User login
Is female genital cosmetic surgery going mainstream?
Experts describe the field of female genital cosmetic surgery as the “Wild West,” but the lack of regulation and consensus has not kept it from exploding in recent years.
More than 10,000 labiaplasties were performed in 2016, a 23% jump over the previous year, and the procedures are offered by more than 35% of all plastic surgeons, according to data from the American Society for Aesthetic Plastic Surgery. As another indicator of increasing attention to the appearance of female genitalia, a 2013 survey of U.S. women revealed that more than 80% performed some sort of pubic hair grooming (JAMA Dermatol. 2016;152[10]:1106-13).
Dr. Iglesia recounted being contacted by a National Gallery of Art staff member, who, when confronted with Gustave Courbet’s L’Origine du Monde, an 1866 below-the-waist portrait of a nude woman, asked, “Is this normal? Do women have this much hair?” Dr. Iglesia said she reassured the staff member that the woman in the portrait did indeed have a normal female Tanner stage IV or V escutcheon. However, she said, social media and other images in the popular press have essentially erased female pubic hair from the public eye, even in explicit imagery that involves female nudity.
“This is an ideal that men and women are seeing in social media, in pornography, and even in the lay press.” And now, she said, “We’re in a new era of sex surgeries, with these ‘nips and tucks’ below the belt.”
Labiaplasty
The combination of a newly-hairless genital region, together with portrayals of adult women with a “Barbie doll” appearance, may contribute to women feeling self-conscious about labia minora protruding beyond the labia majora. Dr. Iglesia, who is section director for female pelvic medicine and reconstructive surgery at MedStar Washington Hospital Center, Washington, D.C., said this is true even though the normal length of labia minora can range from 7 mm to 5 cm.
That’s where labiaplasty comes in. The procedure, which can be performed with conventional surgical techniques or with a laser, is sometimes done for functional reasons.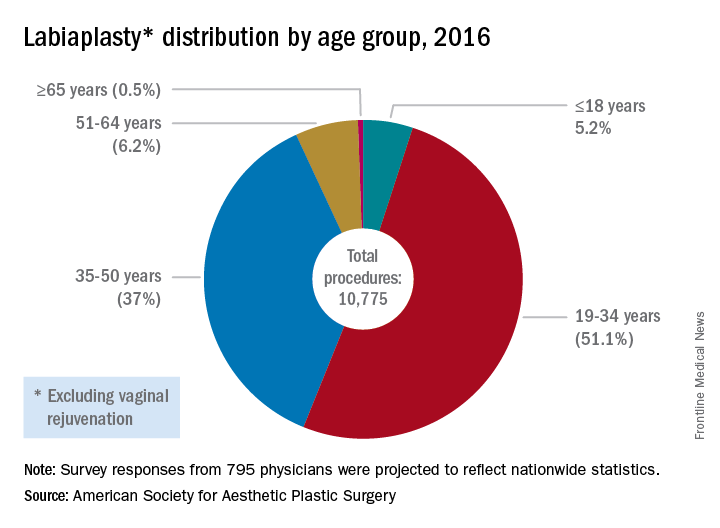
The waters are murkier when labiaplasty is performed for cosmetic reasons, to get that “Barbie doll” look, with some offices advertising the procedure as “designer lips,” Dr. Iglesia said.
In 2007, ACOG issued a committee opinion expressing concern about the lack of data and sometimes deceptive marketing practices surrounding a number of cosmetic vaginal surgeries (Obstet Gynecol 2007;110:737–8). The policy was reaffirmed in 2017.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/is-it-appropriate-to-perform-gynecologic-procedures-such-as-labiaplasty-for-cosmetic-reasons?iframe=1"}]Similarly, the Society of Obstetricians and Gynaecologists of Canada issued a 2013 statement about labiaplasty and other female genital cosmetic surgeries saying that “there is little evidence to support any of the female genital cosmetic surgeries in terms of improvement to sexual satisfaction or self-images. Physicians choosing to proceed with these cosmetic procedures should not promote these surgeries for the enhancement of sexual function and advertising of female genital cosmetic surgical procedures should be avoided.”
However, Mickey Karram, MD, who is director of the urogynecology program at Christ Hospital, Cincinnatti, said that informed consent is the key to dealing appropriately with these procedures.
“If a patient is physically bothered from a cosmetic standpoint that her labia are larger than she thinks they should be, and they are bothering her, is it appropriate or inappropriate to potentially discuss with her a labiaplasty?” Dr. Karram said at the ACOG meeting. For the patient who understands the risk and is also clear that the procedure is not medically necessary, he said he “feels strongly” that labiaplasty should be an option.
Fractional laser
The introduction of the fractional laser to gynecology is also adding to the debate about the appropriate integration of gynecologic procedures that may have nonmedical uses, such as vaginal “tightening.” Used primarily intravaginally, these devices have shallow penetration and are meant to stimulate collagen, proteoglycan, and hyaluronic acid synthesis with minimal tissue damage and downtime. One such device, the MonaLisa Touch, is marketed in the United States by Cynosure.
These energy sources hold great promise for the genitourinary syndrome of menopause (GSM) and other conditions, Dr. Karram said. “Many of these energy sources are being promoted for actual disease states, like vulvovaginal atrophy and lichen sclerosus,” he said.
Dr. Iglesia is not so sure: “This is not the fountain of youth.” She pointed out that the vasculature and innervation of the vagina and vulva are complex, with the outer one-eighth of the vagina being much more highly innervated. Laser treatment with a shallow penetration depth may not get at all of the issues that contribute to GSM.
“Is marketing ahead of the science? I would say yes,” she said. “There’s too much hype about this curing vaginal dryness and making your sex life better.”
Dr. Zahn also urged caution with the use of this technology. “The data are very limited, but, despite this, it’s become a very popular and highly-advertised approach. We need larger studies and more longitudinal data. This is especially true since one of the proposed ways this device works is by stimulating fibrosis. In every other body system, fibrosis stimulation may result in scarring. We have no idea if this is the case with this device. If it is, its application could result in worsening of bodily function, especially in regard to dyspareunia,” he said. “We clearly need more data.”
In 2016, ACOG issued a position statement about the fractional carbon dioxide and yttrium-aluminum-garnet laser systems that had received clearance from the Food and Drug Administration. The statement advised both ob.gyns. and patients that “this technology is, in fact, neither approved nor cleared by the FDA for the specific indication of treating vulvovaginal atrophy.”
Both Dr. Karram and Dr. Iglesia are investigators in an ongoing randomized, placebo- and sham-controlled trial comparing vaginal estrogen and laser therapy used both in conjunction and singly.
‘No-go’ procedures
Though Dr. Karram and Dr. Iglesia disagree on whether cosmetic labiaplasty is appropriate, they were in agreement that certain procedures are so untested, or have such potential risk with no proven benefit, that they should not be performed at all. The procedures on both physicians’ “no-go” lists included clitoral unhooding, G-spot amplification, “revirginification” in any form, vulval recontouring with autologous fat, and the so-called “O-shot,” injections of platelet-rich plasma that are touted as augmenting the sexual experience.
What’s to be done?
There is also agreement that a lack of common terminology is a significant problem. Step one, Dr. Karram said, is doing away with the term vaginal rejuvenation. “This is a terrible term. … There’s no real definition for this term.” He called for a multidisciplinary working group that would bring together gynecologists, plastic surgeons, and dermatologists to begin the work of terminology standardization.
From there, he proposed that the group develop a classification system that clarifies whether procedures are being done for cosmetic reasons, to enhance the sexual experience, or to address a specific disease state. Finally, he said, the group should recommend standardized outcome metrics that can be used to study the various interventions.
Dr. Zahn applauded this notion. “It’s a great point. I agree that multiple disciplines should be involved in examining outcomes, statistics, and criteria for evaluating procedures.”
And gynecologists should be leading this effort, Dr. Karram suggested. “Who knows this anatomy the best? We do.” He added, “If it’s going to be addressed, it should be addressed by us.”
But, Dr. Iglesia said she worries about vulnerable populations, such as adolescents and cancer survivors, who may undergo surgeries, for which the benefits may not outweigh the potential risks. For labiaplasty and laser resurfacing techniques, there have been a small number of studies on outcomes and patient satisfaction that have generally been conducted at single centers with no comparison arms and limited follow-up, she said.
“I also am concerned about pain, scarring, altered sensation, painful sex that could develop, wound complications, and what happens over time,” especially when these procedures may be performed on adolescents or women in their 20s or 30s who may later go on to have children, Dr. Iglesia said.
The question, she said, is not just whether gynecologists are better equipped than plastic surgeons or dermatologists to be performing female genital cosmetic surgery, “but should we be doing this at all?”
Dr. Zahn emphasized the need for evidence to guide decision making. “There has to be data that there is benefit and that the benefit outweighs the potential harm. There is no data on most cosmetic gynecologic procedures. If there are no data, they shouldn’t be done because we would not have the information necessary to appropriately counsel patients,” he said.
Dr. Karram has a financial relationship with Cynosure, which markets the MonaLisa Touch system in the United States. Dr. Iglesia reported that she had no relevant financial disclosures. Dr. Zahn is employed by ACOG.
koakes@frontlinemedcom.com
On Twitter @karioakes
Experts describe the field of female genital cosmetic surgery as the “Wild West,” but the lack of regulation and consensus has not kept it from exploding in recent years.
More than 10,000 labiaplasties were performed in 2016, a 23% jump over the previous year, and the procedures are offered by more than 35% of all plastic surgeons, according to data from the American Society for Aesthetic Plastic Surgery. As another indicator of increasing attention to the appearance of female genitalia, a 2013 survey of U.S. women revealed that more than 80% performed some sort of pubic hair grooming (JAMA Dermatol. 2016;152[10]:1106-13).
Dr. Iglesia recounted being contacted by a National Gallery of Art staff member, who, when confronted with Gustave Courbet’s L’Origine du Monde, an 1866 below-the-waist portrait of a nude woman, asked, “Is this normal? Do women have this much hair?” Dr. Iglesia said she reassured the staff member that the woman in the portrait did indeed have a normal female Tanner stage IV or V escutcheon. However, she said, social media and other images in the popular press have essentially erased female pubic hair from the public eye, even in explicit imagery that involves female nudity.
“This is an ideal that men and women are seeing in social media, in pornography, and even in the lay press.” And now, she said, “We’re in a new era of sex surgeries, with these ‘nips and tucks’ below the belt.”
Labiaplasty
The combination of a newly-hairless genital region, together with portrayals of adult women with a “Barbie doll” appearance, may contribute to women feeling self-conscious about labia minora protruding beyond the labia majora. Dr. Iglesia, who is section director for female pelvic medicine and reconstructive surgery at MedStar Washington Hospital Center, Washington, D.C., said this is true even though the normal length of labia minora can range from 7 mm to 5 cm.
That’s where labiaplasty comes in. The procedure, which can be performed with conventional surgical techniques or with a laser, is sometimes done for functional reasons.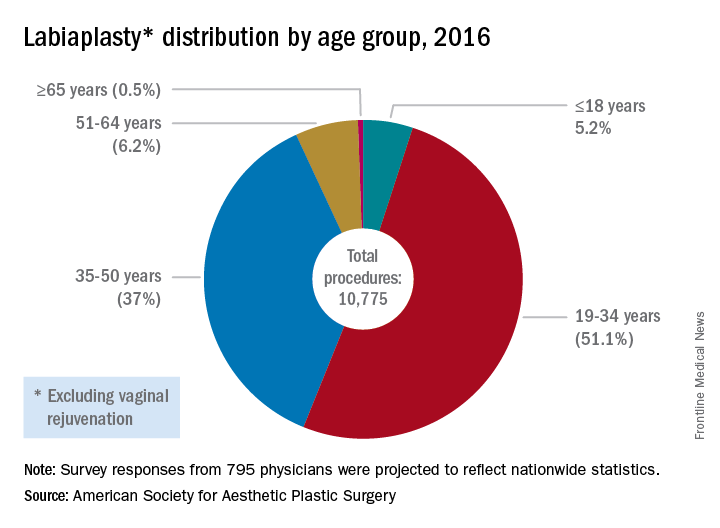
The waters are murkier when labiaplasty is performed for cosmetic reasons, to get that “Barbie doll” look, with some offices advertising the procedure as “designer lips,” Dr. Iglesia said.
In 2007, ACOG issued a committee opinion expressing concern about the lack of data and sometimes deceptive marketing practices surrounding a number of cosmetic vaginal surgeries (Obstet Gynecol 2007;110:737–8). The policy was reaffirmed in 2017.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/is-it-appropriate-to-perform-gynecologic-procedures-such-as-labiaplasty-for-cosmetic-reasons?iframe=1"}]Similarly, the Society of Obstetricians and Gynaecologists of Canada issued a 2013 statement about labiaplasty and other female genital cosmetic surgeries saying that “there is little evidence to support any of the female genital cosmetic surgeries in terms of improvement to sexual satisfaction or self-images. Physicians choosing to proceed with these cosmetic procedures should not promote these surgeries for the enhancement of sexual function and advertising of female genital cosmetic surgical procedures should be avoided.”
However, Mickey Karram, MD, who is director of the urogynecology program at Christ Hospital, Cincinnatti, said that informed consent is the key to dealing appropriately with these procedures.
“If a patient is physically bothered from a cosmetic standpoint that her labia are larger than she thinks they should be, and they are bothering her, is it appropriate or inappropriate to potentially discuss with her a labiaplasty?” Dr. Karram said at the ACOG meeting. For the patient who understands the risk and is also clear that the procedure is not medically necessary, he said he “feels strongly” that labiaplasty should be an option.
Fractional laser
The introduction of the fractional laser to gynecology is also adding to the debate about the appropriate integration of gynecologic procedures that may have nonmedical uses, such as vaginal “tightening.” Used primarily intravaginally, these devices have shallow penetration and are meant to stimulate collagen, proteoglycan, and hyaluronic acid synthesis with minimal tissue damage and downtime. One such device, the MonaLisa Touch, is marketed in the United States by Cynosure.
