User login
American College of Physicians (ACP): Internal Medicine 2014
E&M codes could soon require more rigor
ORLANDO – With Medicare seeing a sharp spike in payments for evaluation and management services, a proposed overhaul of Current Procedural Terminology E&M codes could force physicians to provide substantially more documentation of their medical decision making.
The American Medical Association’s CPT editorial panel is scheduled to vote in mid-May on a recommendation to make such changes to E&M codes.
If the CPT panel’s changes are substantial enough, it’s even possible that the Centers for Medicare and Medicaid Services may embark on a revaluation of all the E&M codes, said Dr. Glenn Littenberg, a past member of the CPT editorial panel and a current CPT adviser to the American Society for Gastrointestinal Endoscopy.
If CMS decided to do so, revaluation potentially could be a good thing – if it results in a higher valuation for decision making, said Dr. Robert Wergin, president-elect of the American Academy of Family Physicians. But "if the motivation is to put up a barrier to code appropriately for the level of complexity of visits, it’s another step to undervalue the cognitive area," he said.
The federal government has been taking a closer look at coding, with the concern that electronic health records are making it easier to upcode.
A report in 2012 by the U.S. Department of Health & Human Services (HHS) inspector general found that between 2001 and 2010, physicians had increased their billing for higher-level E&M codes. Medicare payments for E&M services increased by 48% during the same period, from $22.7 billion to $33.5 billion. The Office of Inspector General labeled E&M services as "vulnerable to fraud and abuse."
Coding is a physician’s lifeblood, said Dr. Wergin. The AAFP is waiting to get more details on the CPT panel’s recommendations before it can say whether it supports the changes, he said.
The American College of Physicians said its officials could not comment, citing confidentiality agreements for ACP members who are on the CPT panel.
Detail your decision making
According to Dr. Littenberg, the CPT panel is proposing much more detailed documentation of decision making, including describing the number and complexity of problems. Medical decision making will be one of the two requirements to qualify for moderate to extensive E&M services for an office visit, an established patient, or follow-up hospital care.
The proposal is more prescriptive than current requirements, "and harder to grasp and keep in mind during an encounter," said Dr. Littenberg, who is also a gastroenterologist in Pasadena, Calif. He said he is "concerned about the impact of this," adding, "there are things about this proposal I don’t like, and I’ve said as much at CPT."
Decision making "is critical at arriving at a diagnosis and treatment plan," Dr. Wergin said, but the AAFP believes that it needs to be better defined by the CPT. "Let’s define medical decision making in a more meaningful way that makes sense to people like me," said Dr. Wergin, who added, "I have a lot of complicated patients."
If the focus is only on the presenting problem, it tends to undervalue the decision making that goes into evaluating a patient who may have multiple comorbidities and perhaps social issues as well, Dr. Wergin explained. To truly evaluate a patient, decision making should look at that individual as a whole, not as one issue, he said.
It appears that the panel is moving in that direction, Dr. Littenberg observed, but it will also require clear documentation that "reflects our thought process."
Note the basics
Physicians should be thinking more in terms of what would be required in documentation to defend an audit, he cautioned. The history, physical, and what led to decisions about diagnosis and treatment – the basic thinking behind what happened on that particular day – need to be within the notes.
That kind of documentation "is actually not that complicated, and yet we fail to do it a large percentage of the time," said Dr. Littenberg.
"It can’t just be a recap of a problem list and continue the same therapy and ‘See you next year,’ " he said. "That’s not ever going to pass a high-level audit."
On Twitter @aliciaault
ORLANDO – With Medicare seeing a sharp spike in payments for evaluation and management services, a proposed overhaul of Current Procedural Terminology E&M codes could force physicians to provide substantially more documentation of their medical decision making.
The American Medical Association’s CPT editorial panel is scheduled to vote in mid-May on a recommendation to make such changes to E&M codes.
If the CPT panel’s changes are substantial enough, it’s even possible that the Centers for Medicare and Medicaid Services may embark on a revaluation of all the E&M codes, said Dr. Glenn Littenberg, a past member of the CPT editorial panel and a current CPT adviser to the American Society for Gastrointestinal Endoscopy.
If CMS decided to do so, revaluation potentially could be a good thing – if it results in a higher valuation for decision making, said Dr. Robert Wergin, president-elect of the American Academy of Family Physicians. But "if the motivation is to put up a barrier to code appropriately for the level of complexity of visits, it’s another step to undervalue the cognitive area," he said.
The federal government has been taking a closer look at coding, with the concern that electronic health records are making it easier to upcode.
A report in 2012 by the U.S. Department of Health & Human Services (HHS) inspector general found that between 2001 and 2010, physicians had increased their billing for higher-level E&M codes. Medicare payments for E&M services increased by 48% during the same period, from $22.7 billion to $33.5 billion. The Office of Inspector General labeled E&M services as "vulnerable to fraud and abuse."
Coding is a physician’s lifeblood, said Dr. Wergin. The AAFP is waiting to get more details on the CPT panel’s recommendations before it can say whether it supports the changes, he said.
The American College of Physicians said its officials could not comment, citing confidentiality agreements for ACP members who are on the CPT panel.
Detail your decision making
According to Dr. Littenberg, the CPT panel is proposing much more detailed documentation of decision making, including describing the number and complexity of problems. Medical decision making will be one of the two requirements to qualify for moderate to extensive E&M services for an office visit, an established patient, or follow-up hospital care.
The proposal is more prescriptive than current requirements, "and harder to grasp and keep in mind during an encounter," said Dr. Littenberg, who is also a gastroenterologist in Pasadena, Calif. He said he is "concerned about the impact of this," adding, "there are things about this proposal I don’t like, and I’ve said as much at CPT."
Decision making "is critical at arriving at a diagnosis and treatment plan," Dr. Wergin said, but the AAFP believes that it needs to be better defined by the CPT. "Let’s define medical decision making in a more meaningful way that makes sense to people like me," said Dr. Wergin, who added, "I have a lot of complicated patients."
If the focus is only on the presenting problem, it tends to undervalue the decision making that goes into evaluating a patient who may have multiple comorbidities and perhaps social issues as well, Dr. Wergin explained. To truly evaluate a patient, decision making should look at that individual as a whole, not as one issue, he said.
It appears that the panel is moving in that direction, Dr. Littenberg observed, but it will also require clear documentation that "reflects our thought process."
Note the basics
Physicians should be thinking more in terms of what would be required in documentation to defend an audit, he cautioned. The history, physical, and what led to decisions about diagnosis and treatment – the basic thinking behind what happened on that particular day – need to be within the notes.
That kind of documentation "is actually not that complicated, and yet we fail to do it a large percentage of the time," said Dr. Littenberg.
"It can’t just be a recap of a problem list and continue the same therapy and ‘See you next year,’ " he said. "That’s not ever going to pass a high-level audit."
On Twitter @aliciaault
ORLANDO – With Medicare seeing a sharp spike in payments for evaluation and management services, a proposed overhaul of Current Procedural Terminology E&M codes could force physicians to provide substantially more documentation of their medical decision making.
The American Medical Association’s CPT editorial panel is scheduled to vote in mid-May on a recommendation to make such changes to E&M codes.
If the CPT panel’s changes are substantial enough, it’s even possible that the Centers for Medicare and Medicaid Services may embark on a revaluation of all the E&M codes, said Dr. Glenn Littenberg, a past member of the CPT editorial panel and a current CPT adviser to the American Society for Gastrointestinal Endoscopy.
If CMS decided to do so, revaluation potentially could be a good thing – if it results in a higher valuation for decision making, said Dr. Robert Wergin, president-elect of the American Academy of Family Physicians. But "if the motivation is to put up a barrier to code appropriately for the level of complexity of visits, it’s another step to undervalue the cognitive area," he said.
The federal government has been taking a closer look at coding, with the concern that electronic health records are making it easier to upcode.
A report in 2012 by the U.S. Department of Health & Human Services (HHS) inspector general found that between 2001 and 2010, physicians had increased their billing for higher-level E&M codes. Medicare payments for E&M services increased by 48% during the same period, from $22.7 billion to $33.5 billion. The Office of Inspector General labeled E&M services as "vulnerable to fraud and abuse."
