User login
University of Colorado: Annual Internal Medicine Program
Expanded role seen for handy new spirometers
ESTES PARK, COLO. – The new generation of portable, user-friendly spirometry devices is likely to gain widespread acceptance among primary care physicians, one pulmonary expert predicted.
"Every subspecialist has their fifth vital sign. Mine is spirometry. Some of these handheld spirometers are really easy to use, and I think they’re going to make their way into office practice," said Dr. Robert L. Keith, professor of medicine at the University of Colorado, Denver.
Spirometry is a tool crucial to diagnosing chronic obstructive pulmonary disease in symptomatic patients. Plus, the forced expiratory volume in 1 second (FEV1) as measured using spirometry is the guideline-recommended means of categorizing patients as to disease stage and the most appropriate choice of treatment in individuals with COPD (Ann. Intern. Med. 2011;155:179-91).
Moreover, spirometry also provides an objective way to assess the effectiveness of treatment, the pulmonologist observed at a conference on internal medicine sponsored by the university.
"One of the neat things about the new software is it can provide quick data on lung age," Dr. Keith explained. "I can see a guy and tell him, ‘I’ve got your spirometry results, and your FEV1 is 41% and your FEV1/forced vital capacity ratio is 0.5,’ and he’s looking at me like, ‘What does that mean, doc?’
"But if I can say, ‘You’re 61 years old and your lungs are 75,’ that’s a take-home message pretty much anyone can understand," said Dr. Keith.
"I also use spirometry to follow patients, so I can say, ‘You’ve quit smoking and are using your medications, and guess what? Your lung age has improved from 75 to age 70,’ " he added.
Examples of state-of-the-art handheld spirometry devices on the market today include the Vitalograph copd-6, the PulmoLife, and PiKo-6, Dr. Keith noted.
"We tend to have a very rural population in Colorado that flows into Denver to be seen at the VA," [Veterans Affairs] he explained. "We give patients handheld spirometers to take back home to measure their disease and report in about their lung function."
Peak expiratory flow rate underestimates COPD severity, Dr. Keith cautioned, and cannot be used to diagnose COPD. Instead, peak expiratory flow is a spirometry measurement used as a tool in managing asthma.
He reported serving on speakers bureaus for Pfizer and Boehringer-Ingelheim.
ESTES PARK, COLO. – The new generation of portable, user-friendly spirometry devices is likely to gain widespread acceptance among primary care physicians, one pulmonary expert predicted.
"Every subspecialist has their fifth vital sign. Mine is spirometry. Some of these handheld spirometers are really easy to use, and I think they’re going to make their way into office practice," said Dr. Robert L. Keith, professor of medicine at the University of Colorado, Denver.
Spirometry is a tool crucial to diagnosing chronic obstructive pulmonary disease in symptomatic patients. Plus, the forced expiratory volume in 1 second (FEV1) as measured using spirometry is the guideline-recommended means of categorizing patients as to disease stage and the most appropriate choice of treatment in individuals with COPD (Ann. Intern. Med. 2011;155:179-91).
Moreover, spirometry also provides an objective way to assess the effectiveness of treatment, the pulmonologist observed at a conference on internal medicine sponsored by the university.
"One of the neat things about the new software is it can provide quick data on lung age," Dr. Keith explained. "I can see a guy and tell him, ‘I’ve got your spirometry results, and your FEV1 is 41% and your FEV1/forced vital capacity ratio is 0.5,’ and he’s looking at me like, ‘What does that mean, doc?’
"But if I can say, ‘You’re 61 years old and your lungs are 75,’ that’s a take-home message pretty much anyone can understand," said Dr. Keith.
"I also use spirometry to follow patients, so I can say, ‘You’ve quit smoking and are using your medications, and guess what? Your lung age has improved from 75 to age 70,’ " he added.
Examples of state-of-the-art handheld spirometry devices on the market today include the Vitalograph copd-6, the PulmoLife, and PiKo-6, Dr. Keith noted.
"We tend to have a very rural population in Colorado that flows into Denver to be seen at the VA," [Veterans Affairs] he explained. "We give patients handheld spirometers to take back home to measure their disease and report in about their lung function."
Peak expiratory flow rate underestimates COPD severity, Dr. Keith cautioned, and cannot be used to diagnose COPD. Instead, peak expiratory flow is a spirometry measurement used as a tool in managing asthma.
He reported serving on speakers bureaus for Pfizer and Boehringer-Ingelheim.
ESTES PARK, COLO. – The new generation of portable, user-friendly spirometry devices is likely to gain widespread acceptance among primary care physicians, one pulmonary expert predicted.
"Every subspecialist has their fifth vital sign. Mine is spirometry. Some of these handheld spirometers are really easy to use, and I think they’re going to make their way into office practice," said Dr. Robert L. Keith, professor of medicine at the University of Colorado, Denver.