These energy sources hold great promise for the genitourinary syndrome of menopause (GSM) and other conditions, Dr. Karram said. “Many of these energy sources are being promoted for actual disease states, like vulvovaginal atrophy and lichen sclerosus,” he said.
Dr. Iglesia is not so sure: “This is not the fountain of youth.” She pointed out that the vasculature and innervation of the vagina and vulva are complex, with the outer one-eighth of the vagina being much more highly innervated. Laser treatment with a shallow penetration depth may not get at all of the issues that contribute to GSM.
“Is marketing ahead of the science? I would say yes,” she said. “There’s too much hype about this curing vaginal dryness and making your sex life better.”
Dr. Zahn also urged caution with the use of this technology. “The data are very limited, but, despite this, it’s become a very popular and highly-advertised approach. We need larger studies and more longitudinal data. This is especially true since one of the proposed ways this device works is by stimulating fibrosis. In every other body system, fibrosis stimulation may result in scarring. We have no idea if this is the case with this device. If it is, its application could result in worsening of bodily function, especially in regard to dyspareunia,” he said. “We clearly need more data.”
In 2016, ACOG issued a position statement about the fractional carbon dioxide and yttrium-aluminum-garnet laser systems that had received clearance from the Food and Drug Administration. The statement advised both ob.gyns. and patients that “this technology is, in fact, neither approved nor cleared by the FDA for the specific indication of treating vulvovaginal atrophy.”
Both Dr. Karram and Dr. Iglesia are investigators in an ongoing randomized, placebo- and sham-controlled trial comparing vaginal estrogen and laser therapy used both in conjunction and singly.
‘No-go’ procedures
Though Dr. Karram and Dr. Iglesia disagree on whether cosmetic labiaplasty is appropriate, they were in agreement that certain procedures are so untested, or have such potential risk with no proven benefit, that they should not be performed at all. The procedures on both physicians’ “no-go” lists included clitoral unhooding, G-spot amplification, “revirginification” in any form, vulval recontouring with autologous fat, and the so-called “O-shot,” injections of platelet-rich plasma that are touted as augmenting the sexual experience.
What’s to be done?
There is also agreement that a lack of common terminology is a significant problem. Step one, Dr. Karram said, is doing away with the term vaginal rejuvenation. “This is a terrible term. … There’s no real definition for this term.” He called for a multidisciplinary working group that would bring together gynecologists, plastic surgeons, and dermatologists to begin the work of terminology standardization.
From there, he proposed that the group develop a classification system that clarifies whether procedures are being done for cosmetic reasons, to enhance the sexual experience, or to address a specific disease state. Finally, he said, the group should recommend standardized outcome metrics that can be used to study the various interventions.
Dr. Zahn applauded this notion. “It’s a great point. I agree that multiple disciplines should be involved in examining outcomes, statistics, and criteria for evaluating procedures.”
And gynecologists should be leading this effort, Dr. Karram suggested. “Who knows this anatomy the best? We do.” He added, “If it’s going to be addressed, it should be addressed by us.”
But, Dr. Iglesia said she worries about vulnerable populations, such as adolescents and cancer survivors, who may undergo surgeries, for which the benefits may not outweigh the potential risks. For labiaplasty and laser resurfacing techniques, there have been a small number of studies on outcomes and patient satisfaction that have generally been conducted at single centers with no comparison arms and limited follow-up, she said.
“I also am concerned about pain, scarring, altered sensation, painful sex that could develop, wound complications, and what happens over time,” especially when these procedures may be performed on adolescents or women in their 20s or 30s who may later go on to have children, Dr. Iglesia said.
The question, she said, is not just whether gynecologists are better equipped than plastic surgeons or dermatologists to be performing female genital cosmetic surgery, “but should we be doing this at all?”
Dr. Zahn emphasized the need for evidence to guide decision making. “There has to be data that there is benefit and that the benefit outweighs the potential harm. There is no data on most cosmetic gynecologic procedures. If there are no data, they shouldn’t be done because we would not have the information necessary to appropriately counsel patients,” he said.
Dr. Karram has a financial relationship with Cynosure, which markets the MonaLisa Touch system in the United States. Dr. Iglesia reported that she had no relevant financial disclosures. Dr. Zahn is employed by ACOG.
koakes@frontlinemedcom.com
On Twitter @karioakes
Experts describe the field of female genital cosmetic surgery as the “Wild West,” but the lack of regulation and consensus has not kept it from exploding in recent years.
More than 10,000 labiaplasties were performed in 2016, a 23% jump over the previous year, and the procedures are offered by more than 35% of all plastic surgeons, according to data from the American Society for Aesthetic Plastic Surgery. As another indicator of increasing attention to the appearance of female genitalia, a 2013 survey of U.S. women revealed that more than 80% performed some sort of pubic hair grooming (JAMA Dermatol. 2016;152[10]:1106-13).
Dr. Iglesia recounted being contacted by a National Gallery of Art staff member, who, when confronted with Gustave Courbet’s L’Origine du Monde, an 1866 below-the-waist portrait of a nude woman, asked, “Is this normal? Do women have this much hair?” Dr. Iglesia said she reassured the staff member that the woman in the portrait did indeed have a normal female Tanner stage IV or V escutcheon. However, she said, social media and other images in the popular press have essentially erased female pubic hair from the public eye, even in explicit imagery that involves female nudity.
“This is an ideal that men and women are seeing in social media, in pornography, and even in the lay press.” And now, she said, “We’re in a new era of sex surgeries, with these ‘nips and tucks’ below the belt.”
Labiaplasty
The combination of a newly-hairless genital region, together with portrayals of adult women with a “Barbie doll” appearance, may contribute to women feeling self-conscious about labia minora protruding beyond the labia majora. Dr. Iglesia, who is section director for female pelvic medicine and reconstructive surgery at MedStar Washington Hospital Center, Washington, D.C., said this is true even though the normal length of labia minora can range from 7 mm to 5 cm.
That’s where labiaplasty comes in. The procedure, which can be performed with conventional surgical techniques or with a laser, is sometimes done for functional reasons.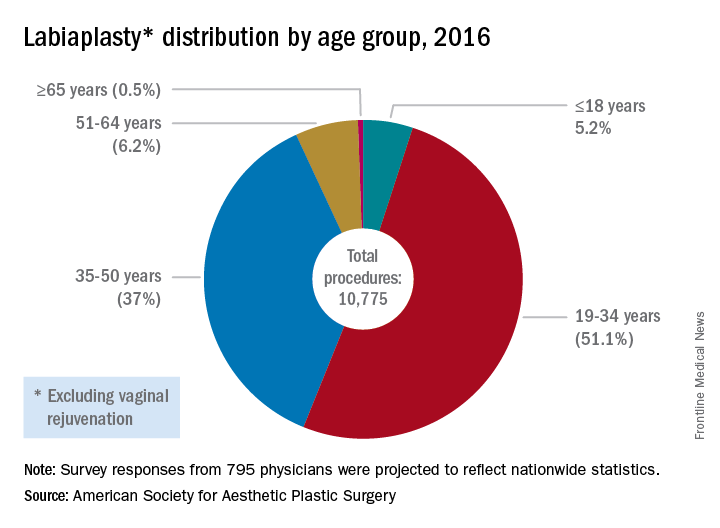
The waters are murkier when labiaplasty is performed for cosmetic reasons, to get that “Barbie doll” look, with some offices advertising the procedure as “designer lips,” Dr. Iglesia said.
In 2007, ACOG issued a committee opinion expressing concern about the lack of data and sometimes deceptive marketing practices surrounding a number of cosmetic vaginal surgeries (Obstet Gynecol 2007;110:737–8). The policy was reaffirmed in 2017.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/is-it-appropriate-to-perform-gynecologic-procedures-such-as-labiaplasty-for-cosmetic-reasons?iframe=1"}]Similarly, the Society of Obstetricians and Gynaecologists of Canada issued a 2013 statement about labiaplasty and other female genital cosmetic surgeries saying that “there is little evidence to support any of the female genital cosmetic surgeries in terms of improvement to sexual satisfaction or self-images. Physicians choosing to proceed with these cosmetic procedures should not promote these surgeries for the enhancement of sexual function and advertising of female genital cosmetic surgical procedures should be avoided.”
However, Mickey Karram, MD, who is director of the urogynecology program at Christ Hospital, Cincinnatti, said that informed consent is the key to dealing appropriately with these procedures.
“If a patient is physically bothered from a cosmetic standpoint that her labia are larger than she thinks they should be, and they are bothering her, is it appropriate or inappropriate to potentially discuss with her a labiaplasty?” Dr. Karram said at the ACOG meeting. For the patient who understands the risk and is also clear that the procedure is not medically necessary, he said he “feels strongly” that labiaplasty should be an option.
Fractional laser
The introduction of the fractional laser to gynecology is also adding to the debate about the appropriate integration of gynecologic procedures that may have nonmedical uses, such as vaginal “tightening.” Used primarily intravaginally, these devices have shallow penetration and are meant to stimulate collagen, proteoglycan, and hyaluronic acid synthesis with minimal tissue damage and downtime. One such device, the MonaLisa Touch, is marketed in the United States by Cynosure.
These energy sources hold great promise for the genitourinary syndrome of menopause (GSM) and other conditions, Dr. Karram said. “Many of these energy sources are being promoted for actual disease states, like vulvovaginal atrophy and lichen sclerosus,” he said.
Dr. Iglesia is not so sure: “This is not the fountain of youth.” She pointed out that the vasculature and innervation of the vagina and vulva are complex, with the outer one-eighth of the vagina being much more highly innervated. Laser treatment with a shallow penetration depth may not get at all of the issues that contribute to GSM.
“Is marketing ahead of the science? I would say yes,” she said. “There’s too much hype about this curing vaginal dryness and making your sex life better.”
Dr. Zahn also urged caution with the use of this technology. “The data are very limited, but, despite this, it’s become a very popular and highly-advertised approach. We need larger studies and more longitudinal data. This is especially true since one of the proposed ways this device works is by stimulating fibrosis. In every other body system, fibrosis stimulation may result in scarring. We have no idea if this is the case with this device. If it is, its application could result in worsening of bodily function, especially in regard to dyspareunia,” he said. “We clearly need more data.”
In 2016, ACOG issued a position statement about the fractional carbon dioxide and yttrium-aluminum-garnet laser systems that had received clearance from the Food and Drug Administration. The statement advised both ob.gyns. and patients that “this technology is, in fact, neither approved nor cleared by the FDA for the specific indication of treating vulvovaginal atrophy.”
Both Dr. Karram and Dr. Iglesia are investigators in an ongoing randomized, placebo- and sham-controlled trial comparing vaginal estrogen and laser therapy used both in conjunction and singly.
‘No-go’ procedures
Though Dr. Karram and Dr. Iglesia disagree on whether cosmetic labiaplasty is appropriate, they were in agreement that certain procedures are so untested, or have such potential risk with no proven benefit, that they should not be performed at all. The procedures on both physicians’ “no-go” lists included clitoral unhooding, G-spot amplification, “revirginification” in any form, vulval recontouring with autologous fat, and the so-called “O-shot,” injections of platelet-rich plasma that are touted as augmenting the sexual experience.
What’s to be done?
There is also agreement that a lack of common terminology is a significant problem. Step one, Dr. Karram said, is doing away with the term vaginal rejuvenation. “This is a terrible term. … There’s no real definition for this term.” He called for a multidisciplinary working group that would bring together gynecologists, plastic surgeons, and dermatologists to begin the work of terminology standardization.
From there, he proposed that the group develop a classification system that clarifies whether procedures are being done for cosmetic reasons, to enhance the sexual experience, or to address a specific disease state. Finally, he said, the group should recommend standardized outcome metrics that can be used to study the various interventions.
Dr. Zahn applauded this notion. “It’s a great point. I agree that multiple disciplines should be involved in examining outcomes, statistics, and criteria for evaluating procedures.”
And gynecologists should be leading this effort, Dr. Karram suggested. “Who knows this anatomy the best? We do.” He added, “If it’s going to be addressed, it should be addressed by us.”
But, Dr. Iglesia said she worries about vulnerable populations, such as adolescents and cancer survivors, who may undergo surgeries, for which the benefits may not outweigh the potential risks. For labiaplasty and laser resurfacing techniques, there have been a small number of studies on outcomes and patient satisfaction that have generally been conducted at single centers with no comparison arms and limited follow-up, she said.
“I also am concerned about pain, scarring, altered sensation, painful sex that could develop, wound complications, and what happens over time,” especially when these procedures may be performed on adolescents or women in their 20s or 30s who may later go on to have children, Dr. Iglesia said.
The question, she said, is not just whether gynecologists are better equipped than plastic surgeons or dermatologists to be performing female genital cosmetic surgery, “but should we be doing this at all?”
Dr. Zahn emphasized the need for evidence to guide decision making. “There has to be data that there is benefit and that the benefit outweighs the potential harm. There is no data on most cosmetic gynecologic procedures. If there are no data, they shouldn’t be done because we would not have the information necessary to appropriately counsel patients,” he said.
Dr. Karram has a financial relationship with Cynosure, which markets the MonaLisa Touch system in the United States. Dr. Iglesia reported that she had no relevant financial disclosures. Dr. Zahn is employed by ACOG.
koakes@frontlinemedcom.com
On Twitter @karioakes
Female genital mutilation is seen by most ob.gyns.
SAN DIEGO – Nearly 60% of ob.gyns. have seen patients who have experienced female genital mutilation (FGM), according to the results of a survey of 288 fellows of the American College of Obstetricians and Gynecologists.
Additionally, the survey found that there are few guidelines for care of these patients. Among fellows who had seen patients with FGM, 80.1% said their institutions had no policies or guidelines for management of these patients. Additionally, just 56.7% of fellows who had treated these women were aware that federal laws prohibit FGM.
The findings came as a surprise to the study’s senior author, Alireza Shamshirsaz, MD, a maternal-fetal medicine specialist at Baylor College of Medicine, Houston. “I really see the gap of knowledge of [ob.gyns.] in the States, and the emergent need for guidelines and regulation.”