Coding is a physician’s lifeblood, said Dr. Wergin. The AAFP is waiting to get more details on the CPT panel’s recommendations before it can say whether it supports the changes, he said.
The American College of Physicians said its officials could not comment, citing confidentiality agreements for ACP members who are on the CPT panel.
Detail your decision making
According to Dr. Littenberg, the CPT panel is proposing much more detailed documentation of decision making, including describing the number and complexity of problems. Medical decision making will be one of the two requirements to qualify for moderate to extensive E&M services for an office visit, an established patient, or follow-up hospital care.
The proposal is more prescriptive than current requirements, "and harder to grasp and keep in mind during an encounter," said Dr. Littenberg, who is also a gastroenterologist in Pasadena, Calif. He said he is "concerned about the impact of this," adding, "there are things about this proposal I don’t like, and I’ve said as much at CPT."
Decision making "is critical at arriving at a diagnosis and treatment plan," Dr. Wergin said, but the AAFP believes that it needs to be better defined by the CPT. "Let’s define medical decision making in a more meaningful way that makes sense to people like me," said Dr. Wergin, who added, "I have a lot of complicated patients."
If the focus is only on the presenting problem, it tends to undervalue the decision making that goes into evaluating a patient who may have multiple comorbidities and perhaps social issues as well, Dr. Wergin explained. To truly evaluate a patient, decision making should look at that individual as a whole, not as one issue, he said.
It appears that the panel is moving in that direction, Dr. Littenberg observed, but it will also require clear documentation that "reflects our thought process."
Note the basics
Physicians should be thinking more in terms of what would be required in documentation to defend an audit, he cautioned. The history, physical, and what led to decisions about diagnosis and treatment – the basic thinking behind what happened on that particular day – need to be within the notes.
That kind of documentation "is actually not that complicated, and yet we fail to do it a large percentage of the time," said Dr. Littenberg.
"It can’t just be a recap of a problem list and continue the same therapy and ‘See you next year,’ " he said. "That’s not ever going to pass a high-level audit."
On Twitter @aliciaault
AT ACP INTERNAL MEDICINE 2014
ABIM will add nonphysicians to certification boards
ORLANDO – The American Board of Internal Medicine is taking a potentially controversial step into the future by adding nonphysicians to both its main board and its subspecialty boards, a move that would give them a say in what defines being a good doctor.
The ABIM began the change in its governance process about 3 years ago, and took the first steps last July when it broke up its 29-member board of directors into two smaller panels: the board of directors and the ABIM council. The board will focus on governance issues, and the council will hone in on the assessment process itself. A few weeks ago, the board approved the addition of two new "public" members, including a health care executive and an official with a consumer organization.
*The subspecialty boards will remain the same, but add non-physician members. The boards will create exam committees, but those will be made up entirely of physicians.
Why the new structure?
One of the ABIM’s core roles is "to offer a professionally sanctioned definition of what a good doctor is," said Dr. Richard J. Baron, president and chief executive officer of the ABIM, in an interview. Physicians have always defined what that means, he said. But the world has changed, and "the definition doesn’t just belong to doctors," said Dr. Baron, who is also a past chair of the ABIM board.
Physicians now have to answer to payers that want to reward performance and measure quality. They also have to answer to patients. "I think there’s an increasingly clear recognition that medicine is a service profession," said Dr. Baron.
"It’s hard for us to say whether we are meeting the needs of our patients if we don’t find ways to ask them if we are. That’s a pretty important evolutionary transformation in assessing how well we do what we do," he said. "Having patients around the table as we think about the standards that we generate will help us have some assurance that we’re actually doing that."
By the same token, as physicians start working more with health care teams, having a team member help define what makes a good doctor also makes sense, said Dr. Baron.
The ABIM will soon announce the names of the nonphysicians who were confirmed in April by the ABIM Board. One is a health care executive who has experience heading a Medicaid managed care company and has also been a senior official with the Department of Health & Human Services. The second is the leader of a widely respected consumer organization, said Dr. Baron.
The main board now has 12 directors, with a maximum of 15. Up to 20% of the board’s membership can be made up of noninternists.
The council has up to 18 members, and will:
• Determine the requirements for certification and maintenance of certification across all the internal medicine disciplines.
• Harmonize ABIM standards with those of other recognized physician education and assessment initiatives.
• Set and integrate operational policies and procedures across the specialty boards.
• Evaluate proposals for new specialties/focused practice areas.
Some subspecialty board members migrated to the council. And the council has some at-large members who have expertise in performance improvement, quality measures, or health information technology. The council also will add members who can offer the patient and caregiver perspective and the health care team perspective.
Overhaul of subspecialty boards
The ABIM also decided it was time to reorganize the subspecialty boards, in part so they could more effectively design quality improvement and performance assessment modules for the MOC (maintenance of certification) process.
The role of the subspecialty boards is to define, refine, and set standards in certification and MOC in the discipline; perform oversight/review of performance assessments in the discipline; and build partnerships with societies and other organizational stakeholders in support of ABIM work.
In the past, the subspecialty boards were mainly charged with developing the exam for each specialty. But as the certification and MOC processes have evolved, the subspecialty board members have not been equipped to flesh out the exam, said Dr. Baron.
Each new exam committee will have from six to eight members, with physicians from the particular specialty. But the committees also will have at least one community physician in nonacademic practice and two public, nonphysician members. This will include, for example, a nurse practitioner who’s part of a patient-centered medical home, or a diabetes educator. And it also will include someone who can give the patient or caregiver perspective, said Dr. Baron.
The ABIM has selected exam committee members for internal medicine, critical care medicine, endocrinology, diabetes and metabolism, gastroenterology, geriatric medicine, hematology, infectious disease, medical oncology, nephrology, pulmonary disease, and rheumatology. Members of the committees will be announced in July.
The cardiology committee will contain a handful of tertiary specialties, including adult congenital heart disease, advanced heart failure and transplant cardiology, cardiovascular disease, clinical cardiac electrophysiology, and interventional cardiology.
Other specialties will be addressed in the near future.
Acceptance slow
So far, the ABIM’s governance and structural shifts seem to have largely gone unnoticed by internists, said Dr. Baron. In part, it’s because governance is a bit of sausage making that may not be of interest to outsiders. But it’s also because of the understandable focus on the changes to the MOC process, he observed.
And, the changes to the ABIM board and its subspecialty boards aren’t likely to have an impact on certification or recertification exams in the near future, Dr. Baron said.
But it will have an impact. And the addition of nonphysicians may not be wholly embraced.
Dr. Baron recalled that while giving a talk about the governance changes at the American College of Cardiology’s annual meeting in March, an ACC physician member stood up and said that he could not imagine why the ABIM thought it made sense to have a patient on the board.
"[He] congratulated me with great sarcasm on my political correctness," Dr. Baron said. " ‘What do [patients] know about being a cardiologist?’ " the physician asked.
This is "a view that many members of our physician community have," Dr. Baron noted, but he believes others will see the merits of bringing in other stakeholders.
On Twitter @aliciaault
*Correction 4/24/14: A previous version of this story misstated that the ABIM would rename the subspecialty boards. The story has been updated.
Thirty years ago, passing a board examination in internal medicine or one of its subspecialties was a rite of passage. The successful examinee had proven that they had mastered the complexities of their chosen medical discipline. One understood that there was more to clinical practice than medical knowledge, but the public demonstration of sufficient medical knowledge was a core requisite of that practice.
As a profession, we grudgingly accepted first recertification, and then the mysterious Maintenance of Certification process, as proof of our continued intellectual competency. We assented without much complaint to the increased costs and the constantly changing specifics of the certification process.
Now we learn that others, such as community physicians, health care executives, and consumer advocates, will have a place on the ABIM to pass judgment on the professional, knowledge-based, assessment of experts in internal medicine and its subspecialties. Instead of just "taking our boards," it may well be time to speak up and take them back!
Thirty years ago, passing a board examination in internal medicine or one of its subspecialties was a rite of passage. The successful examinee had proven that they had mastered the complexities of their chosen medical discipline. One understood that there was more to clinical practice than medical knowledge, but the public demonstration of sufficient medical knowledge was a core requisite of that practice.