Spirometry is a tool crucial to diagnosing chronic obstructive pulmonary disease in symptomatic patients. Plus, the forced expiratory volume in 1 second (FEV1) as measured using spirometry is the guideline-recommended means of categorizing patients as to disease stage and the most appropriate choice of treatment in individuals with COPD (Ann. Intern. Med. 2011;155:179-91).
Moreover, spirometry also provides an objective way to assess the effectiveness of treatment, the pulmonologist observed at a conference on internal medicine sponsored by the university.
"One of the neat things about the new software is it can provide quick data on lung age," Dr. Keith explained. "I can see a guy and tell him, ‘I’ve got your spirometry results, and your FEV1 is 41% and your FEV1/forced vital capacity ratio is 0.5,’ and he’s looking at me like, ‘What does that mean, doc?’
"But if I can say, ‘You’re 61 years old and your lungs are 75,’ that’s a take-home message pretty much anyone can understand," said Dr. Keith.
"I also use spirometry to follow patients, so I can say, ‘You’ve quit smoking and are using your medications, and guess what? Your lung age has improved from 75 to age 70,’ " he added.
Examples of state-of-the-art handheld spirometry devices on the market today include the Vitalograph copd-6, the PulmoLife, and PiKo-6, Dr. Keith noted.
"We tend to have a very rural population in Colorado that flows into Denver to be seen at the VA," [Veterans Affairs] he explained. "We give patients handheld spirometers to take back home to measure their disease and report in about their lung function."
Peak expiratory flow rate underestimates COPD severity, Dr. Keith cautioned, and cannot be used to diagnose COPD. Instead, peak expiratory flow is a spirometry measurement used as a tool in managing asthma.
He reported serving on speakers bureaus for Pfizer and Boehringer-Ingelheim.
EXPERT ANALYSIS FROM THE ANNUAL INTERNAL MEDICINE PROGRAM
Slap an ‘app’ on these five tough clinical decisions
ESTES PARK, COLO. – These days there’s a smartphone app for everything. But not all apps for clinical decision rules are truly helpful in making better patient care decisions in frontline primary care medicine, Dr. Robert E. Burke cautioned at a conference on internal medicine sponsored by the University of Colorado.
Five clinical decision rules have proven merit, each accessible via app as well as by an online website, he said. All five address medical issues that are common, important, and complex. What these rules have in common is excellent – not merely good – predictive value, thorough validation in multiple populations, a high likelihood that their use will influence patient management in individual cases, and an enthusiastic thumbs-up vote by physician-users.
These top-tier clinical decision rules address the following situations: determining which patients with community-acquired pneumonia can safely be managed at home, assessing whether a patient with chronic liver disease is likely to have advanced fibrosis or cirrhosis without resorting to liver biopsy, identifying who can be sent home safely after an episode of syncope, determining whether to prescribe oral anticoagulation for atrial fibrillation, and stratifying risk after a transient ischemic attack (TIA) or stroke.
These clinical decision rules are not a replacement for clinical judgment, but they do make risk/benefit calculations a lot easier, said Dr. Burke, a hospitalist at the Denver VA Medical Center and the university.
Triage of pneumonia patients. Pneumonia is the third most common reason for hospital admission as well as early readmission in the United States. So lots of different pneumonia severity scores have been developed. But few of them are any good, according to Dr. Burke.
Many of these subpar scores measure the likelihood that a patient with pneumonia will be admitted to the intensive care unit. That’s not what primary care physicians really want to know.
"Unfortunately, ICU admission rates vary widely in the U.S. and have nothing to do with how sick patients are or their comorbid conditions. It’s really not clear why the rates vary so much, but the predictive value of those scores is pretty poor, since ICU admission is a subjective thing," he explained.
The score he recommends is the Pneumonia Severity Index. It has been validated as an admission rule in several randomized trials totaling more than 4,000 patients. The score places patients into one of five risk categories. In the randomized trials, patients in the three lowest-risk categories had no negative outcomes when treated as outpatients. Plus, the use of the Pneumonia Severity Index reduced hospital admissions by up to 20%.
The score is calculated using 20 factors readily obtainable from the patient history, physical exam, and lab work. It’s a laborious calculation that’s perfect for an app. And the app exists: It’s called Simpli PSI.
Assessing fibrosis/cirrhosis risk in patients with chronic liver disease. Liver biopsy is painful, costly, decidedly not risk free, and often misleading due to the small tissue sample obtained. Transient elastography, a noninvasive ultrasound-based alternative, is promising but not ready for prime time. Yet knowing whether a patient has advanced fibrosis or cirrhosis is important in terms of prognosis, treatment, and surveillance strategy.