Ob.gyns. who cared for women who had experienced FGM reported that they used a combination of approaches in treating these patients. Nearly half of physicians (45.8%) said they generally treated FGM patients the same as their other patients, but nearly three-quarters said they also discuss potential complications of FGM procedures. About 28% of physicians reported providing information about surgical repair options, while less than 5% provided mental health referrals.
For minors who had experienced FGM, low numbers of survey respondents made law enforcement referrals (7.7%) or social service referrals (7.7%). There were a few respondents (5.4%) who said they didn’t feel comfortable managing patients who had experienced FGM.
In another surprise to the researchers, genital mutilation procedures were not all performed abroad. Three ob.gyns. reported caring for patients who had previously undergone FGM in the United States.
The findings highlight the need for structured education in ob.gyn. residency training programs regarding how to approach at-risk patients and those who have experienced FGM, Dr. Shamshirsaz said in an interview. He also called for specific guidelines from ACOG regarding virginity testing and hymenoplasty and for clearer statutes to guide physicians when patients request FGM or virginity testing procedures.
“All [ob.gyns.] should be aware that their at-risk patients may have a history of honor-related practices and should obtain a full history in a culturally sensitive and professionally responsible manner so that they may respond to and address the unique needs of these patients,” the researchers wrote.
The researchers reported having no relevant financial disclosures. The study was supported by a grant from ACOG.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN DIEGO – Nearly 60% of ob.gyns. have seen patients who have experienced female genital mutilation (FGM), according to the results of a survey of 288 fellows of the American College of Obstetricians and Gynecologists.
Additionally, the survey found that there are few guidelines for care of these patients. Among fellows who had seen patients with FGM, 80.1% said their institutions had no policies or guidelines for management of these patients. Additionally, just 56.7% of fellows who had treated these women were aware that federal laws prohibit FGM.
The findings came as a surprise to the study’s senior author, Alireza Shamshirsaz, MD, a maternal-fetal medicine specialist at Baylor College of Medicine, Houston. “I really see the gap of knowledge of [ob.gyns.] in the States, and the emergent need for guidelines and regulation.”
Ob.gyns. who cared for women who had experienced FGM reported that they used a combination of approaches in treating these patients. Nearly half of physicians (45.8%) said they generally treated FGM patients the same as their other patients, but nearly three-quarters said they also discuss potential complications of FGM procedures. About 28% of physicians reported providing information about surgical repair options, while less than 5% provided mental health referrals.
For minors who had experienced FGM, low numbers of survey respondents made law enforcement referrals (7.7%) or social service referrals (7.7%). There were a few respondents (5.4%) who said they didn’t feel comfortable managing patients who had experienced FGM.
In another surprise to the researchers, genital mutilation procedures were not all performed abroad. Three ob.gyns. reported caring for patients who had previously undergone FGM in the United States.
The findings highlight the need for structured education in ob.gyn. residency training programs regarding how to approach at-risk patients and those who have experienced FGM, Dr. Shamshirsaz said in an interview. He also called for specific guidelines from ACOG regarding virginity testing and hymenoplasty and for clearer statutes to guide physicians when patients request FGM or virginity testing procedures.
“All [ob.gyns.] should be aware that their at-risk patients may have a history of honor-related practices and should obtain a full history in a culturally sensitive and professionally responsible manner so that they may respond to and address the unique needs of these patients,” the researchers wrote.
The researchers reported having no relevant financial disclosures. The study was supported by a grant from ACOG.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN DIEGO – Nearly 60% of ob.gyns. have seen patients who have experienced female genital mutilation (FGM), according to the results of a survey of 288 fellows of the American College of Obstetricians and Gynecologists.
Additionally, the survey found that there are few guidelines for care of these patients. Among fellows who had seen patients with FGM, 80.1% said their institutions had no policies or guidelines for management of these patients. Additionally, just 56.7% of fellows who had treated these women were aware that federal laws prohibit FGM.
The findings came as a surprise to the study’s senior author, Alireza Shamshirsaz, MD, a maternal-fetal medicine specialist at Baylor College of Medicine, Houston. “I really see the gap of knowledge of [ob.gyns.] in the States, and the emergent need for guidelines and regulation.”
Ob.gyns. who cared for women who had experienced FGM reported that they used a combination of approaches in treating these patients. Nearly half of physicians (45.8%) said they generally treated FGM patients the same as their other patients, but nearly three-quarters said they also discuss potential complications of FGM procedures. About 28% of physicians reported providing information about surgical repair options, while less than 5% provided mental health referrals.
For minors who had experienced FGM, low numbers of survey respondents made law enforcement referrals (7.7%) or social service referrals (7.7%). There were a few respondents (5.4%) who said they didn’t feel comfortable managing patients who had experienced FGM.
In another surprise to the researchers, genital mutilation procedures were not all performed abroad. Three ob.gyns. reported caring for patients who had previously undergone FGM in the United States.
The findings highlight the need for structured education in ob.gyn. residency training programs regarding how to approach at-risk patients and those who have experienced FGM, Dr. Shamshirsaz said in an interview. He also called for specific guidelines from ACOG regarding virginity testing and hymenoplasty and for clearer statutes to guide physicians when patients request FGM or virginity testing procedures.
“All [ob.gyns.] should be aware that their at-risk patients may have a history of honor-related practices and should obtain a full history in a culturally sensitive and professionally responsible manner so that they may respond to and address the unique needs of these patients,” the researchers wrote.
The researchers reported having no relevant financial disclosures. The study was supported by a grant from ACOG.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT ACOG 2017
Key clinical point:
Major finding: Of the 288 ACOG fellows surveyed, 58.6% have seen patients who have experienced female genital mutilation.
Data source: An anonymous online survey of 288 randomly-selected and stratified ACOG fellows.
Disclosures: The study was supported by a grant from ACOG. The researchers reported having no relevant financial disclosures.
LARCs are underutilized, even where Zika risk is high
SAN DIEGO – Los Angeles County officials report that few women surveyed are using the most effective contraceptive measures, a fact that concerns public health officials in an area at potential risk for local Zika virus infection.
With close to half of the births in Los Angeles County being unplanned and more than 59% of women reporting use of less effective contraceptive measures, educating providers on the why and the how of placing the most effective contraceptive measures could make a big difference, said Diana Ramos, MD, of the Los Angeles County Department of Public Health.
Los Angeles-area health care providers and public health officials are bracing themselves for a summer mosquito population explosion brought on by the West Coast’s very wet winter and spring of 2016-2017, Dr. Ramos said during a press briefing at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
This sets up the very real possibility of local transmission in the Los Angeles area in the summer of 2017, Dr. Ramos said, adding that the county has both Aedes aegypti and Aedes albopictus mosquitoes, two species capable of transmitting Zika virus.
Dr. Ramos and her colleagues drew from the Los Angeles Mommy and Baby (LAMB) project, a population-based survey of women who have recently given birth. As part of ongoing surveillance to assess whether the county is meeting the CDC’s Healthy People 2020 goals, the 2012 LAMB survey asked about preconception and perinatal experiences, including family planning methods used. From the 2012 survey, the investigators could then identify women who had not had a subsequent pregnancy. They excluded women who did not complete the family planning portion of the 2012 survey. A total of 3,175 women were queried in 2014 about their current family planning practices.
Overall, 28% of women said that they were using not using any form of birth control. The remaining women (n = 2,400) used a variety of methods, with condoms being the most common, used by 38.1%. Oral contraceptives were used by 15.6% of respondents, but nearly as many (14.8%) reported using the withdrawal method, and 6.1% said they used the rhythm method. An additional 15% reported that either they or their partner had undergone a permanent sterilization procedure. Vaginal rings were used by 1.7%.
Of the remaining women who were using birth control, 14.5% were using intrauterine devices, and 6.1% were using depot medroxyprogesterone acetate. These two methods of long-acting reversible contraception (LARC) represent some of the most effective methods to prevent conception, Dr. Ramos said. The fact that only one in five women is using these methods leaves room for provider and public education, she said.
Though some women used a combination of methods, the researchers estimated that about 59% of the women using any birth control were using methods proven to be less effective in real-world studies, including condoms, withdrawal, and the rhythm method.
Accordingly, she said her department is working with providers to expand awareness of the high efficacy rates and good safety profiles of LARCs, and also to educate the public that “the most effective contraceptive methods can decrease neonatal Zika complications by preventing unplanned pregnancies.” The hope, Dr. Ramos said, is to decrease the number of neonatal Zika cases.
Dr. Ramos and her coauthors reported no external sources of funding and no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN DIEGO – Los Angeles County officials report that few women surveyed are using the most effective contraceptive measures, a fact that concerns public health officials in an area at potential risk for local Zika virus infection.
With close to half of the births in Los Angeles County being unplanned and more than 59% of women reporting use of less effective contraceptive measures, educating providers on the why and the how of placing the most effective contraceptive measures could make a big difference, said Diana Ramos, MD, of the Los Angeles County Department of Public Health.
Los Angeles-area health care providers and public health officials are bracing themselves for a summer mosquito population explosion brought on by the West Coast’s very wet winter and spring of 2016-2017, Dr. Ramos said during a press briefing at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
This sets up the very real possibility of local transmission in the Los Angeles area in the summer of 2017, Dr. Ramos said, adding that the county has both Aedes aegypti and Aedes albopictus mosquitoes, two species capable of transmitting Zika virus.
Dr. Ramos and her colleagues drew from the Los Angeles Mommy and Baby (LAMB) project, a population-based survey of women who have recently given birth. As part of ongoing surveillance to assess whether the county is meeting the CDC’s Healthy People 2020 goals, the 2012 LAMB survey asked about preconception and perinatal experiences, including family planning methods used. From the 2012 survey, the investigators could then identify women who had not had a subsequent pregnancy. They excluded women who did not complete the family planning portion of the 2012 survey. A total of 3,175 women were queried in 2014 about their current family planning practices.
Overall, 28% of women said that they were using not using any form of birth control. The remaining women (n = 2,400) used a variety of methods, with condoms being the most common, used by 38.1%. Oral contraceptives were used by 15.6% of respondents, but nearly as many (14.8%) reported using the withdrawal method, and 6.1% said they used the rhythm method. An additional 15% reported that either they or their partner had undergone a permanent sterilization procedure. Vaginal rings were used by 1.7%.
Of the remaining women who were using birth control, 14.5% were using intrauterine devices, and 6.1% were using depot medroxyprogesterone acetate. These two methods of long-acting reversible contraception (LARC) represent some of the most effective methods to prevent conception, Dr. Ramos said. The fact that only one in five women is using these methods leaves room for provider and public education, she said.
Though some women used a combination of methods, the researchers estimated that about 59% of the women using any birth control were using methods proven to be less effective in real-world studies, including condoms, withdrawal, and the rhythm method.
Accordingly, she said her department is working with providers to expand awareness of the high efficacy rates and good safety profiles of LARCs, and also to educate the public that “the most effective contraceptive methods can decrease neonatal Zika complications by preventing unplanned pregnancies.” The hope, Dr. Ramos said, is to decrease the number of neonatal Zika cases.
Dr. Ramos and her coauthors reported no external sources of funding and no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN DIEGO – Los Angeles County officials report that few women surveyed are using the most effective contraceptive measures, a fact that concerns public health officials in an area at potential risk for local Zika virus infection.
With close to half of the births in Los Angeles County being unplanned and more than 59% of women reporting use of less effective contraceptive measures, educating providers on the why and the how of placing the most effective contraceptive measures could make a big difference, said Diana Ramos, MD, of the Los Angeles County Department of Public Health.
Los Angeles-area health care providers and public health officials are bracing themselves for a summer mosquito population explosion brought on by the West Coast’s very wet winter and spring of 2016-2017, Dr. Ramos said during a press briefing at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
This sets up the very real possibility of local transmission in the Los Angeles area in the summer of 2017, Dr. Ramos said, adding that the county has both Aedes aegypti and Aedes albopictus mosquitoes, two species capable of transmitting Zika virus.
Dr. Ramos and her colleagues drew from the Los Angeles Mommy and Baby (LAMB) project, a population-based survey of women who have recently given birth. As part of ongoing surveillance to assess whether the county is meeting the CDC’s Healthy People 2020 goals, the 2012 LAMB survey asked about preconception and perinatal experiences, including family planning methods used. From the 2012 survey, the investigators could then identify women who had not had a subsequent pregnancy. They excluded women who did not complete the family planning portion of the 2012 survey. A total of 3,175 women were queried in 2014 about their current family planning practices.
Overall, 28% of women said that they were using not using any form of birth control. The remaining women (n = 2,400) used a variety of methods, with condoms being the most common, used by 38.1%. Oral contraceptives were used by 15.6% of respondents, but nearly as many (14.8%) reported using the withdrawal method, and 6.1% said they used the rhythm method. An additional 15% reported that either they or their partner had undergone a permanent sterilization procedure. Vaginal rings were used by 1.7%.
Of the remaining women who were using birth control, 14.5% were using intrauterine devices, and 6.1% were using depot medroxyprogesterone acetate. These two methods of long-acting reversible contraception (LARC) represent some of the most effective methods to prevent conception, Dr. Ramos said. The fact that only one in five women is using these methods leaves room for provider and public education, she said.
Though some women used a combination of methods, the researchers estimated that about 59% of the women using any birth control were using methods proven to be less effective in real-world studies, including condoms, withdrawal, and the rhythm method.
Accordingly, she said her department is working with providers to expand awareness of the high efficacy rates and good safety profiles of LARCs, and also to educate the public that “the most effective contraceptive methods can decrease neonatal Zika complications by preventing unplanned pregnancies.” The hope, Dr. Ramos said, is to decrease the number of neonatal Zika cases.
Dr. Ramos and her coauthors reported no external sources of funding and no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT ACOG 2017
Key clinical point:
Major finding: Of women surveyed who were using contraception, 20.6% were using a highly effective long-acting reversible contraceptive.
Data source: A population-based survey of 3,175 women in Los Angeles County who had previously given birth.
Disclosures: The study authors reported no outside sources of funding and no conflicts of interest.