As a profession, we grudgingly accepted first recertification, and then the mysterious Maintenance of Certification process, as proof of our continued intellectual competency. We assented without much complaint to the increased costs and the constantly changing specifics of the certification process.
Now we learn that others, such as community physicians, health care executives, and consumer advocates, will have a place on the ABIM to pass judgment on the professional, knowledge-based, assessment of experts in internal medicine and its subspecialties. Instead of just "taking our boards," it may well be time to speak up and take them back!
Thirty years ago, passing a board examination in internal medicine or one of its subspecialties was a rite of passage. The successful examinee had proven that they had mastered the complexities of their chosen medical discipline. One understood that there was more to clinical practice than medical knowledge, but the public demonstration of sufficient medical knowledge was a core requisite of that practice.
As a profession, we grudgingly accepted first recertification, and then the mysterious Maintenance of Certification process, as proof of our continued intellectual competency. We assented without much complaint to the increased costs and the constantly changing specifics of the certification process.
Now we learn that others, such as community physicians, health care executives, and consumer advocates, will have a place on the ABIM to pass judgment on the professional, knowledge-based, assessment of experts in internal medicine and its subspecialties. Instead of just "taking our boards," it may well be time to speak up and take them back!
ORLANDO – The American Board of Internal Medicine is taking a potentially controversial step into the future by adding nonphysicians to both its main board and its subspecialty boards, a move that would give them a say in what defines being a good doctor.
The ABIM began the change in its governance process about 3 years ago, and took the first steps last July when it broke up its 29-member board of directors into two smaller panels: the board of directors and the ABIM council. The board will focus on governance issues, and the council will hone in on the assessment process itself. A few weeks ago, the board approved the addition of two new "public" members, including a health care executive and an official with a consumer organization.
*The subspecialty boards will remain the same, but add non-physician members. The boards will create exam committees, but those will be made up entirely of physicians.
Why the new structure?
One of the ABIM’s core roles is "to offer a professionally sanctioned definition of what a good doctor is," said Dr. Richard J. Baron, president and chief executive officer of the ABIM, in an interview. Physicians have always defined what that means, he said. But the world has changed, and "the definition doesn’t just belong to doctors," said Dr. Baron, who is also a past chair of the ABIM board.
Physicians now have to answer to payers that want to reward performance and measure quality. They also have to answer to patients. "I think there’s an increasingly clear recognition that medicine is a service profession," said Dr. Baron.
"It’s hard for us to say whether we are meeting the needs of our patients if we don’t find ways to ask them if we are. That’s a pretty important evolutionary transformation in assessing how well we do what we do," he said. "Having patients around the table as we think about the standards that we generate will help us have some assurance that we’re actually doing that."
By the same token, as physicians start working more with health care teams, having a team member help define what makes a good doctor also makes sense, said Dr. Baron.
The ABIM will soon announce the names of the nonphysicians who were confirmed in April by the ABIM Board. One is a health care executive who has experience heading a Medicaid managed care company and has also been a senior official with the Department of Health & Human Services. The second is the leader of a widely respected consumer organization, said Dr. Baron.
The main board now has 12 directors, with a maximum of 15. Up to 20% of the board’s membership can be made up of noninternists.
The council has up to 18 members, and will:
• Determine the requirements for certification and maintenance of certification across all the internal medicine disciplines.
• Harmonize ABIM standards with those of other recognized physician education and assessment initiatives.
• Set and integrate operational policies and procedures across the specialty boards.
• Evaluate proposals for new specialties/focused practice areas.
Some subspecialty board members migrated to the council. And the council has some at-large members who have expertise in performance improvement, quality measures, or health information technology. The council also will add members who can offer the patient and caregiver perspective and the health care team perspective.
Overhaul of subspecialty boards
The ABIM also decided it was time to reorganize the subspecialty boards, in part so they could more effectively design quality improvement and performance assessment modules for the MOC (maintenance of certification) process.
The role of the subspecialty boards is to define, refine, and set standards in certification and MOC in the discipline; perform oversight/review of performance assessments in the discipline; and build partnerships with societies and other organizational stakeholders in support of ABIM work.
In the past, the subspecialty boards were mainly charged with developing the exam for each specialty. But as the certification and MOC processes have evolved, the subspecialty board members have not been equipped to flesh out the exam, said Dr. Baron.
Each new exam committee will have from six to eight members, with physicians from the particular specialty. But the committees also will have at least one community physician in nonacademic practice and two public, nonphysician members. This will include, for example, a nurse practitioner who’s part of a patient-centered medical home, or a diabetes educator. And it also will include someone who can give the patient or caregiver perspective, said Dr. Baron.
The ABIM has selected exam committee members for internal medicine, critical care medicine, endocrinology, diabetes and metabolism, gastroenterology, geriatric medicine, hematology, infectious disease, medical oncology, nephrology, pulmonary disease, and rheumatology. Members of the committees will be announced in July.
The cardiology committee will contain a handful of tertiary specialties, including adult congenital heart disease, advanced heart failure and transplant cardiology, cardiovascular disease, clinical cardiac electrophysiology, and interventional cardiology.
Other specialties will be addressed in the near future.
Acceptance slow
So far, the ABIM’s governance and structural shifts seem to have largely gone unnoticed by internists, said Dr. Baron. In part, it’s because governance is a bit of sausage making that may not be of interest to outsiders. But it’s also because of the understandable focus on the changes to the MOC process, he observed.
And, the changes to the ABIM board and its subspecialty boards aren’t likely to have an impact on certification or recertification exams in the near future, Dr. Baron said.
But it will have an impact. And the addition of nonphysicians may not be wholly embraced.
Dr. Baron recalled that while giving a talk about the governance changes at the American College of Cardiology’s annual meeting in March, an ACC physician member stood up and said that he could not imagine why the ABIM thought it made sense to have a patient on the board.
"[He] congratulated me with great sarcasm on my political correctness," Dr. Baron said. " ‘What do [patients] know about being a cardiologist?’ " the physician asked.
This is "a view that many members of our physician community have," Dr. Baron noted, but he believes others will see the merits of bringing in other stakeholders.
On Twitter @aliciaault
*Correction 4/24/14: A previous version of this story misstated that the ABIM would rename the subspecialty boards. The story has been updated.
ORLANDO – The American Board of Internal Medicine is taking a potentially controversial step into the future by adding nonphysicians to both its main board and its subspecialty boards, a move that would give them a say in what defines being a good doctor.
The ABIM began the change in its governance process about 3 years ago, and took the first steps last July when it broke up its 29-member board of directors into two smaller panels: the board of directors and the ABIM council. The board will focus on governance issues, and the council will hone in on the assessment process itself. A few weeks ago, the board approved the addition of two new "public" members, including a health care executive and an official with a consumer organization.
*The subspecialty boards will remain the same, but add non-physician members. The boards will create exam committees, but those will be made up entirely of physicians.
Why the new structure?
One of the ABIM’s core roles is "to offer a professionally sanctioned definition of what a good doctor is," said Dr. Richard J. Baron, president and chief executive officer of the ABIM, in an interview. Physicians have always defined what that means, he said. But the world has changed, and "the definition doesn’t just belong to doctors," said Dr. Baron, who is also a past chair of the ABIM board.
Physicians now have to answer to payers that want to reward performance and measure quality. They also have to answer to patients. "I think there’s an increasingly clear recognition that medicine is a service profession," said Dr. Baron.
"It’s hard for us to say whether we are meeting the needs of our patients if we don’t find ways to ask them if we are. That’s a pretty important evolutionary transformation in assessing how well we do what we do," he said. "Having patients around the table as we think about the standards that we generate will help us have some assurance that we’re actually doing that."
By the same token, as physicians start working more with health care teams, having a team member help define what makes a good doctor also makes sense, said Dr. Baron.
The ABIM will soon announce the names of the nonphysicians who were confirmed in April by the ABIM Board. One is a health care executive who has experience heading a Medicaid managed care company and has also been a senior official with the Department of Health & Human Services. The second is the leader of a widely respected consumer organization, said Dr. Baron.
The main board now has 12 directors, with a maximum of 15. Up to 20% of the board’s membership can be made up of noninternists.