This is where the FIB-4 Index, a serum score for fibrosis, is of value. The FIB-4 Index is easily calculated from basic laboratory data. Findings from multiple studies have shown excellent discrimination regardless of whether patients had hepatitis C, hepatitis B, or nonalcoholic fatty liver disease.
"It has a c-statistic [equivalent to the area under the receiver operating characteristic curve] of 0.84. That’s about as good as it gets," according to the hospitalist.
The app is called Liver Calc. Like all the other apps Dr. Burke highlighted, it is available to iPhone users at the App Store.
"Or if you were to type in ‘FIB-4 Index’ on Google, you’ll find a website that will actually calculate the score online," he noted.
Whom to hospitalize for syncope. "Syncope is one of the most common things I see as a physician of in-patients," Dr. Burke said. "It accounts for maybe 1%-3% of emergency department visits and 6% of hospitalizations in the United States."
The San Francisco Syncope Rule is of proven value in helping to identify patients at low risk of serious outcomes in the 30 days following a syncopal episode. These are the patients who don’t need to undergo emergency department evaluation. The rule has been prospectively validated in tens of thousands of patients. It had a negative predictive value of 97% in a systematic review. The rule works less well in patients over age 65, where the likelihood of arrhythmia as the cause of syncope increases sharply. And the rule works best when applied only after a thorough history and physical exam aimed at finding a cause for the patient’s syncope.
"For example, the rule assumes you’ve already checked for hypoglycemia, a common cause of syncope," the hospitalist explained.
The San Francisco Syncope Rule is available in app form as Doctor Tools of the Trade.
Atrial fibrillation: To anticoagulate or not? This is a decision that entails balancing the reduction in stroke risk obtained with anticoagulation against the potential harm in the form of bleeding. The best tool for assessing the potential stroke-risk benefit is the CHA2DS2-VASc score, which represents a significant advance over the CHADS2 score, in Dr. Burke’s view.
"What the CHA2DS2-VASc score is really useful for, I think, is in putting people into low- or high-risk buckets. It takes people out of that intermediate-risk category in CHADS2," he explained.
It turns out that when physicians rely upon clinical intuition to estimate the risk of clinically important bleeding in patients on oral anticoagulation, they tend to overestimate the true risk. This observation has led to a proliferation of scales aimed at predicting who is likely to bleed when placed on warfarin. The best performer among them, regardless of whether the endpoint is any clinically relevant bleeding, major bleeding, or all-cause mortality, is the HAS-BLED score.
"I would encourage you to use both the CHA2DS2-VASc and HAS-BLED, and to use them at the same time. In some cases you’ll find the numbers are really discordant; there may be much more benefit than you thought, or much more risk," Dr. Burke said.
The focus-AF calculator is the app that will do the work.
Risk stratification after TIA or stroke. The ABCD2 score provides an estimate of stroke risk within 7 or 90 days after a TIA. This information helps establish the urgency of patient evaluation and risk factor management. A patient with an ABCD2 score of 4 or more should go straight to the emergency department, while a score of 3 or less indicates outpatient evaluation is appropriate. The Neuro Toolkit app will run the numbers.
Dr. Burke is keeping a watchful eye on a number of other clinical decision rules that, while promising, aren’t quite ready for prime time in his view. These include the FRAX score, the TIMI score, and the Marburg Heart Score. The Marburg score, for example, has been extensively validated as a tool to help primary care physicians decide whether chest pain is cardiac or noncardiac. But in the clinical trials, the score wasn’t compared to clinical intuition. That’s a problem.
"I think our clinical intuition here is relatively good. So I’d like to see data showing the rule adds something to clinical intuition before I recommend it," he said.
In a head-to-head comparative trial, the Pittsburgh Knee Rule outperformed the older Ottawa Knee Rule as an aid in figuring out who needs imaging after a knee injury. Impressive, in Dr. Burke’s view, but he’d like to see the results confirmed in a second study.
He reported having no financial conflicts.
ESTES PARK, COLO. – These days there’s a smartphone app for everything. But not all apps for clinical decision rules are truly helpful in making better patient care decisions in frontline primary care medicine, Dr. Robert E. Burke cautioned at a conference on internal medicine sponsored by the University of Colorado.
Five clinical decision rules have proven merit, each accessible via app as well as by an online website, he said. All five address medical issues that are common, important, and complex. What these rules have in common is excellent – not merely good – predictive value, thorough validation in multiple populations, a high likelihood that their use will influence patient management in individual cases, and an enthusiastic thumbs-up vote by physician-users.
These top-tier clinical decision rules address the following situations: determining which patients with community-acquired pneumonia can safely be managed at home, assessing whether a patient with chronic liver disease is likely to have advanced fibrosis or cirrhosis without resorting to liver biopsy, identifying who can be sent home safely after an episode of syncope, determining whether to prescribe oral anticoagulation for atrial fibrillation, and stratifying risk after a transient ischemic attack (TIA) or stroke.