Cervical cancer screening adherence drops after HPV vaccination
SAN DIEGO – Young adult women who received the human papillomavirus (HPV) vaccination were less likely to adhere to the recommended screening schedule for cervical cancer, according to a recent study.
In looking at a cohort of women who received at least two Pap smears during a 4-year study period, Daniel Terk, MD, and his colleagues saw a significant drop-off in screening visits after women received their HPV vaccinations. The group of women who received their vaccine midstudy were significantly less likely to come in for annual screening after their vaccination than before (n = 140, adjusted odds ratio 0.19, 95% confidence interval, 0.08-0.49).
The retrospective chart review looked at rates of cervical cancer screening and HPV vaccination across 943 patient charts, beginning in 2006 when the HPV vaccine was released and ending in 2010. The inclusion criteria ensured that “participants were old enough to obtain cervical cancer screening and young enough to receive the HPV vaccine,” Dr. Terk and his collaborators wrote in the research abstract.
The drop-off in adherence for the subgroup who received their vaccines midstudy was an isolated finding, said Dr. Terk, noting that vaccination status did not affect adherence to the recommended screening schedule for the group as a whole.
Billing data and medical records were used to track HPV vaccination status and dates of administration, as well as the dates of testing and results for cervical cancer screening. Patients were included if they were born from 1980 to 1988, if they had two or more Pap smears during the study period, and if their HPV vaccination status could be verified. Patients with an initial abnormal Pap smear or a prior loop electrosurgical excision procedure were excluded, as were patients whose HPV vaccination status could not be confirmed.
In all, 943 patient charts were included in the review; 448 patients had no documented vaccination, with further review showing that 418 of these had, in fact, not been vaccinated, while the remaining 30 had actually had at least one HPV vaccine dose during the study period. Of the 495 patients with at least one documented vaccination, 175 had at least one Pap smear done before they were vaccinated, while 320 had their HPV vaccine before any documented cervical cancer screening.
Thus, there were two patient groups: 593 “unvaccinated” patients, who had at least one cervical cancer screening before receiving the vaccine, and 350 “vaccinated” patients, who had their HPV vaccine before any documented Pap smears.
Dr. Terk and his colleagues considered a screening interval of 18 months or less appropriate, while a longer interval than that between Pap smears was considered inappropriate timing. Individual patients were considered adherent if 76%-100% of their Pap smears were appropriately timed, partially adherent if 50%-75% of their Pap smears were appropriately timed, and not adherent if less than 50% of their Pap smears were appropriately timed.
Of those receiving their vaccine midstudy, 116 (82.9%) were adherent before vaccination, while 69 (49.3%) were adherent after vaccination.
The HPV vaccine is highly effective at preventing infection with the strains of HPV that are primarily responsible for cervical cancer. At the same time, about 70% of the cervical cancer cases that occur are associated with missed screening or inappropriate screening intervals, so screening is still an important part of the strategy to prevent cervical cancers, said Dr. Terk, a 4th-year ob.gyn. resident at the University of Rochester, N.Y.
The ACOG guidelines for cervical cancer screening have shifted through the years. During the period from 2003 to 2009, annual Pap smears were recommended for women under the age of 30 years, beginning at age 21 or 3 years after first sexual intercourse. Women 30 years and older who were at low risk could have a less frequent screening interval. ACOG currently recommends Pap testing alone every 3 years for women aged 21-29 years; co-testing with a Pap test and an HPV test every 5 years in women aged 30-65 years, or a Pap test alone every 3 years.
The study had a large sample size, and adherence rates track with national data, Dr. Terk said. However, screening guidelines have shifted in recent years, and vaccinations are now happening at a much younger age, so the findings should be interpreted with some caution. Still, he said, clinicians should incorporate a strong message about the importance of cervical cancer screening in their HPV vaccination and well-woman counseling.
Dr. Terk reported having no relevant financial disclosures and reported no outside sources of funding.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN DIEGO – Young adult women who received the human papillomavirus (HPV) vaccination were less likely to adhere to the recommended screening schedule for cervical cancer, according to a recent study.
In looking at a cohort of women who received at least two Pap smears during a 4-year study period, Daniel Terk, MD, and his colleagues saw a significant drop-off in screening visits after women received their HPV vaccinations. The group of women who received their vaccine midstudy were significantly less likely to come in for annual screening after their vaccination than before (n = 140, adjusted odds ratio 0.19, 95% confidence interval, 0.08-0.49).
The retrospective chart review looked at rates of cervical cancer screening and HPV vaccination across 943 patient charts, beginning in 2006 when the HPV vaccine was released and ending in 2010. The inclusion criteria ensured that “participants were old enough to obtain cervical cancer screening and young enough to receive the HPV vaccine,” Dr. Terk and his collaborators wrote in the research abstract.
The drop-off in adherence for the subgroup who received their vaccines midstudy was an isolated finding, said Dr. Terk, noting that vaccination status did not affect adherence to the recommended screening schedule for the group as a whole.
Billing data and medical records were used to track HPV vaccination status and dates of administration, as well as the dates of testing and results for cervical cancer screening. Patients were included if they were born from 1980 to 1988, if they had two or more Pap smears during the study period, and if their HPV vaccination status could be verified. Patients with an initial abnormal Pap smear or a prior loop electrosurgical excision procedure were excluded, as were patients whose HPV vaccination status could not be confirmed.
In all, 943 patient charts were included in the review; 448 patients had no documented vaccination, with further review showing that 418 of these had, in fact, not been vaccinated, while the remaining 30 had actually had at least one HPV vaccine dose during the study period. Of the 495 patients with at least one documented vaccination, 175 had at least one Pap smear done before they were vaccinated, while 320 had their HPV vaccine before any documented cervical cancer screening.
Thus, there were two patient groups: 593 “unvaccinated” patients, who had at least one cervical cancer screening before receiving the vaccine, and 350 “vaccinated” patients, who had their HPV vaccine before any documented Pap smears.
Dr. Terk and his colleagues considered a screening interval of 18 months or less appropriate, while a longer interval than that between Pap smears was considered inappropriate timing. Individual patients were considered adherent if 76%-100% of their Pap smears were appropriately timed, partially adherent if 50%-75% of their Pap smears were appropriately timed, and not adherent if less than 50% of their Pap smears were appropriately timed.
Of those receiving their vaccine midstudy, 116 (82.9%) were adherent before vaccination, while 69 (49.3%) were adherent after vaccination.
The HPV vaccine is highly effective at preventing infection with the strains of HPV that are primarily responsible for cervical cancer. At the same time, about 70% of the cervical cancer cases that occur are associated with missed screening or inappropriate screening intervals, so screening is still an important part of the strategy to prevent cervical cancers, said Dr. Terk, a 4th-year ob.gyn. resident at the University of Rochester, N.Y.
The ACOG guidelines for cervical cancer screening have shifted through the years. During the period from 2003 to 2009, annual Pap smears were recommended for women under the age of 30 years, beginning at age 21 or 3 years after first sexual intercourse. Women 30 years and older who were at low risk could have a less frequent screening interval. ACOG currently recommends Pap testing alone every 3 years for women aged 21-29 years; co-testing with a Pap test and an HPV test every 5 years in women aged 30-65 years, or a Pap test alone every 3 years.
The study had a large sample size, and adherence rates track with national data, Dr. Terk said. However, screening guidelines have shifted in recent years, and vaccinations are now happening at a much younger age, so the findings should be interpreted with some caution. Still, he said, clinicians should incorporate a strong message about the importance of cervical cancer screening in their HPV vaccination and well-woman counseling.
Dr. Terk reported having no relevant financial disclosures and reported no outside sources of funding.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN DIEGO – Young adult women who received the human papillomavirus (HPV) vaccination were less likely to adhere to the recommended screening schedule for cervical cancer, according to a recent study.
In looking at a cohort of women who received at least two Pap smears during a 4-year study period, Daniel Terk, MD, and his colleagues saw a significant drop-off in screening visits after women received their HPV vaccinations. The group of women who received their vaccine midstudy were significantly less likely to come in for annual screening after their vaccination than before (n = 140, adjusted odds ratio 0.19, 95% confidence interval, 0.08-0.49).
The retrospective chart review looked at rates of cervical cancer screening and HPV vaccination across 943 patient charts, beginning in 2006 when the HPV vaccine was released and ending in 2010. The inclusion criteria ensured that “participants were old enough to obtain cervical cancer screening and young enough to receive the HPV vaccine,” Dr. Terk and his collaborators wrote in the research abstract.
The drop-off in adherence for the subgroup who received their vaccines midstudy was an isolated finding, said Dr. Terk, noting that vaccination status did not affect adherence to the recommended screening schedule for the group as a whole.
Billing data and medical records were used to track HPV vaccination status and dates of administration, as well as the dates of testing and results for cervical cancer screening. Patients were included if they were born from 1980 to 1988, if they had two or more Pap smears during the study period, and if their HPV vaccination status could be verified. Patients with an initial abnormal Pap smear or a prior loop electrosurgical excision procedure were excluded, as were patients whose HPV vaccination status could not be confirmed.
In all, 943 patient charts were included in the review; 448 patients had no documented vaccination, with further review showing that 418 of these had, in fact, not been vaccinated, while the remaining 30 had actually had at least one HPV vaccine dose during the study period. Of the 495 patients with at least one documented vaccination, 175 had at least one Pap smear done before they were vaccinated, while 320 had their HPV vaccine before any documented cervical cancer screening.
Thus, there were two patient groups: 593 “unvaccinated” patients, who had at least one cervical cancer screening before receiving the vaccine, and 350 “vaccinated” patients, who had their HPV vaccine before any documented Pap smears.
Dr. Terk and his colleagues considered a screening interval of 18 months or less appropriate, while a longer interval than that between Pap smears was considered inappropriate timing. Individual patients were considered adherent if 76%-100% of their Pap smears were appropriately timed, partially adherent if 50%-75% of their Pap smears were appropriately timed, and not adherent if less than 50% of their Pap smears were appropriately timed.
Of those receiving their vaccine midstudy, 116 (82.9%) were adherent before vaccination, while 69 (49.3%) were adherent after vaccination.
The HPV vaccine is highly effective at preventing infection with the strains of HPV that are primarily responsible for cervical cancer. At the same time, about 70% of the cervical cancer cases that occur are associated with missed screening or inappropriate screening intervals, so screening is still an important part of the strategy to prevent cervical cancers, said Dr. Terk, a 4th-year ob.gyn. resident at the University of Rochester, N.Y.
The ACOG guidelines for cervical cancer screening have shifted through the years. During the period from 2003 to 2009, annual Pap smears were recommended for women under the age of 30 years, beginning at age 21 or 3 years after first sexual intercourse. Women 30 years and older who were at low risk could have a less frequent screening interval. ACOG currently recommends Pap testing alone every 3 years for women aged 21-29 years; co-testing with a Pap test and an HPV test every 5 years in women aged 30-65 years, or a Pap test alone every 3 years.
The study had a large sample size, and adherence rates track with national data, Dr. Terk said. However, screening guidelines have shifted in recent years, and vaccinations are now happening at a much younger age, so the findings should be interpreted with some caution. Still, he said, clinicians should incorporate a strong message about the importance of cervical cancer screening in their HPV vaccination and well-woman counseling.
Dr. Terk reported having no relevant financial disclosures and reported no outside sources of funding.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT ACOG 2017
Key clinical point:
Major finding: The odds ratio for adherence after immunization compared to before was 0.19 (95% confidence interval, 0.08-0.49).
Data source: Retrospective chart review of 495 women who received at least two Pap smears during the period from 2006 to 2010.
Disclosures: The study authors reported no outside sources of funding and no conflicts of interest.
Continuing tamoxifen costs less, performs better in ER+ breast cancer
AT ACOG 2017
SAN DIEGO – Continuation of tamoxifen for an additional 5 years is a cost-effective strategy that does not increase all-cause mortality for premenopausal women with estrogen receptor–positive breast cancer, based on an analysis using sophisticated computational modeling techniques.
“For premenopausal women with an early estrogen receptor–positive breast cancer who have completed 5 years of tamoxifen as initial treatment, another 5 years of tamoxifen is preferable to ovarian ablation with an aromatase inhibitor as extended endocrine treatment,” Janice Kwon, MD, said at the annual meeting of the American College of Obstetricians and Gynecologists.
The researchers sought to answer a key clinical question: “What is the optimal endocrine strategy for premenopausal women who have completed 5 years of tamoxifen? Another 5 years of tamoxifen? An aromatase inhibitor preceded by ovarian ablation? Or no further treatment?”
Dr. Kwon and her coinvestigators used a Markov Monte Carlo simulation to project adverse events that would occur with each of the three treatments in a hypothetical cohort of 18,000 premenopausal women with estrogen receptor–positive breast cancer. They also conducted sensitivity analyses to ascertain the point at which a given treatment would become cost effective. The investigators used a time horizon of 40 years in the Monte Carlo simulation, which uses repeated random sampling of a large data set to model the probability of a variety of outcomes. The primary outcome measure used to compare the three treatment strategies was the incremental cost-effectiveness ratio (ICER).
For the no further treatment strategy, the average costs were $1,074, for an average life expectancy gain of 16.69 years. Compared with this strategy, 5 more years of tamoxifen would cost $3,550 for an average life expectancy gain of 17.31 years, yielding an ICER of $4,042. The strategy of performing a bilateral salpingo-oophorectomy (BSO), followed by 5 years of aromatase inhibitor therapy, was more costly at $14,312 and yielded a shorter life expectancy gain at an average of 17.06 years, eliminating it as a feasible strategy in the ICER analysis.
Using the Monte Carlo simulation to assess treatment-related mortality, Dr. Kwon and her colleagues found that no further treatment would result in the most deaths from breast cancer, at 7,358. For this, and each of the other two strategies, the investigators also modeled deaths from other causes and from early BSO, using the Nurses’ Health Study hazard ratios. No further treatment would result in 5,878 deaths from other causes and none from early BSO, for a total of 13,236.
Another 5 years of tamoxifen, the model showed, would result in 6,227 deaths from breast cancer, 6,330 from other causes, and none from BSO, for a total of 12,557.