The council has up to 18 members, and will:
• Determine the requirements for certification and maintenance of certification across all the internal medicine disciplines.
• Harmonize ABIM standards with those of other recognized physician education and assessment initiatives.
• Set and integrate operational policies and procedures across the specialty boards.
• Evaluate proposals for new specialties/focused practice areas.
Some subspecialty board members migrated to the council. And the council has some at-large members who have expertise in performance improvement, quality measures, or health information technology. The council also will add members who can offer the patient and caregiver perspective and the health care team perspective.
Overhaul of subspecialty boards
The ABIM also decided it was time to reorganize the subspecialty boards, in part so they could more effectively design quality improvement and performance assessment modules for the MOC (maintenance of certification) process.
The role of the subspecialty boards is to define, refine, and set standards in certification and MOC in the discipline; perform oversight/review of performance assessments in the discipline; and build partnerships with societies and other organizational stakeholders in support of ABIM work.
In the past, the subspecialty boards were mainly charged with developing the exam for each specialty. But as the certification and MOC processes have evolved, the subspecialty board members have not been equipped to flesh out the exam, said Dr. Baron.
Each new exam committee will have from six to eight members, with physicians from the particular specialty. But the committees also will have at least one community physician in nonacademic practice and two public, nonphysician members. This will include, for example, a nurse practitioner who’s part of a patient-centered medical home, or a diabetes educator. And it also will include someone who can give the patient or caregiver perspective, said Dr. Baron.
The ABIM has selected exam committee members for internal medicine, critical care medicine, endocrinology, diabetes and metabolism, gastroenterology, geriatric medicine, hematology, infectious disease, medical oncology, nephrology, pulmonary disease, and rheumatology. Members of the committees will be announced in July.
The cardiology committee will contain a handful of tertiary specialties, including adult congenital heart disease, advanced heart failure and transplant cardiology, cardiovascular disease, clinical cardiac electrophysiology, and interventional cardiology.
Other specialties will be addressed in the near future.
Acceptance slow
So far, the ABIM’s governance and structural shifts seem to have largely gone unnoticed by internists, said Dr. Baron. In part, it’s because governance is a bit of sausage making that may not be of interest to outsiders. But it’s also because of the understandable focus on the changes to the MOC process, he observed.
And, the changes to the ABIM board and its subspecialty boards aren’t likely to have an impact on certification or recertification exams in the near future, Dr. Baron said.
But it will have an impact. And the addition of nonphysicians may not be wholly embraced.
Dr. Baron recalled that while giving a talk about the governance changes at the American College of Cardiology’s annual meeting in March, an ACC physician member stood up and said that he could not imagine why the ABIM thought it made sense to have a patient on the board.
"[He] congratulated me with great sarcasm on my political correctness," Dr. Baron said. " ‘What do [patients] know about being a cardiologist?’ " the physician asked.
This is "a view that many members of our physician community have," Dr. Baron noted, but he believes others will see the merits of bringing in other stakeholders.
On Twitter @aliciaault
*Correction 4/24/14: A previous version of this story misstated that the ABIM would rename the subspecialty boards. The story has been updated.
FROM ACP 2014
VIDEO: How to engage patients in their health
ORLANDO – Asking your patients about where they get their health information online is the first step toward helping them become "e-patients" – engaged patients who change their behaviors to improve their health, explains Dr. Daniel Sands.
And a willingness to answer a patient’s question with "I don’t know" can be the first step to becoming an engaged physician.
Dr. Sands has coauthored the book "Let Patients Help!" with Dave deBronkart, better known as "e-Patient Dave." He’s also the cofounder and cochair of the Society for Participatory Medicine, so he knows a thing or two about engaging patients in their health care and creating better outcomes.
In a video interview during the annual meeting of the American College of Physicians, Dr. Sands, who is with the department of medicine at Harvard Medical School in Boston, explains how physicians can use patients’ own online searches for health care answers to better involve patients in their health, and how physicians can work together with patients via technology to create a more satisfying experience in their practices.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
ORLANDO – Asking your patients about where they get their health information online is the first step toward helping them become "e-patients" – engaged patients who change their behaviors to improve their health, explains Dr. Daniel Sands.
And a willingness to answer a patient’s question with "I don’t know" can be the first step to becoming an engaged physician.
Dr. Sands has coauthored the book "Let Patients Help!" with Dave deBronkart, better known as "e-Patient Dave." He’s also the cofounder and cochair of the Society for Participatory Medicine, so he knows a thing or two about engaging patients in their health care and creating better outcomes.
In a video interview during the annual meeting of the American College of Physicians, Dr. Sands, who is with the department of medicine at Harvard Medical School in Boston, explains how physicians can use patients’ own online searches for health care answers to better involve patients in their health, and how physicians can work together with patients via technology to create a more satisfying experience in their practices.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
ORLANDO – Asking your patients about where they get their health information online is the first step toward helping them become "e-patients" – engaged patients who change their behaviors to improve their health, explains Dr. Daniel Sands.
And a willingness to answer a patient’s question with "I don’t know" can be the first step to becoming an engaged physician.
Dr. Sands has coauthored the book "Let Patients Help!" with Dave deBronkart, better known as "e-Patient Dave." He’s also the cofounder and cochair of the Society for Participatory Medicine, so he knows a thing or two about engaging patients in their health care and creating better outcomes.
In a video interview during the annual meeting of the American College of Physicians, Dr. Sands, who is with the department of medicine at Harvard Medical School in Boston, explains how physicians can use patients’ own online searches for health care answers to better involve patients in their health, and how physicians can work together with patients via technology to create a more satisfying experience in their practices.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
AT ACP INTERNAL MEDICINE 2014
VIDEO: Practice pearls for treating opiate dependence
ORLANDO — What should you do when you have a patient who is opiate dependent, but is hospitalized for an unrelated medical reason? What should you do at discharge? And how effective are the available pharmacotherapies for addiction?
Dr. Jeffrey H. Samet, chief of general internal medicine at Boston University School of Medicine, Boston, shared a few clinical pearls in this video interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
ORLANDO — What should you do when you have a patient who is opiate dependent, but is hospitalized for an unrelated medical reason? What should you do at discharge? And how effective are the available pharmacotherapies for addiction?
Dr. Jeffrey H. Samet, chief of general internal medicine at Boston University School of Medicine, Boston, shared a few clinical pearls in this video interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
ORLANDO — What should you do when you have a patient who is opiate dependent, but is hospitalized for an unrelated medical reason? What should you do at discharge? And how effective are the available pharmacotherapies for addiction?
Dr. Jeffrey H. Samet, chief of general internal medicine at Boston University School of Medicine, Boston, shared a few clinical pearls in this video interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
AT ACP INTERNAL MEDICINE 2014
VIDEO: The don'ts of social media for physicians
ORLANDO — If you’re on social media sites such as Twitter and Facebook, or considering joining one, there’s one type of post you should absolutely refrain from making.
In an interview at the American College of Physicians annual meeting, Dr. Matthew DeCamp, assistant professor at the Johns Hopkins Berman Institute of Bioethics and in the Johns Hopkins division of general internal medicine, revealed the type of post that poses greatest danger for clinicians, and outlined other tips for safely navigating social media as a physician.
On Twitter @naseemmiller
ORLANDO — If you’re on social media sites such as Twitter and Facebook, or considering joining one, there’s one type of post you should absolutely refrain from making.
In an interview at the American College of Physicians annual meeting, Dr. Matthew DeCamp, assistant professor at the Johns Hopkins Berman Institute of Bioethics and in the Johns Hopkins division of general internal medicine, revealed the type of post that poses greatest danger for clinicians, and outlined other tips for safely navigating social media as a physician.
On Twitter @naseemmiller
ORLANDO — If you’re on social media sites such as Twitter and Facebook, or considering joining one, there’s one type of post you should absolutely refrain from making.
In an interview at the American College of Physicians annual meeting, Dr. Matthew DeCamp, assistant professor at the Johns Hopkins Berman Institute of Bioethics and in the Johns Hopkins division of general internal medicine, revealed the type of post that poses greatest danger for clinicians, and outlined other tips for safely navigating social media as a physician.
