage BF. Cost-effectiveness of dabigatran for stroke prophylaxis in atrial fibrillation. Circulation 2011;123:
72. Sorensen SV, Kansal AR, Connolly S, et al. Cost-effectiveness of dabigatran etexilate for the prevention of stroke and systemic embolism in atrial fibrillation: a Canadian payer perspective. Thromb Haemost 2011;105:908–19.
73. Adcock AK, Lee-Iannotti JK, Aguilar MI, et al. Is dabigatran cost effective compared with warfarin for stroke prevention in atrial fibrillation?: a critically appraised topic. Neurologist 2012;18:102–7.
74. Kamel H, Johnston SC, Easton JD, Kim AS. Cost-effectiveness of dabigatran compared with warfarin for stroke prevention in patients with atrial fibrillation and prior stroke or transient ischemic attack. Stroke 2012;43:881–3.
75. Langkilde LK, Bergholdt AM, Overgaard M. Cost-effectiveness of dabigatran etexilate for stroke prevention in non-valvular atrial fibrillation. J Med Econ 2012;15:695-703.
76. Kansal AR, Sorensen SV, Gani R, et al. Cost-effectiveness of dabigatran etexilate for the prevention of stroke and systemic embolism in UK patients with atrial fibrillation. Heart 2012; 98:573–8.
77. Freeman JV, Zhu RP, Owens DK, et al. Cost-effectiveness of dabigatran compared with warfarin for stroke prevention in atrial fibrillation. Ann Intern Med 2011;154:1–11.
78. Pink J, Lane S, Pirmohamed M, Hughes DA. Dabigatran etexilate versus warfarin in management of non-valvular atrial fibrillation in UK context: quantitative benefit-harm and economic analyses. BMJ 2011;343:d6333.
79. Ali A, Bailey C, Abdelhafiz AH. Stroke prophylaxis with warfarin or dabigatran for patients with non-valvular atrial fibrillation-cost analysis. Age Ageing 2012;41:681–4.
80. Harrington AR, Armstrong EP, Nolan PE Jr, Malone DC. Cost effectiveness of apixaban, dabigatran, rivaroxaban, and warfarin for stroke prevention in atrial fibrillation. Stroke 2013;44:1676–81.
81. Amin A, Lingohr-Smith M, Bruno A, et al. Economic evaluations of medical cost differences: use of targeted-specific oral anticoagulants vs. warfarin among patients with nonvalvular atrial fibrillation and venous thromboembolism in the US. J Hematol Thrombo Dis 2015;3:209.
82. Lexicomp, Lexi-Drugs. Hudson, OH: Lexi-Comp.
83. U.S. Food and Drug Administration, Center for Drug Evaluation and Research. Apixaban NDA 202155/S-002 approval letter. Jan 30 2014. Available at http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2014/202155Orig1s002ltr.pdf
84. Hinojar R, Jimenez-Natcher JJ, Fernandez-Golfin C, Zamorano JL. New oral anticoagulants: a practical guide for physicians. Eur Heart J Cardiovasc Pharmacother 2015;1:134-45.
85. Connolly SJ, Eikelboom J, Joyner C, et al. Apixaban in patiets with atrial fibrillation. N Engl J Med 2011;364;806–17.