The BSO–aromatase inhibitor strategy was modeled to have the fewest deaths from breast cancer (5,504) and from other causes (5,834) but would result in an additional 1,897 deaths from the early BSO. The BSO–aromatase inhibitor strategy thus resulted in a virtually identical number of deaths over a 40-year period as no treatment at all, at 13,235.
An aromatase inhibitor is frequently considered as a treatment strategy for women with estrogen receptor–positive breast cancer. However, using an aromatase inhibitor is predicated on the patient being menopausal, so ovarian ablation is recommended for patients who have, or who may have, intact ovarian function.
Nearly 3 decades’ worth of data from the Nurses’ Health Study showed an overall hazard ratio of 1.41 for premenopausal oophorectomy without hormone therapy, said Dr. Kwon of the gynecologic oncology division at the University of British Columbia, Vancouver. Increased rates of osteoporosis, stroke, and coronary heart disease contributed to the increased risk, with 80% of the excess deaths occurring within 15 years of oophorectomy. The analysis yielded a number needed to harm for the procedure of eight.
The study’s results have also been substantiated by a recent meta-analysis, said Dr. Kwon, that also saw “fewer disease-free events but more deaths with aromatase inhibitor versus tamoxifen” (Breast Cancer Res Treat. 2017;161:185-90). However, she said, the long-term outcomes of breast cancer over many decades are unknown, and the analysis did not include costs for treatment of recurrent breast cancer.
No external funding sources were reported, and Dr. Kwon reported having no relevant financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT ACOG 2017
SAN DIEGO – Continuation of tamoxifen for an additional 5 years is a cost-effective strategy that does not increase all-cause mortality for premenopausal women with estrogen receptor–positive breast cancer, based on an analysis using sophisticated computational modeling techniques.
“For premenopausal women with an early estrogen receptor–positive breast cancer who have completed 5 years of tamoxifen as initial treatment, another 5 years of tamoxifen is preferable to ovarian ablation with an aromatase inhibitor as extended endocrine treatment,” Janice Kwon, MD, said at the annual meeting of the American College of Obstetricians and Gynecologists.
The researchers sought to answer a key clinical question: “What is the optimal endocrine strategy for premenopausal women who have completed 5 years of tamoxifen? Another 5 years of tamoxifen? An aromatase inhibitor preceded by ovarian ablation? Or no further treatment?”
Dr. Kwon and her coinvestigators used a Markov Monte Carlo simulation to project adverse events that would occur with each of the three treatments in a hypothetical cohort of 18,000 premenopausal women with estrogen receptor–positive breast cancer. They also conducted sensitivity analyses to ascertain the point at which a given treatment would become cost effective. The investigators used a time horizon of 40 years in the Monte Carlo simulation, which uses repeated random sampling of a large data set to model the probability of a variety of outcomes. The primary outcome measure used to compare the three treatment strategies was the incremental cost-effectiveness ratio (ICER).
For the no further treatment strategy, the average costs were $1,074, for an average life expectancy gain of 16.69 years. Compared with this strategy, 5 more years of tamoxifen would cost $3,550 for an average life expectancy gain of 17.31 years, yielding an ICER of $4,042. The strategy of performing a bilateral salpingo-oophorectomy (BSO), followed by 5 years of aromatase inhibitor therapy, was more costly at $14,312 and yielded a shorter life expectancy gain at an average of 17.06 years, eliminating it as a feasible strategy in the ICER analysis.
Using the Monte Carlo simulation to assess treatment-related mortality, Dr. Kwon and her colleagues found that no further treatment would result in the most deaths from breast cancer, at 7,358. For this, and each of the other two strategies, the investigators also modeled deaths from other causes and from early BSO, using the Nurses’ Health Study hazard ratios. No further treatment would result in 5,878 deaths from other causes and none from early BSO, for a total of 13,236.
Another 5 years of tamoxifen, the model showed, would result in 6,227 deaths from breast cancer, 6,330 from other causes, and none from BSO, for a total of 12,557.
The BSO–aromatase inhibitor strategy was modeled to have the fewest deaths from breast cancer (5,504) and from other causes (5,834) but would result in an additional 1,897 deaths from the early BSO. The BSO–aromatase inhibitor strategy thus resulted in a virtually identical number of deaths over a 40-year period as no treatment at all, at 13,235.
An aromatase inhibitor is frequently considered as a treatment strategy for women with estrogen receptor–positive breast cancer. However, using an aromatase inhibitor is predicated on the patient being menopausal, so ovarian ablation is recommended for patients who have, or who may have, intact ovarian function.
Nearly 3 decades’ worth of data from the Nurses’ Health Study showed an overall hazard ratio of 1.41 for premenopausal oophorectomy without hormone therapy, said Dr. Kwon of the gynecologic oncology division at the University of British Columbia, Vancouver. Increased rates of osteoporosis, stroke, and coronary heart disease contributed to the increased risk, with 80% of the excess deaths occurring within 15 years of oophorectomy. The analysis yielded a number needed to harm for the procedure of eight.
The study’s results have also been substantiated by a recent meta-analysis, said Dr. Kwon, that also saw “fewer disease-free events but more deaths with aromatase inhibitor versus tamoxifen” (Breast Cancer Res Treat. 2017;161:185-90). However, she said, the long-term outcomes of breast cancer over many decades are unknown, and the analysis did not include costs for treatment of recurrent breast cancer.
No external funding sources were reported, and Dr. Kwon reported having no relevant financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT ACOG 2017
SAN DIEGO – Continuation of tamoxifen for an additional 5 years is a cost-effective strategy that does not increase all-cause mortality for premenopausal women with estrogen receptor–positive breast cancer, based on an analysis using sophisticated computational modeling techniques.
“For premenopausal women with an early estrogen receptor–positive breast cancer who have completed 5 years of tamoxifen as initial treatment, another 5 years of tamoxifen is preferable to ovarian ablation with an aromatase inhibitor as extended endocrine treatment,” Janice Kwon, MD, said at the annual meeting of the American College of Obstetricians and Gynecologists.
The researchers sought to answer a key clinical question: “What is the optimal endocrine strategy for premenopausal women who have completed 5 years of tamoxifen? Another 5 years of tamoxifen? An aromatase inhibitor preceded by ovarian ablation? Or no further treatment?”
Dr. Kwon and her coinvestigators used a Markov Monte Carlo simulation to project adverse events that would occur with each of the three treatments in a hypothetical cohort of 18,000 premenopausal women with estrogen receptor–positive breast cancer. They also conducted sensitivity analyses to ascertain the point at which a given treatment would become cost effective. The investigators used a time horizon of 40 years in the Monte Carlo simulation, which uses repeated random sampling of a large data set to model the probability of a variety of outcomes. The primary outcome measure used to compare the three treatment strategies was the incremental cost-effectiveness ratio (ICER).
For the no further treatment strategy, the average costs were $1,074, for an average life expectancy gain of 16.69 years. Compared with this strategy, 5 more years of tamoxifen would cost $3,550 for an average life expectancy gain of 17.31 years, yielding an ICER of $4,042. The strategy of performing a bilateral salpingo-oophorectomy (BSO), followed by 5 years of aromatase inhibitor therapy, was more costly at $14,312 and yielded a shorter life expectancy gain at an average of 17.06 years, eliminating it as a feasible strategy in the ICER analysis.
Using the Monte Carlo simulation to assess treatment-related mortality, Dr. Kwon and her colleagues found that no further treatment would result in the most deaths from breast cancer, at 7,358. For this, and each of the other two strategies, the investigators also modeled deaths from other causes and from early BSO, using the Nurses’ Health Study hazard ratios. No further treatment would result in 5,878 deaths from other causes and none from early BSO, for a total of 13,236.
Another 5 years of tamoxifen, the model showed, would result in 6,227 deaths from breast cancer, 6,330 from other causes, and none from BSO, for a total of 12,557.
The BSO–aromatase inhibitor strategy was modeled to have the fewest deaths from breast cancer (5,504) and from other causes (5,834) but would result in an additional 1,897 deaths from the early BSO. The BSO–aromatase inhibitor strategy thus resulted in a virtually identical number of deaths over a 40-year period as no treatment at all, at 13,235.
An aromatase inhibitor is frequently considered as a treatment strategy for women with estrogen receptor–positive breast cancer. However, using an aromatase inhibitor is predicated on the patient being menopausal, so ovarian ablation is recommended for patients who have, or who may have, intact ovarian function.
Nearly 3 decades’ worth of data from the Nurses’ Health Study showed an overall hazard ratio of 1.41 for premenopausal oophorectomy without hormone therapy, said Dr. Kwon of the gynecologic oncology division at the University of British Columbia, Vancouver. Increased rates of osteoporosis, stroke, and coronary heart disease contributed to the increased risk, with 80% of the excess deaths occurring within 15 years of oophorectomy. The analysis yielded a number needed to harm for the procedure of eight.
The study’s results have also been substantiated by a recent meta-analysis, said Dr. Kwon, that also saw “fewer disease-free events but more deaths with aromatase inhibitor versus tamoxifen” (Breast Cancer Res Treat. 2017;161:185-90). However, she said, the long-term outcomes of breast cancer over many decades are unknown, and the analysis did not include costs for treatment of recurrent breast cancer.
No external funding sources were reported, and Dr. Kwon reported having no relevant financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
Key clinical point:
Major finding: Continuation of tamoxifen for 5 more years resulted in 678 fewer deaths than did receipt of an aromatase inhibitor and oophorectomy in a hypothetical cohort of 18,000 women.
Data source: Monte Carlo simulation and sensitivity analysis of a hypothetical cohort of 18,000 premenopausal women with estrogen receptor–positive breast cancer.
Disclosures: No external funding sources were reported, and the researchers reported having no relevant financial disclosures.
Inpatient prenatal yoga found feasible for high-risk women
AT ACOG 2017
SAN DIEGO – Inpatient prenatal yoga is a feasible and acceptable intervention for high-risk women admitted to the hospital, results from a single-center study suggested.
“We know that outside of obstetrics, yoga is beneficial to stress relief, musculoskeletal pain, and sleep quality,” Veronica Demtchouk, MD, said in an interview at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. “Inpatient high-risk obstetrics patients have very limited physical activity that they feel is safe to do.”
In an effort to investigate the feasibility of establishing an inpatient prenatal yoga program, the researchers recruited 40 women with anticipated admission to the antepartum service for at least 72 hours and who received medical clearance from their primary obstetrician. One of the medical center’s nurse practitioners, who is also a certified yoga instructor, taught a 30-minute prenatal yoga session once a week in a waiting room.
“It was a large enough space; we moved away the furniture and did the yoga sessions there,” Dr. Demtchouk said.
Study participants completed a questionnaire after each yoga session and at hospital discharge, while 14 nurses completed questionnaires regarding patient care and patient satisfaction. Of the 40 patients, 16 completed one or more yoga sessions; 24 did not participate because of scheduling conflicts with ultrasound or fetal testing, change in clinical status, lack of interest on the day of the session, and delivery or discharge prior to the yoga session.
Of the 16 study participants, 8 reported a decreased level of stress, 4 reported better sleep, 4 reported applying the yoga techniques outside of class, and 3 reported decreased pain/discomfort.
“Not a single woman complained or was displeased with the yoga sessions,” Dr. Demtchouk said. “The biggest challenge was the timing of the yoga session. It was just once a week, which limited the number of women who could attend.”
Of the 14 nurses who completed questionnaires, all viewed yoga as beneficial to their patients, none found it disruptive to providing patient care, and all indicated they would recommend an inpatient prenatal yoga program to other hospitals with an antepartum service.
“I think having several sessions throughout the week is essential for having adequate patient participation,” Dr. Demtchouk added. “It’s essential to have the nurses on board with it.”
She reported having no relevant financial disclosures.
AT ACOG 2017
SAN DIEGO – Inpatient prenatal yoga is a feasible and acceptable intervention for high-risk women admitted to the hospital, results from a single-center study suggested.
“We know that outside of obstetrics, yoga is beneficial to stress relief, musculoskeletal pain, and sleep quality,” Veronica Demtchouk, MD, said in an interview at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. “Inpatient high-risk obstetrics patients have very limited physical activity that they feel is safe to do.”
In an effort to investigate the feasibility of establishing an inpatient prenatal yoga program, the researchers recruited 40 women with anticipated admission to the antepartum service for at least 72 hours and who received medical clearance from their primary obstetrician. One of the medical center’s nurse practitioners, who is also a certified yoga instructor, taught a 30-minute prenatal yoga session once a week in a waiting room.
“It was a large enough space; we moved away the furniture and did the yoga sessions there,” Dr. Demtchouk said.
Study participants completed a questionnaire after each yoga session and at hospital discharge, while 14 nurses completed questionnaires regarding patient care and patient satisfaction. Of the 40 patients, 16 completed one or more yoga sessions; 24 did not participate because of scheduling conflicts with ultrasound or fetal testing, change in clinical status, lack of interest on the day of the session, and delivery or discharge prior to the yoga session.
Of the 16 study participants, 8 reported a decreased level of stress, 4 reported better sleep, 4 reported applying the yoga techniques outside of class, and 3 reported decreased pain/discomfort.
“Not a single woman complained or was displeased with the yoga sessions,” Dr. Demtchouk said. “The biggest challenge was the timing of the yoga session. It was just once a week, which limited the number of women who could attend.”
Of the 14 nurses who completed questionnaires, all viewed yoga as beneficial to their patients, none found it disruptive to providing patient care, and all indicated they would recommend an inpatient prenatal yoga program to other hospitals with an antepartum service.
“I think having several sessions throughout the week is essential for having adequate patient participation,” Dr. Demtchouk added. “It’s essential to have the nurses on board with it.”
She reported having no relevant financial disclosures.
AT ACOG 2017
SAN DIEGO – Inpatient prenatal yoga is a feasible and acceptable intervention for high-risk women admitted to the hospital, results from a single-center study suggested.
“We know that outside of obstetrics, yoga is beneficial to stress relief, musculoskeletal pain, and sleep quality,” Veronica Demtchouk, MD, said in an interview at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. “Inpatient high-risk obstetrics patients have very limited physical activity that they feel is safe to do.”