On Twitter @naseemmiller
AT ACP INTERNAL MEDICINE 2014
ACP gives primary care and specialists tools for better referrals
ORLANDO – The American College of Physicians has unveiled a toolkit to improve referrals and care coordination between primary care physicians and specialists.
The High Value Care Coordination Toolkit also aims to eliminate waste and duplicative care and create more efficiency in care delivery.
The toolkit is available on the ACP’s website and was developed by the group’s Council of Subspecialty Societies and patient advocacy groups. The ACP also received input from a number of specialty societies, including the American Academy of Neurology, the American College of Cardiology, the American College of Rheumatology, the American Gastroenterological Association, the American Society of Hematology, the Endocrine Society, and the Society of Hospital Medicine.
"Physicians need specific information to do their jobs effectively," said Dr. Molly Cooke, the outgoing president of the ACP, in a statement. "The High Value Care Coordination Toolkit facilitates clear communication between primary care and subspecialist practices so that doctors can provide seamless, coordinated, and quality care to their patients."
Dr. Charles Cutler, immediate past chair of the ACP Board of Regents, said that he frequently heard from frustrated specialists who felt that referring primary care doctors had not given them enough information about the patient who was being referred.
"This is not a trivial problem, it’s something that drives both the medical subspecialists crazy and the primary care doctor like myself," said Dr. Cutler. "Because, on both sides, the information isn’t moving back and forth."
The toolkit creates a roadmap, he said. It includes five components:
• A checklist of information to include in a generic referral to a subspecialist practice.
• A checklist of information to include in a subspecialist’s response to a referral request.
• Pertinent data sets reflecting specific information – in addition to that found on a generic referral request – to include in a referral for a number of specific common conditions to help ensure an effective and high-value engagement.
• Model care coordination agreement templates between primary care and subspecialty practices, and between a primary care practice and hospital care team.
• An outline of recommendations to physicians on preparing a patient for a referral in a patient- and family-centered manner.
The data sets were developed with the medical specialty societies and can come in very useful, said Dr. Cooke, who has been using the toolkit in her practice at the University of California, San Francisco.
Dr. Carol Greenlee, vice chair of the ACP’s Council of Subspecialty Societies and an endocrinologist in Grand Junction, Colo., also said that she had been using the toolkit with physicians who were in her independent practice association (IPA).
"It’s easy when we’re integrated," said Dr. Greenlee, who helped develop the toolkit. For physicians who work outside her IPA, she said she sent letters outlining what she would like from doctors who made referrals to her. She said the vast majority responded, and now she gets great clinical questions and data on the patients who come in. And the patients come in prepared, Dr. Greenlee added.
She recommended that primary care physicians ask specialists who they work with what they’d like to see. "It doesn’t have to be a contract," she said.
Care coordination would be more crucial as health care moved to accountable care organizations and payment arrangements that were either true capitation or something similar, noted Dr. Bruce Leff, chair of the ACP’s Council of Subspecialty Societies. "There will be very strong positive incentives to be more efficient," said Dr. Leff, a geriatrician at Johns Hopkins University, Baltimore. "Efficiency is not just dollars. It’s physician time and patient time."
The documents offered in the toolkit "are really well thought–through guides," said Dr. Leff, adding that he believed that they could "save medical systems a lot of time and effort."
On Twitter @aliciaault
Dr. Molly Cooke,
ORLANDO – The American College of Physicians has unveiled a toolkit to improve referrals and care coordination between primary care physicians and specialists.
The High Value Care Coordination Toolkit also aims to eliminate waste and duplicative care and create more efficiency in care delivery.
The toolkit is available on the ACP’s website and was developed by the group’s Council of Subspecialty Societies and patient advocacy groups. The ACP also received input from a number of specialty societies, including the American Academy of Neurology, the American College of Cardiology, the American College of Rheumatology, the American Gastroenterological Association, the American Society of Hematology, the Endocrine Society, and the Society of Hospital Medicine.
"Physicians need specific information to do their jobs effectively," said Dr. Molly Cooke, the outgoing president of the ACP, in a statement. "The High Value Care Coordination Toolkit facilitates clear communication between primary care and subspecialist practices so that doctors can provide seamless, coordinated, and quality care to their patients."
Dr. Charles Cutler, immediate past chair of the ACP Board of Regents, said that he frequently heard from frustrated specialists who felt that referring primary care doctors had not given them enough information about the patient who was being referred.
"This is not a trivial problem, it’s something that drives both the medical subspecialists crazy and the primary care doctor like myself," said Dr. Cutler. "Because, on both sides, the information isn’t moving back and forth."
The toolkit creates a roadmap, he said. It includes five components:
• A checklist of information to include in a generic referral to a subspecialist practice.
• A checklist of information to include in a subspecialist’s response to a referral request.
• Pertinent data sets reflecting specific information – in addition to that found on a generic referral request – to include in a referral for a number of specific common conditions to help ensure an effective and high-value engagement.
• Model care coordination agreement templates between primary care and subspecialty practices, and between a primary care practice and hospital care team.
• An outline of recommendations to physicians on preparing a patient for a referral in a patient- and family-centered manner.
The data sets were developed with the medical specialty societies and can come in very useful, said Dr. Cooke, who has been using the toolkit in her practice at the University of California, San Francisco.
Dr. Carol Greenlee, vice chair of the ACP’s Council of Subspecialty Societies and an endocrinologist in Grand Junction, Colo., also said that she had been using the toolkit with physicians who were in her independent practice association (IPA).
"It’s easy when we’re integrated," said Dr. Greenlee, who helped develop the toolkit. For physicians who work outside her IPA, she said she sent letters outlining what she would like from doctors who made referrals to her. She said the vast majority responded, and now she gets great clinical questions and data on the patients who come in. And the patients come in prepared, Dr. Greenlee added.
She recommended that primary care physicians ask specialists who they work with what they’d like to see. "It doesn’t have to be a contract," she said.
Care coordination would be more crucial as health care moved to accountable care organizations and payment arrangements that were either true capitation or something similar, noted Dr. Bruce Leff, chair of the ACP’s Council of Subspecialty Societies. "There will be very strong positive incentives to be more efficient," said Dr. Leff, a geriatrician at Johns Hopkins University, Baltimore. "Efficiency is not just dollars. It’s physician time and patient time."
The documents offered in the toolkit "are really well thought–through guides," said Dr. Leff, adding that he believed that they could "save medical systems a lot of time and effort."
On Twitter @aliciaault
ORLANDO – The American College of Physicians has unveiled a toolkit to improve referrals and care coordination between primary care physicians and specialists.
The High Value Care Coordination Toolkit also aims to eliminate waste and duplicative care and create more efficiency in care delivery.
The toolkit is available on the ACP’s website and was developed by the group’s Council of Subspecialty Societies and patient advocacy groups. The ACP also received input from a number of specialty societies, including the American Academy of Neurology, the American College of Cardiology, the American College of Rheumatology, the American Gastroenterological Association, the American Society of Hematology, the Endocrine Society, and the Society of Hospital Medicine.
"Physicians need specific information to do their jobs effectively," said Dr. Molly Cooke, the outgoing president of the ACP, in a statement. "The High Value Care Coordination Toolkit facilitates clear communication between primary care and subspecialist practices so that doctors can provide seamless, coordinated, and quality care to their patients."
Dr. Charles Cutler, immediate past chair of the ACP Board of Regents, said that he frequently heard from frustrated specialists who felt that referring primary care doctors had not given them enough information about the patient who was being referred.
"This is not a trivial problem, it’s something that drives both the medical subspecialists crazy and the primary care doctor like myself," said Dr. Cutler. "Because, on both sides, the information isn’t moving back and forth."
The toolkit creates a roadmap, he said. It includes five components:
• A checklist of information to include in a generic referral to a subspecialist practice.
• A checklist of information to include in a subspecialist’s response to a referral request.
• Pertinent data sets reflecting specific information – in addition to that found on a generic referral request – to include in a referral for a number of specific common conditions to help ensure an effective and high-value engagement.
• Model care coordination agreement templates between primary care and subspecialty practices, and between a primary care practice and hospital care team.
• An outline of recommendations to physicians on preparing a patient for a referral in a patient- and family-centered manner.