In an effort to investigate the feasibility of establishing an inpatient prenatal yoga program, the researchers recruited 40 women with anticipated admission to the antepartum service for at least 72 hours and who received medical clearance from their primary obstetrician. One of the medical center’s nurse practitioners, who is also a certified yoga instructor, taught a 30-minute prenatal yoga session once a week in a waiting room.
“It was a large enough space; we moved away the furniture and did the yoga sessions there,” Dr. Demtchouk said.
Study participants completed a questionnaire after each yoga session and at hospital discharge, while 14 nurses completed questionnaires regarding patient care and patient satisfaction. Of the 40 patients, 16 completed one or more yoga sessions; 24 did not participate because of scheduling conflicts with ultrasound or fetal testing, change in clinical status, lack of interest on the day of the session, and delivery or discharge prior to the yoga session.
Of the 16 study participants, 8 reported a decreased level of stress, 4 reported better sleep, 4 reported applying the yoga techniques outside of class, and 3 reported decreased pain/discomfort.
“Not a single woman complained or was displeased with the yoga sessions,” Dr. Demtchouk said. “The biggest challenge was the timing of the yoga session. It was just once a week, which limited the number of women who could attend.”
Of the 14 nurses who completed questionnaires, all viewed yoga as beneficial to their patients, none found it disruptive to providing patient care, and all indicated they would recommend an inpatient prenatal yoga program to other hospitals with an antepartum service.
“I think having several sessions throughout the week is essential for having adequate patient participation,” Dr. Demtchouk added. “It’s essential to have the nurses on board with it.”
She reported having no relevant financial disclosures.
Key clinical point:
Major finding: Of the 16 study participants, 8 reported a decreased level of stress, 4 reported better sleep, 4 reported applying the yoga techniques outside of class, and 3 reported decreased pain/discomfort.
Data source: A feasibility study of 16 hospitalized high-risk pregnant women.
Disclosures: Dr. Demtchouk reported having no relevant financial disclosures.
Meconium-stained amniotic fluid linked to postcesarean SSI
SAN DIEGO – Meconium-stained amniotic fluid may increased risk of surgical site infections following a cesarean delivery, results from a large analysis showed.
Surgical site infection (SSI) occurs in 3%-9% of patients who have a cesarean delivery, and many require hospitalization or further surgery, lead study author Andrea Snyder, MD, PhD, said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. Risk factors for SSI included chorioamnionitis, obesity, preeclampsia, preterm premature rupture of membranes, nulliparity, or emergency cesarean. Current management for avoiding SSIs includes prophylactic antibiotics, antiseptic skin, and vaginal prep.
In an effort to test the hypothesis that meconium-stained fluid is an independent risk factor associated with an increased risk of postcesarean SSI, she and her associates evaluated a subset of 25,220 women from the Maternal-Fetal Medicine Units Network cesarean registry who were treated at 19 different institutions. Their mean age was 27 years, they were all attempting labor or induction of labor, were all singleton pregnancies, and all had cesarean deliveries.
Of the 25,220 patients studied, 5,883 (23%) had MSAF. The researchers found that the incidence of SSI was 11.9% among patients who had MSAF, compared with an incidence of 8.9% among patients who did not, a difference that reached statistical significance (P less than .001). After using a multivariable logistic regression model to control for confounders including chorioamnionitis, diabetes, intrauterine pressure catheter placement, tobacco use, length of labor, length of rupture, preeclampsia, and obesity, the association between MSAF and SSI persisted (odds ratio, 1.25; confidence interval, 1.12-1.39; P less than .001).
Advantages of the study, she said, include the fact that it was a large population of patients treated at multiple institutions, “so it should be very generalizable to most practices. We also controlled for many known factors associated with SSI.” Dr. Snyder acknowledged certain limitations of the study, including the fact that the data do not show causation and that there is no further information about the SSIs. “Were those associated with meconium less or more severe SSIs?” she asked. “Does the increase in risk confer an increased risk of severe infectious morbidity? Where do we go from here and what do we do with this information? At this point we don’t have any way of preventing meconium.”
A 2014 Cochrane review found that, while prophylactic antibiotics for patients with MSAF did not decrease the risk of postpartum endometriosis, it did decrease the risk of chorioamnionitis. “But would it help decrease the risk of SSIs? We have no idea,” Dr. Snyder asked. “Would continuing antibiotics after delivery help reduce wound infections? We don’t do that routinely in a C-section, but maybe that would make sense for patients that are higher risk.” She reported having no financial disclosures.
dbrunk@frontlinemedcom.com
SAN DIEGO – Meconium-stained amniotic fluid may increased risk of surgical site infections following a cesarean delivery, results from a large analysis showed.
Surgical site infection (SSI) occurs in 3%-9% of patients who have a cesarean delivery, and many require hospitalization or further surgery, lead study author Andrea Snyder, MD, PhD, said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. Risk factors for SSI included chorioamnionitis, obesity, preeclampsia, preterm premature rupture of membranes, nulliparity, or emergency cesarean. Current management for avoiding SSIs includes prophylactic antibiotics, antiseptic skin, and vaginal prep.
In an effort to test the hypothesis that meconium-stained fluid is an independent risk factor associated with an increased risk of postcesarean SSI, she and her associates evaluated a subset of 25,220 women from the Maternal-Fetal Medicine Units Network cesarean registry who were treated at 19 different institutions. Their mean age was 27 years, they were all attempting labor or induction of labor, were all singleton pregnancies, and all had cesarean deliveries.
Of the 25,220 patients studied, 5,883 (23%) had MSAF. The researchers found that the incidence of SSI was 11.9% among patients who had MSAF, compared with an incidence of 8.9% among patients who did not, a difference that reached statistical significance (P less than .001). After using a multivariable logistic regression model to control for confounders including chorioamnionitis, diabetes, intrauterine pressure catheter placement, tobacco use, length of labor, length of rupture, preeclampsia, and obesity, the association between MSAF and SSI persisted (odds ratio, 1.25; confidence interval, 1.12-1.39; P less than .001).
Advantages of the study, she said, include the fact that it was a large population of patients treated at multiple institutions, “so it should be very generalizable to most practices. We also controlled for many known factors associated with SSI.” Dr. Snyder acknowledged certain limitations of the study, including the fact that the data do not show causation and that there is no further information about the SSIs. “Were those associated with meconium less or more severe SSIs?” she asked. “Does the increase in risk confer an increased risk of severe infectious morbidity? Where do we go from here and what do we do with this information? At this point we don’t have any way of preventing meconium.”
A 2014 Cochrane review found that, while prophylactic antibiotics for patients with MSAF did not decrease the risk of postpartum endometriosis, it did decrease the risk of chorioamnionitis. “But would it help decrease the risk of SSIs? We have no idea,” Dr. Snyder asked. “Would continuing antibiotics after delivery help reduce wound infections? We don’t do that routinely in a C-section, but maybe that would make sense for patients that are higher risk.” She reported having no financial disclosures.
dbrunk@frontlinemedcom.com
SAN DIEGO – Meconium-stained amniotic fluid may increased risk of surgical site infections following a cesarean delivery, results from a large analysis showed.
Surgical site infection (SSI) occurs in 3%-9% of patients who have a cesarean delivery, and many require hospitalization or further surgery, lead study author Andrea Snyder, MD, PhD, said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. Risk factors for SSI included chorioamnionitis, obesity, preeclampsia, preterm premature rupture of membranes, nulliparity, or emergency cesarean. Current management for avoiding SSIs includes prophylactic antibiotics, antiseptic skin, and vaginal prep.
In an effort to test the hypothesis that meconium-stained fluid is an independent risk factor associated with an increased risk of postcesarean SSI, she and her associates evaluated a subset of 25,220 women from the Maternal-Fetal Medicine Units Network cesarean registry who were treated at 19 different institutions. Their mean age was 27 years, they were all attempting labor or induction of labor, were all singleton pregnancies, and all had cesarean deliveries.
Of the 25,220 patients studied, 5,883 (23%) had MSAF. The researchers found that the incidence of SSI was 11.9% among patients who had MSAF, compared with an incidence of 8.9% among patients who did not, a difference that reached statistical significance (P less than .001). After using a multivariable logistic regression model to control for confounders including chorioamnionitis, diabetes, intrauterine pressure catheter placement, tobacco use, length of labor, length of rupture, preeclampsia, and obesity, the association between MSAF and SSI persisted (odds ratio, 1.25; confidence interval, 1.12-1.39; P less than .001).
Advantages of the study, she said, include the fact that it was a large population of patients treated at multiple institutions, “so it should be very generalizable to most practices. We also controlled for many known factors associated with SSI.” Dr. Snyder acknowledged certain limitations of the study, including the fact that the data do not show causation and that there is no further information about the SSIs. “Were those associated with meconium less or more severe SSIs?” she asked. “Does the increase in risk confer an increased risk of severe infectious morbidity? Where do we go from here and what do we do with this information? At this point we don’t have any way of preventing meconium.”
A 2014 Cochrane review found that, while prophylactic antibiotics for patients with MSAF did not decrease the risk of postpartum endometriosis, it did decrease the risk of chorioamnionitis. “But would it help decrease the risk of SSIs? We have no idea,” Dr. Snyder asked. “Would continuing antibiotics after delivery help reduce wound infections? We don’t do that routinely in a C-section, but maybe that would make sense for patients that are higher risk.” She reported having no financial disclosures.
dbrunk@frontlinemedcom.com
AT ACOG 2017
Key clinical point:
Major finding: The incidence of SSI was 11.9% in patients who had meconium-stained amniotic fluid, compared with an incidence of 8.9% in patients who did not, a difference that reached statistical significance (P less than .001).
Data source: A subset analysis of 25,220 women from the Maternal-Fetal Medicine Networks Cesarean Registry who were treated at 19 different institutions.
Disclosures: Dr. Snyder reported having no financial disclosures.
Group prenatal care offers benefits for young mothers
SAN DIEGO – Young women who received group prenatal visits under the CenteringPregnancy model were significantly more likely than were women receiving traditional prenatal care to elect long-acting reversible contraceptives postpartum, results from a small study show.
CenteringPregnancy (CP) – a group prenatal care model for women with due dates around the same time – has been touted as a way to decrease the incidence of preterm deliveries, but little is known about potential additional benefits for other birth-related outcomes, lead study author
CP sessions “follow the regular prenatal visit structure but the care itself is in a group setting,” said Dr. Roussos-Ross, an ob.gyn. at the University of Florida, Gainesville. “Each session lasts an hour and a half to 2 hours. In that group session, patients receive routine prenatal care and increased knowledge of various topics in pregnancy.”
Dr. Roussos-Ross and her associates set out to compare pregnancy-related outcomes in 20 patients aged 18-21 years who received care through the CP model, with a random sample of 20 patients who received care via the traditional care model in women’s health clinics at the University of Florida Health from January to December of 2014. They found that a significantly higher proportion of women in the CP group were African American, compared with those in the control group (85% vs. 55%, respectively; P = .024). In addition, uptake of long-acting reversible contraceptives was significantly higher among the CP group, compared with the control group (32% vs. 0%; P = .0292).
“One of the centering sessions is revolved around the education of different contraceptive uses, so they get information on the different options that they have,” Dr. Roussos-Ross said.
Differences did not reach statistical significance in other birth-related outcomes, but trends favored the CP group in most of the variables studied, including higher rates of flu vaccination (50% vs. 30%; P = .196), Tdap vaccination (60% vs. 35%; P = .11), breastfeeding initiation (95% vs. 90%; P = .579), and breastfeeding at 6 weeks postpartum (42% vs. 20%; P = .2427). Some adverse outcomes were lower in the CP group, such as low birth weight (0% vs. 10%; P = .1468), and the proportion of patients who failed to appear for their postpartum visit (21% vs. 35%; P = .333).
“The CP program was not able to demonstrate an improved preterm delivery outcome in adolescent mothers,” Dr. Roussos-Ross said. “However, this small study was able to demonstrate complementary benefits of CP in adolescent mothers, including improved breastfeeding rates, immunization rates, and [long-acting reversible contraception] usage rates. Offering adolescent mothers group care allows for greater time with their provider, which in turn may lead to increased knowledge and understanding of health and pregnancy-related outcomes.”
The researchers received grant funding from the March of Dimes for start-up costs.
SAN DIEGO – Young women who received group prenatal visits under the CenteringPregnancy model were significantly more likely than were women receiving traditional prenatal care to elect long-acting reversible contraceptives postpartum, results from a small study show.
CenteringPregnancy (CP) – a group prenatal care model for women with due dates around the same time – has been touted as a way to decrease the incidence of preterm deliveries, but little is known about potential additional benefits for other birth-related outcomes, lead study author
CP sessions “follow the regular prenatal visit structure but the care itself is in a group setting,” said Dr. Roussos-Ross, an ob.gyn. at the University of Florida, Gainesville. “Each session lasts an hour and a half to 2 hours. In that group session, patients receive routine prenatal care and increased knowledge of various topics in pregnancy.”
Dr. Roussos-Ross and her associates set out to compare pregnancy-related outcomes in 20 patients aged 18-21 years who received care through the CP model, with a random sample of 20 patients who received care via the traditional care model in women’s health clinics at the University of Florida Health from January to December of 2014. They found that a significantly higher proportion of women in the CP group were African American, compared with those in the control group (85% vs. 55%, respectively; P = .024). In addition, uptake of long-acting reversible contraceptives was significantly higher among the CP group, compared with the control group (32% vs. 0%; P = .0292).
“One of the centering sessions is revolved around the education of different contraceptive uses, so they get information on the different options that they have,” Dr. Roussos-Ross said.
Differences did not reach statistical significance in other birth-related outcomes, but trends favored the CP group in most of the variables studied, including higher rates of flu vaccination (50% vs. 30%; P = .196), Tdap vaccination (60% vs. 35%; P = .11), breastfeeding initiation (95% vs. 90%; P = .579), and breastfeeding at 6 weeks postpartum (42% vs. 20%; P = .2427). Some adverse outcomes were lower in the CP group, such as low birth weight (0% vs. 10%; P = .1468), and the proportion of patients who failed to appear for their postpartum visit (21% vs. 35%; P = .333).
“The CP program was not able to demonstrate an improved preterm delivery outcome in adolescent mothers,” Dr. Roussos-Ross said. “However, this small study was able to demonstrate complementary benefits of CP in adolescent mothers, including improved breastfeeding rates, immunization rates, and [long-acting reversible contraception] usage rates. Offering adolescent mothers group care allows for greater time with their provider, which in turn may lead to increased knowledge and understanding of health and pregnancy-related outcomes.”
The researchers received grant funding from the March of Dimes for start-up costs.
SAN DIEGO – Young women who received group prenatal visits under the CenteringPregnancy model were significantly more likely than were women receiving traditional prenatal care to elect long-acting reversible contraceptives postpartum, results from a small study show.
CenteringPregnancy (CP) – a group prenatal care model for women with due dates around the same time – has been touted as a way to decrease the incidence of preterm deliveries, but little is known about potential additional benefits for other birth-related outcomes, lead study author
CP sessions “follow the regular prenatal visit structure but the care itself is in a group setting,” said Dr. Roussos-Ross, an ob.gyn. at the University of Florida, Gainesville. “Each session lasts an hour and a half to 2 hours. In that group session, patients receive routine prenatal care and increased knowledge of various topics in pregnancy.”
Dr. Roussos-Ross and her associates set out to compare pregnancy-related outcomes in 20 patients aged 18-21 years who received care through the CP model, with a random sample of 20 patients who received care via the traditional care model in women’s health clinics at the University of Florida Health from January to December of 2014. They found that a significantly higher proportion of women in the CP group were African American, compared with those in the control group (85% vs. 55%, respectively; P = .024). In addition, uptake of long-acting reversible contraceptives was significantly higher among the CP group, compared with the control group (32% vs. 0%; P = .0292).
“One of the centering sessions is revolved around the education of different contraceptive uses, so they get information on the different options that they have,” Dr. Roussos-Ross said.
Differences did not reach statistical significance in other birth-related outcomes, but trends favored the CP group in most of the variables studied, including higher rates of flu vaccination (50% vs. 30%; P = .196), Tdap vaccination (60% vs. 35%; P = .11), breastfeeding initiation (95% vs. 90%; P = .579), and breastfeeding at 6 weeks postpartum (42% vs. 20%; P = .2427). Some adverse outcomes were lower in the CP group, such as low birth weight (0% vs. 10%; P = .1468), and the proportion of patients who failed to appear for their postpartum visit (21% vs. 35%; P = .333).
“The CP program was not able to demonstrate an improved preterm delivery outcome in adolescent mothers,” Dr. Roussos-Ross said. “However, this small study was able to demonstrate complementary benefits of CP in adolescent mothers, including improved breastfeeding rates, immunization rates, and [long-acting reversible contraception] usage rates. Offering adolescent mothers group care allows for greater time with their provider, which in turn may lead to increased knowledge and understanding of health and pregnancy-related outcomes.”
The researchers received grant funding from the March of Dimes for start-up costs.
AT ACOG 2017
Key clinical point:
Major finding: Uptake of long-acting reversible contraceptives was significantly higher among the CenteringPregnancy group compared with the control group (32% vs. 0%; P = .0292).
Data source: A chart review of 20 patients aged 18-21 years who received prenatal care via the CenteringPregnancy model, compared with a random sample of 20 patients who received traditional prenatal care.
Disclosures: The researchers received grant funding from the March of Dimes for start-up costs.
Postcesarean outpatient opioid needs predicted by inpatient use
SAN DIEGO – The amount of pain medication a women requires in the hospital after a cesarean delivery was an accurate predictor of postdischarge needs, and could provide guidance to tailor home prescriptions, reducing the amount of unused opioids left after recovery, according to a new study.
Jenna Emerson, MD, and her colleagues also found that more than half of the opioid medications prescribed for home postcesarean use went untaken, and that one in five women used no opioid medication after leaving the hospital.
The prospective cohort study, one of two awarded the Donald F. Richardson Prize at the meeting, looked at how much opioid medication was used by women while they were inpatients, and also asked women to keep track of how much medication they used at home, to see if one could predict the other.
The pilot study enrolled 100 women who had a postdelivery inpatient stay of less than 8 days, who spoke English, and who had given birth to a live viable infant. The study’s statistical analysis looked for relationships not only between inpatient and outpatient use of opioids, but also between patient characteristics and level of opioid use in the hospital and at home.
A total of 76 women completed follow-up, said Dr. Emerson, who is a fourth-year ob.gyn. resident at Brown University, Providence, R.I. One patient was excluded because she was on high opioid doses for addiction treatment before delivery, and her postdelivery opioid requirements represented a clear outlier in the data.
The investigators used medical record data to determine opioid requirements as inpatients after cesarean delivery. For standardization of different strengths of opioids, use was expressed by using Mean Morphine Equivalents (MME). Baseline patient demographic characteristics and comorbidities were also obtained from medical record review.
Patients were asked to track their home opioid use for 2 weeks postdischarge, and also received a follow-up phone call at the end of their first 2 weeks at home.
Inpatient opioid use was divided into tertiles according to low (less than 40 MME), medium (41-70 MME), and high (greater than 70 MME) use. Overall, the group’s mean opioid use in the final 24 hours before discharge was 59 MME, an amount Dr. Emerson said was equivalent to about eight tablets of oxycodone/acetaminophen or 12 tablets of hydrocodone/acetaminophen.
Most patients (89%) went home with a prescription for oxycodone/acetaminophen, and the mean number of pills prescribed per patient was 35. For the original group of 100 patients, this meant that prescriptions were written for 3,150 oxycodone/acetaminophen tablets, 162 hydrocodone/acetaminophen tablets, and 139 oxycodone tablets.
Home use over the first 2 weeks postdischarge was a mean 126 MME, or the equivalent of about 17 oxycodone/acetaminophen tablets. A total of 39% of women reported they had used less than half of their opioid medication; 21% had used all or required more opioids, and 20% had used at least half of their opioids. One in five patients (20%) had not taken a single opioid tablet after discharge from the hospital, and only 2 of the 75 women were still using opioids at the time of the 2-week follow-up call, Dr. Emerson said.
This means there was a total of 1,538 tablets of unused prescription opioid medication left in the homes of the 75 women included in the final analysis, Dr. Emerson said.
When the investigators compared inpatient and outpatient opioid use, they found that 26 women (34.7%) had been in the lowest tertile of inpatient opioid use. These women also had the lowest mean MME at home, using 53 MME in the first 2 weeks post discharge. The middle tertile for inpatient use used a mean 111 MME at home, while the highest used 195 MME (analysis of variance P less than .001).
Higher outpatient opioid use was seen in patients with a history of psychiatric comorbidities (MME 172 vs. 103 for no psychiatric comorbidities; P = .046). Other factors associated with numerically higher use that did not reach statistical significance included breastfeeding status (MME 197 for no breastfeeding, 112 for breastfeeding; P = .068) and insurance status (MME 154 for public, 95 for private; P = .058).
Patients’ mean age was 30.3 years; 63% of participants were Caucasian, 5% were black, and 19% identified their ethnicity as Hispanic. Patients were about evenly divided between having public and private insurance, and most (72%) had some post-high school education. Just 5% had a prior history of drug use or abuse, and about half (49%) were having a repeat cesarean delivery. Three quarters were breastfeeding their infants.
Unused opioid prescriptions are a significant contributor to the pool of opioids available for diversion and recent work has shown that up to 23% of opioids prescribed are used for “nonmedical” purposes, Dr. Emerson said. Since cesarean deliveries are the most commonly performed major surgery in the United States, the opportunity to reduce the number of opioids available for diversion is significant, she said.
“Opioid prescription use after cesarean delivery should be tailored to patient needs,” she said, calling for larger studies to validate and expand on the findings.
Dr. Emerson reported having no outside sources of funding and no relevant financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN DIEGO – The amount of pain medication a women requires in the hospital after a cesarean delivery was an accurate predictor of postdischarge needs, and could provide guidance to tailor home prescriptions, reducing the amount of unused opioids left after recovery, according to a new study.
Jenna Emerson, MD, and her colleagues also found that more than half of the opioid medications prescribed for home postcesarean use went untaken, and that one in five women used no opioid medication after leaving the hospital.
The prospective cohort study, one of two awarded the Donald F. Richardson Prize at the meeting, looked at how much opioid medication was used by women while they were inpatients, and also asked women to keep track of how much medication they used at home, to see if one could predict the other.
The pilot study enrolled 100 women who had a postdelivery inpatient stay of less than 8 days, who spoke English, and who had given birth to a live viable infant. The study’s statistical analysis looked for relationships not only between inpatient and outpatient use of opioids, but also between patient characteristics and level of opioid use in the hospital and at home.
A total of 76 women completed follow-up, said Dr. Emerson, who is a fourth-year ob.gyn. resident at Brown University, Providence, R.I. One patient was excluded because she was on high opioid doses for addiction treatment before delivery, and her postdelivery opioid requirements represented a clear outlier in the data.
The investigators used medical record data to determine opioid requirements as inpatients after cesarean delivery. For standardization of different strengths of opioids, use was expressed by using Mean Morphine Equivalents (MME). Baseline patient demographic characteristics and comorbidities were also obtained from medical record review.
Patients were asked to track their home opioid use for 2 weeks postdischarge, and also received a follow-up phone call at the end of their first 2 weeks at home.
Inpatient opioid use was divided into tertiles according to low (less than 40 MME), medium (41-70 MME), and high (greater than 70 MME) use. Overall, the group’s mean opioid use in the final 24 hours before discharge was 59 MME, an amount Dr. Emerson said was equivalent to about eight tablets of oxycodone/acetaminophen or 12 tablets of hydrocodone/acetaminophen.
Most patients (89%) went home with a prescription for oxycodone/acetaminophen, and the mean number of pills prescribed per patient was 35. For the original group of 100 patients, this meant that prescriptions were written for 3,150 oxycodone/acetaminophen tablets, 162 hydrocodone/acetaminophen tablets, and 139 oxycodone tablets.
Home use over the first 2 weeks postdischarge was a mean 126 MME, or the equivalent of about 17 oxycodone/acetaminophen tablets. A total of 39% of women reported they had used less than half of their opioid medication; 21% had used all or required more opioids, and 20% had used at least half of their opioids. One in five patients (20%) had not taken a single opioid tablet after discharge from the hospital, and only 2 of the 75 women were still using opioids at the time of the 2-week follow-up call, Dr. Emerson said.
This means there was a total of 1,538 tablets of unused prescription opioid medication left in the homes of the 75 women included in the final analysis, Dr. Emerson said.
When the investigators compared inpatient and outpatient opioid use, they found that 26 women (34.7%) had been in the lowest tertile of inpatient opioid use. These women also had the lowest mean MME at home, using 53 MME in the first 2 weeks post discharge. The middle tertile for inpatient use used a mean 111 MME at home, while the highest used 195 MME (analysis of variance P less than .001).
Higher outpatient opioid use was seen in patients with a history of psychiatric comorbidities (MME 172 vs. 103 for no psychiatric comorbidities; P = .046). Other factors associated with numerically higher use that did not reach statistical significance included breastfeeding status (MME 197 for no breastfeeding, 112 for breastfeeding; P = .068) and insurance status (MME 154 for public, 95 for private; P = .058).
Patients’ mean age was 30.3 years; 63% of participants were Caucasian, 5% were black, and 19% identified their ethnicity as Hispanic. Patients were about evenly divided between having public and private insurance, and most (72%) had some post-high school education. Just 5% had a prior history of drug use or abuse, and about half (49%) were having a repeat cesarean delivery. Three quarters were breastfeeding their infants.
Unused opioid prescriptions are a significant contributor to the pool of opioids available for diversion and recent work has shown that up to 23% of opioids prescribed are used for “nonmedical” purposes, Dr. Emerson said. Since cesarean deliveries are the most commonly performed major surgery in the United States, the opportunity to reduce the number of opioids available for diversion is significant, she said.
“Opioid prescription use after cesarean delivery should be tailored to patient needs,” she said, calling for larger studies to validate and expand on the findings.
Dr. Emerson reported having no outside sources of funding and no relevant financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN DIEGO – The amount of pain medication a women requires in the hospital after a cesarean delivery was an accurate predictor of postdischarge needs, and could provide guidance to tailor home prescriptions, reducing the amount of unused opioids left after recovery, according to a new study.
Jenna Emerson, MD, and her colleagues also found that more than half of the opioid medications prescribed for home postcesarean use went untaken, and that one in five women used no opioid medication after leaving the hospital.
The prospective cohort study, one of two awarded the Donald F. Richardson Prize at the meeting, looked at how much opioid medication was used by women while they were inpatients, and also asked women to keep track of how much medication they used at home, to see if one could predict the other.
The pilot study enrolled 100 women who had a postdelivery inpatient stay of less than 8 days, who spoke English, and who had given birth to a live viable infant. The study’s statistical analysis looked for relationships not only between inpatient and outpatient use of opioids, but also between patient characteristics and level of opioid use in the hospital and at home.
A total of 76 women completed follow-up, said Dr. Emerson, who is a fourth-year ob.gyn. resident at Brown University, Providence, R.I. One patient was excluded because she was on high opioid doses for addiction treatment before delivery, and her postdelivery opioid requirements represented a clear outlier in the data.
The investigators used medical record data to determine opioid requirements as inpatients after cesarean delivery. For standardization of different strengths of opioids, use was expressed by using Mean Morphine Equivalents (MME). Baseline patient demographic characteristics and comorbidities were also obtained from medical record review.
Patients were asked to track their home opioid use for 2 weeks postdischarge, and also received a follow-up phone call at the end of their first 2 weeks at home.
Inpatient opioid use was divided into tertiles according to low (less than 40 MME), medium (41-70 MME), and high (greater than 70 MME) use. Overall, the group’s mean opioid use in the final 24 hours before discharge was 59 MME, an amount Dr. Emerson said was equivalent to about eight tablets of oxycodone/acetaminophen or 12 tablets of hydrocodone/acetaminophen.