The data sets were developed with the medical specialty societies and can come in very useful, said Dr. Cooke, who has been using the toolkit in her practice at the University of California, San Francisco.
Dr. Carol Greenlee, vice chair of the ACP’s Council of Subspecialty Societies and an endocrinologist in Grand Junction, Colo., also said that she had been using the toolkit with physicians who were in her independent practice association (IPA).
"It’s easy when we’re integrated," said Dr. Greenlee, who helped develop the toolkit. For physicians who work outside her IPA, she said she sent letters outlining what she would like from doctors who made referrals to her. She said the vast majority responded, and now she gets great clinical questions and data on the patients who come in. And the patients come in prepared, Dr. Greenlee added.
She recommended that primary care physicians ask specialists who they work with what they’d like to see. "It doesn’t have to be a contract," she said.
Care coordination would be more crucial as health care moved to accountable care organizations and payment arrangements that were either true capitation or something similar, noted Dr. Bruce Leff, chair of the ACP’s Council of Subspecialty Societies. "There will be very strong positive incentives to be more efficient," said Dr. Leff, a geriatrician at Johns Hopkins University, Baltimore. "Efficiency is not just dollars. It’s physician time and patient time."
The documents offered in the toolkit "are really well thought–through guides," said Dr. Leff, adding that he believed that they could "save medical systems a lot of time and effort."
On Twitter @aliciaault
Dr. Molly Cooke,
Dr. Molly Cooke,
AT ACP INTERNAL MEDICINE 2014
VIDEO: Do you ask patients about guns in their homes?
ORLANDO – The American College of Physicians released a policy paper on April 10 calling gun violence a public health threat and asking physicians to discuss gun violence with their patients.
Physicians, however, vary in how they handle the issue, depending on where they work, or how they view the issue. In a series of onsite interviews with physicians attending the American College of Physicians annual meeting, we captured a snapshot of their own nuanced perspectives.
On Twitter @naseemmiller
ORLANDO – The American College of Physicians released a policy paper on April 10 calling gun violence a public health threat and asking physicians to discuss gun violence with their patients.
Physicians, however, vary in how they handle the issue, depending on where they work, or how they view the issue. In a series of onsite interviews with physicians attending the American College of Physicians annual meeting, we captured a snapshot of their own nuanced perspectives.
On Twitter @naseemmiller
ORLANDO – The American College of Physicians released a policy paper on April 10 calling gun violence a public health threat and asking physicians to discuss gun violence with their patients.
Physicians, however, vary in how they handle the issue, depending on where they work, or how they view the issue. In a series of onsite interviews with physicians attending the American College of Physicians annual meeting, we captured a snapshot of their own nuanced perspectives.
On Twitter @naseemmiller
AT ACP 2014
ACP: Physicians must address gun violence
ORLANDO – Gun violence is a public health threat that needs to be addressed with the best scientific evidence to help reduce injuries and deaths, a new policy from the American College of Physicians proclaims.
"Access to firearms, especially firearms in the home, increases the likelihood that a person will be a victim of gun violence by homicide or suicide," Bob Doherty, ACP senior vice president of governmental affairs and public policy, said April 10 at the annual meeting of the American College of Physicians. "The evidence is very clear – the risk is higher.
The policy, published simultaneously in Annals of Internal Medicine (2014 April 10 [doi: 10.7326/M14-0216]), calls for universal criminal background checks and favors a prohibition on assault and semiautomatic weapons and large-capacity magazines. It updates the ACP’s 1996 policy.
"As an organization representing physicians who have firsthand experience with the devastating impact of firearm-related violence, ACP has a responsibility to participate in efforts to mitigate needless tragedies," Dr. Thomas Tape, chairman of the ACP health and public policy committee, said.
The ACP sought to balance its recommendations on gun violence and mental illness, Dr. Tape said, adding that any restrictions on gun ownership should not broadly target people with mental illness. Only a small portion of those who are mentally ill may be at risk for harming themselves or others, he said.
Of the 32,000 gun-related deaths in the United States each year, 11,000 are homicides, 19,000 are suicides, and the rest are unintentional, according to evidence from the 120 studies reviewed for the policy paper.
Determining who’s at the greatest risk for harming themselves or others "clearly begs for more research," said Dr. Tape. "We need better predictors."
Dr. Molly Cooke, ACP president, agreed, and noted that 30% of patients in primary care practices have a mental health diagnosis. With a high prevalence of illness and a low proportion of those who might actually do harm, "you’d be prohibiting lots of people from owning guns who would never harm anyone," Dr. Cooke said.
Dr. Tape also said the ACP believes that "the physician’s judgment is critically important." He said that often, patients will disclose their state of mind, allowing the physician to determine whether it is appropriate to alert the authorities or offer follow-up care.
Physicians are required by law to inform authorities when they believe a patient poses an imminent threat. "But the question is whether physicians should be required to more broadly report on individuals with mental illness who may pose a threat," Dr. Tape said.
Reporting requirements should not act as a disincentive to seek care, or interfere with the patient-physician relationship, according to the policy paper.
"The ACP strongly believes the patient-physician relationship should be protected from laws that prevent physicians from initiating a discussion about guns," Dr. Cooke said.
The policy paper also voices the ACP’s support for devices such as trigger locks, as well as efforts to keep guns out of the hands of children, adolescents, people with dementia, and those with substance use disorders.
According to a 2013 survey of ACP members, the vast majority agree that firearm injury is a public health issue. Close to 90% also said they supported mandatory background checks, mandatory registration, and a ban on assault weapons (Ann. Intern. Med. 2014 April 10 [doi: 10.7326/M13-1960]).
Of the 573 respondents, 64% reported having had patients who were injured or killed by a gun, and 14% said that they or someone in their family had been threatened or injured by someone with a gun.
However, more than half (58%) said they had never asked patients whether they had guns in the home, and 80% reported never discussing gun use with patients. More than three-quarters said they had never discussed ways to reduce the risk for gun-related injury or death, and 62% had never talked about keeping guns away from children. Gun-owning physicians were more likely to ask about guns in the home.
Three-quarters of the physician respondents said there was a need for an educational program to help physicians counsel patients in firearm injury prevention.
aault@frontlinemedcom.com On Twitter @aliciaault
Listen to audio from the press briefing here:
And here:ORLANDO – Gun violence is a public health threat that needs to be addressed with the best scientific evidence to help reduce injuries and deaths, a new policy from the American College of Physicians proclaims.
"Access to firearms, especially firearms in the home, increases the likelihood that a person will be a victim of gun violence by homicide or suicide," Bob Doherty, ACP senior vice president of governmental affairs and public policy, said April 10 at the annual meeting of the American College of Physicians. "The evidence is very clear – the risk is higher.
The policy, published simultaneously in Annals of Internal Medicine (2014 April 10 [doi: 10.7326/M14-0216]), calls for universal criminal background checks and favors a prohibition on assault and semiautomatic weapons and large-capacity magazines. It updates the ACP’s 1996 policy.
"As an organization representing physicians who have firsthand experience with the devastating impact of firearm-related violence, ACP has a responsibility to participate in efforts to mitigate needless tragedies," Dr. Thomas Tape, chairman of the ACP health and public policy committee, said.
The ACP sought to balance its recommendations on gun violence and mental illness, Dr. Tape said, adding that any restrictions on gun ownership should not broadly target people with mental illness. Only a small portion of those who are mentally ill may be at risk for harming themselves or others, he said.
Of the 32,000 gun-related deaths in the United States each year, 11,000 are homicides, 19,000 are suicides, and the rest are unintentional, according to evidence from the 120 studies reviewed for the policy paper.
Determining who’s at the greatest risk for harming themselves or others "clearly begs for more research," said Dr. Tape. "We need better predictors."
Dr. Molly Cooke, ACP president, agreed, and noted that 30% of patients in primary care practices have a mental health diagnosis. With a high prevalence of illness and a low proportion of those who might actually do harm, "you’d be prohibiting lots of people from owning guns who would never harm anyone," Dr. Cooke said.
Dr. Tape also said the ACP believes that "the physician’s judgment is critically important." He said that often, patients will disclose their state of mind, allowing the physician to determine whether it is appropriate to alert the authorities or offer follow-up care.