Most patients (89%) went home with a prescription for oxycodone/acetaminophen, and the mean number of pills prescribed per patient was 35. For the original group of 100 patients, this meant that prescriptions were written for 3,150 oxycodone/acetaminophen tablets, 162 hydrocodone/acetaminophen tablets, and 139 oxycodone tablets.
Home use over the first 2 weeks postdischarge was a mean 126 MME, or the equivalent of about 17 oxycodone/acetaminophen tablets. A total of 39% of women reported they had used less than half of their opioid medication; 21% had used all or required more opioids, and 20% had used at least half of their opioids. One in five patients (20%) had not taken a single opioid tablet after discharge from the hospital, and only 2 of the 75 women were still using opioids at the time of the 2-week follow-up call, Dr. Emerson said.
This means there was a total of 1,538 tablets of unused prescription opioid medication left in the homes of the 75 women included in the final analysis, Dr. Emerson said.
When the investigators compared inpatient and outpatient opioid use, they found that 26 women (34.7%) had been in the lowest tertile of inpatient opioid use. These women also had the lowest mean MME at home, using 53 MME in the first 2 weeks post discharge. The middle tertile for inpatient use used a mean 111 MME at home, while the highest used 195 MME (analysis of variance P less than .001).
Higher outpatient opioid use was seen in patients with a history of psychiatric comorbidities (MME 172 vs. 103 for no psychiatric comorbidities; P = .046). Other factors associated with numerically higher use that did not reach statistical significance included breastfeeding status (MME 197 for no breastfeeding, 112 for breastfeeding; P = .068) and insurance status (MME 154 for public, 95 for private; P = .058).
Patients’ mean age was 30.3 years; 63% of participants were Caucasian, 5% were black, and 19% identified their ethnicity as Hispanic. Patients were about evenly divided between having public and private insurance, and most (72%) had some post-high school education. Just 5% had a prior history of drug use or abuse, and about half (49%) were having a repeat cesarean delivery. Three quarters were breastfeeding their infants.
Unused opioid prescriptions are a significant contributor to the pool of opioids available for diversion and recent work has shown that up to 23% of opioids prescribed are used for “nonmedical” purposes, Dr. Emerson said. Since cesarean deliveries are the most commonly performed major surgery in the United States, the opportunity to reduce the number of opioids available for diversion is significant, she said.
“Opioid prescription use after cesarean delivery should be tailored to patient needs,” she said, calling for larger studies to validate and expand on the findings.
Dr. Emerson reported having no outside sources of funding and no relevant financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT ACOG 2017
Key clinical point:
Major finding: Inpatient opioid use by tertile was highly associated with outpatient opioid use by tertile (P less than .001).
Data source: A prospective cohort study of 75 women with cesarean deliveries of live viable infants.
Disclosures: The study authors reported no outside sources of funding and no conflicts of interest.
Despite CVD risk, few internists screen for prior preeclampsia
SAN DIEGO – Women who have preeclampsia are at increased risk for later cardiovascular disease, yet internists performing well-woman exams were unlikely to have asked their patients about a history of preeclampsia, a small study showed.
Just 21 of 89 women were asked about preeclampsia during a well-woman exam, while 88 of 89 were asked about diabetes or smoking history, and all 89 were asked about hypertension (P = .0002 for comparing preeclampsia to each individual comorbidity).
“There is a screening gap leading to missed opportunities to identify women at risk for cardiovascular disease,” Irene Lewnard, MD, said at the annual meeting of the American College of Obstetricians and Gynecologists.
Dr. Lewnard and her colleagues at the Medical College of Wisconsin, Milwaukee, used a retrospective chart review to see whether internal medicine physicians were asking about preeclampsia as well as traditional CVD risk factors during well-woman exams.
The researchers looked at records from 89 women, aged 18-48 years, who had at least one prior delivery to see whether they were asked about preeclampsia. The review also assessed whether physicians had asked about traditional CVD risk factors: smoking, diabetes, and hypertension.
Of the 89 patients, 6 had a confirmed prior history of preeclampsia. The demographic characteristics and obstetric histories of these patients were not significantly different from those of the larger group. The mean patient age was about 35 years, and the average gravidity was three and parity was two.
Dr. Lewnard, an ob.gyn., and her colleagues looked at charts beginning Jan. 1, 2013, and ending May 31, 2016, after both the American Heart Association (AHA) and the American College of Obstetricians and Gynecologists (ACOG) had issued guidelines that recognized the elevated CVD risk for women with a history of preeclampsia.
In 2011, the AHA issued guidelines that preeclampsia should be listed along with gestational diabetes and gestational hypertension as risk factors for CVD. The AHA called for ob.gyns. to refer patients with these conditions to primary care physicians or cardiologists for follow-up, and recommended that providers include questions about pregnancy-related CVD risk factors when taking a history.
In 2013, ACOG recommended early screening for heart disease for women with a history of preterm or recurrent preeclampsia, to include a consideration for early assessment of blood pressure, body mass index, serum lipids, and fasting blood glucose. The group also recommended counseling on modifiable lifestyle factors for these patients.
Data from several large studies support preeclampsia’s status as an independent risk factor for CVD. A 2001 Norwegian study of more than 600,000 births found that, for women who had preeclampsia and were delivered at term, the relative risk for death from cardiovascular disease was 1.65. However, when women with preeclampsia gave birth before 37 weeks’ gestation, the relative risk for later death from CVD rose to 8.12 (BMJ. 2001;323[7323]:1213-7).
A 2007 systematic review and meta-analysis examined data from 3,488,160 women and found a relative risk of 2.16 for ischemic heart disease after an average 11.7 years of follow-up (BMJ 2007;335:974). Finally, a smaller 2010 California study of 14,403 women found a hazard ratio of 2.14 for CVD-related deaths for all women with a history of preeclampsia. For women whose preeclampsia began before 34 weeks’ gestation, that hazard ratio rose to 9.54 (Hypertension. 2010;56:166-71).
When Dr. Lewnard and her colleagues spoke with the internists who had participated in their study, several raised the point that there are not clear guidelines about how to incorporate a history of preeclampsia into risk calculators or treatment recommendations. This knowledge gap, she said, should be addressed, with an ultimate goal of establishing an interdisciplinary set of guidelines for counseling and management of women with prior preeclampsia.
The investigators are assessing whether adding prompts to the electronic medical record could increase the number of primary care physicians who include preeclampsia questions in their history taking.
Dr. Lewnard and her colleagues reported having no outside sources of funding and no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN DIEGO – Women who have preeclampsia are at increased risk for later cardiovascular disease, yet internists performing well-woman exams were unlikely to have asked their patients about a history of preeclampsia, a small study showed.
Just 21 of 89 women were asked about preeclampsia during a well-woman exam, while 88 of 89 were asked about diabetes or smoking history, and all 89 were asked about hypertension (P = .0002 for comparing preeclampsia to each individual comorbidity).
“There is a screening gap leading to missed opportunities to identify women at risk for cardiovascular disease,” Irene Lewnard, MD, said at the annual meeting of the American College of Obstetricians and Gynecologists.
Dr. Lewnard and her colleagues at the Medical College of Wisconsin, Milwaukee, used a retrospective chart review to see whether internal medicine physicians were asking about preeclampsia as well as traditional CVD risk factors during well-woman exams.
The researchers looked at records from 89 women, aged 18-48 years, who had at least one prior delivery to see whether they were asked about preeclampsia. The review also assessed whether physicians had asked about traditional CVD risk factors: smoking, diabetes, and hypertension.
Of the 89 patients, 6 had a confirmed prior history of preeclampsia. The demographic characteristics and obstetric histories of these patients were not significantly different from those of the larger group. The mean patient age was about 35 years, and the average gravidity was three and parity was two.
Dr. Lewnard, an ob.gyn., and her colleagues looked at charts beginning Jan. 1, 2013, and ending May 31, 2016, after both the American Heart Association (AHA) and the American College of Obstetricians and Gynecologists (ACOG) had issued guidelines that recognized the elevated CVD risk for women with a history of preeclampsia.
In 2011, the AHA issued guidelines that preeclampsia should be listed along with gestational diabetes and gestational hypertension as risk factors for CVD. The AHA called for ob.gyns. to refer patients with these conditions to primary care physicians or cardiologists for follow-up, and recommended that providers include questions about pregnancy-related CVD risk factors when taking a history.
In 2013, ACOG recommended early screening for heart disease for women with a history of preterm or recurrent preeclampsia, to include a consideration for early assessment of blood pressure, body mass index, serum lipids, and fasting blood glucose. The group also recommended counseling on modifiable lifestyle factors for these patients.
Data from several large studies support preeclampsia’s status as an independent risk factor for CVD. A 2001 Norwegian study of more than 600,000 births found that, for women who had preeclampsia and were delivered at term, the relative risk for death from cardiovascular disease was 1.65. However, when women with preeclampsia gave birth before 37 weeks’ gestation, the relative risk for later death from CVD rose to 8.12 (BMJ. 2001;323[7323]:1213-7).
A 2007 systematic review and meta-analysis examined data from 3,488,160 women and found a relative risk of 2.16 for ischemic heart disease after an average 11.7 years of follow-up (BMJ 2007;335:974). Finally, a smaller 2010 California study of 14,403 women found a hazard ratio of 2.14 for CVD-related deaths for all women with a history of preeclampsia. For women whose preeclampsia began before 34 weeks’ gestation, that hazard ratio rose to 9.54 (Hypertension. 2010;56:166-71).
When Dr. Lewnard and her colleagues spoke with the internists who had participated in their study, several raised the point that there are not clear guidelines about how to incorporate a history of preeclampsia into risk calculators or treatment recommendations. This knowledge gap, she said, should be addressed, with an ultimate goal of establishing an interdisciplinary set of guidelines for counseling and management of women with prior preeclampsia.
The investigators are assessing whether adding prompts to the electronic medical record could increase the number of primary care physicians who include preeclampsia questions in their history taking.
Dr. Lewnard and her colleagues reported having no outside sources of funding and no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN DIEGO – Women who have preeclampsia are at increased risk for later cardiovascular disease, yet internists performing well-woman exams were unlikely to have asked their patients about a history of preeclampsia, a small study showed.
Just 21 of 89 women were asked about preeclampsia during a well-woman exam, while 88 of 89 were asked about diabetes or smoking history, and all 89 were asked about hypertension (P = .0002 for comparing preeclampsia to each individual comorbidity).
“There is a screening gap leading to missed opportunities to identify women at risk for cardiovascular disease,” Irene Lewnard, MD, said at the annual meeting of the American College of Obstetricians and Gynecologists.
Dr. Lewnard and her colleagues at the Medical College of Wisconsin, Milwaukee, used a retrospective chart review to see whether internal medicine physicians were asking about preeclampsia as well as traditional CVD risk factors during well-woman exams.
The researchers looked at records from 89 women, aged 18-48 years, who had at least one prior delivery to see whether they were asked about preeclampsia. The review also assessed whether physicians had asked about traditional CVD risk factors: smoking, diabetes, and hypertension.
Of the 89 patients, 6 had a confirmed prior history of preeclampsia. The demographic characteristics and obstetric histories of these patients were not significantly different from those of the larger group. The mean patient age was about 35 years, and the average gravidity was three and parity was two.
Dr. Lewnard, an ob.gyn., and her colleagues looked at charts beginning Jan. 1, 2013, and ending May 31, 2016, after both the American Heart Association (AHA) and the American College of Obstetricians and Gynecologists (ACOG) had issued guidelines that recognized the elevated CVD risk for women with a history of preeclampsia.
In 2011, the AHA issued guidelines that preeclampsia should be listed along with gestational diabetes and gestational hypertension as risk factors for CVD. The AHA called for ob.gyns. to refer patients with these conditions to primary care physicians or cardiologists for follow-up, and recommended that providers include questions about pregnancy-related CVD risk factors when taking a history.
In 2013, ACOG recommended early screening for heart disease for women with a history of preterm or recurrent preeclampsia, to include a consideration for early assessment of blood pressure, body mass index, serum lipids, and fasting blood glucose. The group also recommended counseling on modifiable lifestyle factors for these patients.
Data from several large studies support preeclampsia’s status as an independent risk factor for CVD. A 2001 Norwegian study of more than 600,000 births found that, for women who had preeclampsia and were delivered at term, the relative risk for death from cardiovascular disease was 1.65. However, when women with preeclampsia gave birth before 37 weeks’ gestation, the relative risk for later death from CVD rose to 8.12 (BMJ. 2001;323[7323]:1213-7).
A 2007 systematic review and meta-analysis examined data from 3,488,160 women and found a relative risk of 2.16 for ischemic heart disease after an average 11.7 years of follow-up (BMJ 2007;335:974). Finally, a smaller 2010 California study of 14,403 women found a hazard ratio of 2.14 for CVD-related deaths for all women with a history of preeclampsia. For women whose preeclampsia began before 34 weeks’ gestation, that hazard ratio rose to 9.54 (Hypertension. 2010;56:166-71).
When Dr. Lewnard and her colleagues spoke with the internists who had participated in their study, several raised the point that there are not clear guidelines about how to incorporate a history of preeclampsia into risk calculators or treatment recommendations. This knowledge gap, she said, should be addressed, with an ultimate goal of establishing an interdisciplinary set of guidelines for counseling and management of women with prior preeclampsia.
The investigators are assessing whether adding prompts to the electronic medical record could increase the number of primary care physicians who include preeclampsia questions in their history taking.
Dr. Lewnard and her colleagues reported having no outside sources of funding and no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT ACOG 2017
Key clinical point:
Major finding: Of 89 women who received well-woman exams, 21 were asked about prior preeclampsia, while 88 were asked about diabetes and smoking, and 89, about hypertension (P = .0002).
Data source: A retrospective record review of 89 women receiving well-woman exams in the year after the American College of Obstetricians and Gynecologists issued CVD screening guidelines for prior preeclampsia.
Disclosures: The study authors reported having no outside sources of funding and no conflicts of interest.