Physicians are required by law to inform authorities when they believe a patient poses an imminent threat. "But the question is whether physicians should be required to more broadly report on individuals with mental illness who may pose a threat," Dr. Tape said.
Reporting requirements should not act as a disincentive to seek care, or interfere with the patient-physician relationship, according to the policy paper.
"The ACP strongly believes the patient-physician relationship should be protected from laws that prevent physicians from initiating a discussion about guns," Dr. Cooke said.
The policy paper also voices the ACP’s support for devices such as trigger locks, as well as efforts to keep guns out of the hands of children, adolescents, people with dementia, and those with substance use disorders.
According to a 2013 survey of ACP members, the vast majority agree that firearm injury is a public health issue. Close to 90% also said they supported mandatory background checks, mandatory registration, and a ban on assault weapons (Ann. Intern. Med. 2014 April 10 [doi: 10.7326/M13-1960]).
Of the 573 respondents, 64% reported having had patients who were injured or killed by a gun, and 14% said that they or someone in their family had been threatened or injured by someone with a gun.
However, more than half (58%) said they had never asked patients whether they had guns in the home, and 80% reported never discussing gun use with patients. More than three-quarters said they had never discussed ways to reduce the risk for gun-related injury or death, and 62% had never talked about keeping guns away from children. Gun-owning physicians were more likely to ask about guns in the home.
Three-quarters of the physician respondents said there was a need for an educational program to help physicians counsel patients in firearm injury prevention.
aault@frontlinemedcom.com On Twitter @aliciaault
Listen to audio from the press briefing here:
And here:ORLANDO – Gun violence is a public health threat that needs to be addressed with the best scientific evidence to help reduce injuries and deaths, a new policy from the American College of Physicians proclaims.
"Access to firearms, especially firearms in the home, increases the likelihood that a person will be a victim of gun violence by homicide or suicide," Bob Doherty, ACP senior vice president of governmental affairs and public policy, said April 10 at the annual meeting of the American College of Physicians. "The evidence is very clear – the risk is higher.
The policy, published simultaneously in Annals of Internal Medicine (2014 April 10 [doi: 10.7326/M14-0216]), calls for universal criminal background checks and favors a prohibition on assault and semiautomatic weapons and large-capacity magazines. It updates the ACP’s 1996 policy.
"As an organization representing physicians who have firsthand experience with the devastating impact of firearm-related violence, ACP has a responsibility to participate in efforts to mitigate needless tragedies," Dr. Thomas Tape, chairman of the ACP health and public policy committee, said.
The ACP sought to balance its recommendations on gun violence and mental illness, Dr. Tape said, adding that any restrictions on gun ownership should not broadly target people with mental illness. Only a small portion of those who are mentally ill may be at risk for harming themselves or others, he said.
Of the 32,000 gun-related deaths in the United States each year, 11,000 are homicides, 19,000 are suicides, and the rest are unintentional, according to evidence from the 120 studies reviewed for the policy paper.
Determining who’s at the greatest risk for harming themselves or others "clearly begs for more research," said Dr. Tape. "We need better predictors."
Dr. Molly Cooke, ACP president, agreed, and noted that 30% of patients in primary care practices have a mental health diagnosis. With a high prevalence of illness and a low proportion of those who might actually do harm, "you’d be prohibiting lots of people from owning guns who would never harm anyone," Dr. Cooke said.
Dr. Tape also said the ACP believes that "the physician’s judgment is critically important." He said that often, patients will disclose their state of mind, allowing the physician to determine whether it is appropriate to alert the authorities or offer follow-up care.
Physicians are required by law to inform authorities when they believe a patient poses an imminent threat. "But the question is whether physicians should be required to more broadly report on individuals with mental illness who may pose a threat," Dr. Tape said.
Reporting requirements should not act as a disincentive to seek care, or interfere with the patient-physician relationship, according to the policy paper.
"The ACP strongly believes the patient-physician relationship should be protected from laws that prevent physicians from initiating a discussion about guns," Dr. Cooke said.
The policy paper also voices the ACP’s support for devices such as trigger locks, as well as efforts to keep guns out of the hands of children, adolescents, people with dementia, and those with substance use disorders.
According to a 2013 survey of ACP members, the vast majority agree that firearm injury is a public health issue. Close to 90% also said they supported mandatory background checks, mandatory registration, and a ban on assault weapons (Ann. Intern. Med. 2014 April 10 [doi: 10.7326/M13-1960]).
Of the 573 respondents, 64% reported having had patients who were injured or killed by a gun, and 14% said that they or someone in their family had been threatened or injured by someone with a gun.
However, more than half (58%) said they had never asked patients whether they had guns in the home, and 80% reported never discussing gun use with patients. More than three-quarters said they had never discussed ways to reduce the risk for gun-related injury or death, and 62% had never talked about keeping guns away from children. Gun-owning physicians were more likely to ask about guns in the home.
Three-quarters of the physician respondents said there was a need for an educational program to help physicians counsel patients in firearm injury prevention.
aault@frontlinemedcom.com On Twitter @aliciaault
Listen to audio from the press briefing here:
And here:AT ACP INTERNAL MEDICINE 2014
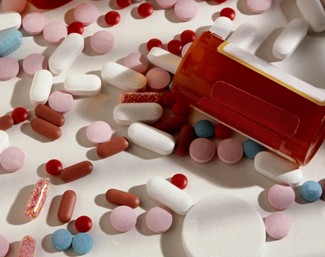
Prescription refills may continue after discontinuation
SAN FRANCISCO – Pharmacies refilled prescriptions for 1.5% of electronically discontinued medications, risking potential harm in 12% of cases, a study of 30,406 patients showed.
A retrospective study of records on 83,902 medications that had been electronically discontinued by physicians showed that 1,218 medications continued to be dispensed for 1,128 patients an average of one time in the year after discontinuation, Dr. Adrienne S. Allen reported at the annual meeting of the American College of Physicians.
Dr. Allen and her colleagues manually reviewed 416 charts to look for high-risk events and found suggestions of potential harm in 50 patients, including clinical reactions in 18 patients, laboratory abnormalities in 17, medication duplication in 8, and documented allergy in 7, said Dr. Allen, an internist in group practice in Danvers, Mass.
The continued refilling of discontinued prescriptions was seen for all drug classes and was most likely to affect patients with multiple prescriptions, nonwhite patients, and patients on Medicare or Medicaid (Ann. Intern. Med. 2012;157:700-5). Dr. Allen received a Junior Investigator Recognition Award at the meeting for her study.
Clinicians need to realize that dispensing of discontinued medication "does occur," Dr. Allen said. "Systemic intervention is needed to ensure that patients receive the correct medication."
Electronic health records with direct links to pharmacies make it easier to prescribe electronically, but most electronic health records do not transmit discontinuation orders to pharmacies, she noted.
The investigators studied records from 1 year in an integrated group practice with a common electronic health record that was separate from the group pharmacy’s computer system. They looked at medications commonly used in primary care: statins, antihypertensive medications, oral hypoglycemics, antiplatelet medications, and anticoagulants.
Among the 10 most commonly discontinued medications, dispensing continued for 1.4% of patients who had been using lisinopril or simvastatin, 1.2% of patients on hydrochlorothiazide, 1% on atenolol, 2.1% on amlodipine, 2.5% on metoprolol, 0.9% on metformin, 1.1% on enalapril, 1.5% on irbesartan, and 1.6% on warfarin.
The main reason for discontinuing a prescription was a dose adjustment. Other reasons included a change to an alternative medication, clinical intolerance, no further need for the drug, patient preference, or a laboratory abnormality.
Compared with white patients, black patients were 50% more likely and patients of other races were 60% more likely to have a discontinued medication dispensed. Patients covered by Medicaid were 40% more likely, and patients covered by Medicare were 70% more likely, to have a discontinued medication dispensed, compared with patients who had commercial insurance.
Patients on 15 or more medications were twice as likely to continue receiving a discontinued medication, compared with patients with fewer prescriptions.
Clinical reactions that suggested potential harm from the continued dispensing included hypotension in six patients; bradycardia, cough, or light-headedness in three patients each; and atrial flutter, GI upset, or myalgia in one patient each.
Laboratory abnormalities that suggested potential harm from refilling discontinued prescriptions included elevated liver function tests in five patients, hyponatremia or hypokalemia in four patients each, hyperkalemia in two patients, and increased levels of creatinine or uric acid in one patient each.
Dispensing of duplicate medications involved two statins in three patients, one patient each who got two sulfonylureas, two angiotensin-converting enzyme inhibitors, or two angiotensin receptor blockers, and two patients who got duplicate angiotensin-converting enzyme inhibitor/angiotensin receptor blocker medications. Medications continued to be dispensed despite records of allergy in seven patients, with allergy documented by cough in five patients and by rash or elevated creatinine phosphokinase in one patient each.
The National Institutes of Health funded the study. Dr. Allen reported having no relevant financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Pharmacies refilled prescriptions for 1.5% of electronically discontinued medications, risking potential harm in 12% of cases, a study of 30,406 patients showed.
A retrospective study of records on 83,902 medications that had been electronically discontinued by physicians showed that 1,218 medications continued to be dispensed for 1,128 patients an average of one time in the year after discontinuation, Dr. Adrienne S. Allen reported at the annual meeting of the American College of Physicians.
Dr. Allen and her colleagues manually reviewed 416 charts to look for high-risk events and found suggestions of potential harm in 50 patients, including clinical reactions in 18 patients, laboratory abnormalities in 17, medication duplication in 8, and documented allergy in 7, said Dr. Allen, an internist in group practice in Danvers, Mass.
The continued refilling of discontinued prescriptions was seen for all drug classes and was most likely to affect patients with multiple prescriptions, nonwhite patients, and patients on Medicare or Medicaid (Ann. Intern. Med. 2012;157:700-5). Dr. Allen received a Junior Investigator Recognition Award at the meeting for her study.
Clinicians need to realize that dispensing of discontinued medication "does occur," Dr. Allen said. "Systemic intervention is needed to ensure that patients receive the correct medication."
Electronic health records with direct links to pharmacies make it easier to prescribe electronically, but most electronic health records do not transmit discontinuation orders to pharmacies, she noted.
The investigators studied records from 1 year in an integrated group practice with a common electronic health record that was separate from the group pharmacy’s computer system. They looked at medications commonly used in primary care: statins, antihypertensive medications, oral hypoglycemics, antiplatelet medications, and anticoagulants.
Among the 10 most commonly discontinued medications, dispensing continued for 1.4% of patients who had been using lisinopril or simvastatin, 1.2% of patients on hydrochlorothiazide, 1% on atenolol, 2.1% on amlodipine, 2.5% on metoprolol, 0.9% on metformin, 1.1% on enalapril, 1.5% on irbesartan, and 1.6% on warfarin.
The main reason for discontinuing a prescription was a dose adjustment. Other reasons included a change to an alternative medication, clinical intolerance, no further need for the drug, patient preference, or a laboratory abnormality.
Compared with white patients, black patients were 50% more likely and patients of other races were 60% more likely to have a discontinued medication dispensed. Patients covered by Medicaid were 40% more likely, and patients covered by Medicare were 70% more likely, to have a discontinued medication dispensed, compared with patients who had commercial insurance.
Patients on 15 or more medications were twice as likely to continue receiving a discontinued medication, compared with patients with fewer prescriptions.
Clinical reactions that suggested potential harm from the continued dispensing included hypotension in six patients; bradycardia, cough, or light-headedness in three patients each; and atrial flutter, GI upset, or myalgia in one patient each.
Laboratory abnormalities that suggested potential harm from refilling discontinued prescriptions included elevated liver function tests in five patients, hyponatremia or hypokalemia in four patients each, hyperkalemia in two patients, and increased levels of creatinine or uric acid in one patient each.
Dispensing of duplicate medications involved two statins in three patients, one patient each who got two sulfonylureas, two angiotensin-converting enzyme inhibitors, or two angiotensin receptor blockers, and two patients who got duplicate angiotensin-converting enzyme inhibitor/angiotensin receptor blocker medications. Medications continued to be dispensed despite records of allergy in seven patients, with allergy documented by cough in five patients and by rash or elevated creatinine phosphokinase in one patient each.
The National Institutes of Health funded the study. Dr. Allen reported having no relevant financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Pharmacies refilled prescriptions for 1.5% of electronically discontinued medications, risking potential harm in 12% of cases, a study of 30,406 patients showed.
A retrospective study of records on 83,902 medications that had been electronically discontinued by physicians showed that 1,218 medications continued to be dispensed for 1,128 patients an average of one time in the year after discontinuation, Dr. Adrienne S. Allen reported at the annual meeting of the American College of Physicians.
Dr. Allen and her colleagues manually reviewed 416 charts to look for high-risk events and found suggestions of potential harm in 50 patients, including clinical reactions in 18 patients, laboratory abnormalities in 17, medication duplication in 8, and documented allergy in 7, said Dr. Allen, an internist in group practice in Danvers, Mass.
The continued refilling of discontinued prescriptions was seen for all drug classes and was most likely to affect patients with multiple prescriptions, nonwhite patients, and patients on Medicare or Medicaid (Ann. Intern. Med. 2012;157:700-5). Dr. Allen received a Junior Investigator Recognition Award at the meeting for her study.
Clinicians need to realize that dispensing of discontinued medication "does occur," Dr. Allen said. "Systemic intervention is needed to ensure that patients receive the correct medication."
Electronic health records with direct links to pharmacies make it easier to prescribe electronically, but most electronic health records do not transmit discontinuation orders to pharmacies, she noted.
The investigators studied records from 1 year in an integrated group practice with a common electronic health record that was separate from the group pharmacy’s computer system. They looked at medications commonly used in primary care: statins, antihypertensive medications, oral hypoglycemics, antiplatelet medications, and anticoagulants.
Among the 10 most commonly discontinued medications, dispensing continued for 1.4% of patients who had been using lisinopril or simvastatin, 1.2% of patients on hydrochlorothiazide, 1% on atenolol, 2.1% on amlodipine, 2.5% on metoprolol, 0.9% on metformin, 1.1% on enalapril, 1.5% on irbesartan, and 1.6% on warfarin.
The main reason for discontinuing a prescription was a dose adjustment. Other reasons included a change to an alternative medication, clinical intolerance, no further need for the drug, patient preference, or a laboratory abnormality.
Compared with white patients, black patients were 50% more likely and patients of other races were 60% more likely to have a discontinued medication dispensed. Patients covered by Medicaid were 40% more likely, and patients covered by Medicare were 70% more likely, to have a discontinued medication dispensed, compared with patients who had commercial insurance.
Patients on 15 or more medications were twice as likely to continue receiving a discontinued medication, compared with patients with fewer prescriptions.
Clinical reactions that suggested potential harm from the continued dispensing included hypotension in six patients; bradycardia, cough, or light-headedness in three patients each; and atrial flutter, GI upset, or myalgia in one patient each.
Laboratory abnormalities that suggested potential harm from refilling discontinued prescriptions included elevated liver function tests in five patients, hyponatremia or hypokalemia in four patients each, hyperkalemia in two patients, and increased levels of creatinine or uric acid in one patient each.
Dispensing of duplicate medications involved two statins in three patients, one patient each who got two sulfonylureas, two angiotensin-converting enzyme inhibitors, or two angiotensin receptor blockers, and two patients who got duplicate angiotensin-converting enzyme inhibitor/angiotensin receptor blocker medications. Medications continued to be dispensed despite records of allergy in seven patients, with allergy documented by cough in five patients and by rash or elevated creatinine phosphokinase in one patient each.
The National Institutes of Health funded the study. Dr. Allen reported having no relevant financial disclosures.
On Twitter @sherryboschert
AT ACP INTERNAL MEDICINE 2013
Major finding: Prescriptions that had been electronically discontinued were refilled 1.5% of the time, with potential harm in 12% of cases.
Data source: Retrospective studies of 83,902 discontinued medications for 30,406 patients in an integrated group practice.
Disclosures: The National Institutes of Health funded the study. Dr. Allen reported having no relevant financial disclosures.