These clinical decision rules are not a replacement for clinical judgment, but they do make risk/benefit calculations a lot easier, said Dr. Burke, a hospitalist at the Denver VA Medical Center and the university.
Triage of pneumonia patients. Pneumonia is the third most common reason for hospital admission as well as early readmission in the United States. So lots of different pneumonia severity scores have been developed. But few of them are any good, according to Dr. Burke.
Many of these subpar scores measure the likelihood that a patient with pneumonia will be admitted to the intensive care unit. That’s not what primary care physicians really want to know.
"Unfortunately, ICU admission rates vary widely in the U.S. and have nothing to do with how sick patients are or their comorbid conditions. It’s really not clear why the rates vary so much, but the predictive value of those scores is pretty poor, since ICU admission is a subjective thing," he explained.
The score he recommends is the Pneumonia Severity Index. It has been validated as an admission rule in several randomized trials totaling more than 4,000 patients. The score places patients into one of five risk categories. In the randomized trials, patients in the three lowest-risk categories had no negative outcomes when treated as outpatients. Plus, the use of the Pneumonia Severity Index reduced hospital admissions by up to 20%.
The score is calculated using 20 factors readily obtainable from the patient history, physical exam, and lab work. It’s a laborious calculation that’s perfect for an app. And the app exists: It’s called Simpli PSI.
Assessing fibrosis/cirrhosis risk in patients with chronic liver disease. Liver biopsy is painful, costly, decidedly not risk free, and often misleading due to the small tissue sample obtained. Transient elastography, a noninvasive ultrasound-based alternative, is promising but not ready for prime time. Yet knowing whether a patient has advanced fibrosis or cirrhosis is important in terms of prognosis, treatment, and surveillance strategy.
This is where the FIB-4 Index, a serum score for fibrosis, is of value. The FIB-4 Index is easily calculated from basic laboratory data. Findings from multiple studies have shown excellent discrimination regardless of whether patients had hepatitis C, hepatitis B, or nonalcoholic fatty liver disease.
"It has a c-statistic [equivalent to the area under the receiver operating characteristic curve] of 0.84. That’s about as good as it gets," according to the hospitalist.
The app is called Liver Calc. Like all the other apps Dr. Burke highlighted, it is available to iPhone users at the App Store.
"Or if you were to type in ‘FIB-4 Index’ on Google, you’ll find a website that will actually calculate the score online," he noted.
Whom to hospitalize for syncope. "Syncope is one of the most common things I see as a physician of in-patients," Dr. Burke said. "It accounts for maybe 1%-3% of emergency department visits and 6% of hospitalizations in the United States."
The San Francisco Syncope Rule is of proven value in helping to identify patients at low risk of serious outcomes in the 30 days following a syncopal episode. These are the patients who don’t need to undergo emergency department evaluation. The rule has been prospectively validated in tens of thousands of patients. It had a negative predictive value of 97% in a systematic review. The rule works less well in patients over age 65, where the likelihood of arrhythmia as the cause of syncope increases sharply. And the rule works best when applied only after a thorough history and physical exam aimed at finding a cause for the patient’s syncope.
"For example, the rule assumes you’ve already checked for hypoglycemia, a common cause of syncope," the hospitalist explained.
The San Francisco Syncope Rule is available in app form as Doctor Tools of the Trade.
Atrial fibrillation: To anticoagulate or not? This is a decision that entails balancing the reduction in stroke risk obtained with anticoagulation against the potential harm in the form of bleeding. The best tool for assessing the potential stroke-risk benefit is the CHA2DS2-VASc score, which represents a significant advance over the CHADS2 score, in Dr. Burke’s view.
"What the CHA2DS2-VASc score is really useful for, I think, is in putting people into low- or high-risk buckets. It takes people out of that intermediate-risk category in CHADS2," he explained.
It turns out that when physicians rely upon clinical intuition to estimate the risk of clinically important bleeding in patients on oral anticoagulation, they tend to overestimate the true risk. This observation has led to a proliferation of scales aimed at predicting who is likely to bleed when placed on warfarin. The best performer among them, regardless of whether the endpoint is any clinically relevant bleeding, major bleeding, or all-cause mortality, is the HAS-BLED score.
"I would encourage you to use both the CHA2DS2-VASc and HAS-BLED, and to use them at the same time. In some cases you’ll find the numbers are really discordant; there may be much more benefit than you thought, or much more risk," Dr. Burke said.
The focus-AF calculator is the app that will do the work.
Risk stratification after TIA or stroke. The ABCD2 score provides an estimate of stroke risk within 7 or 90 days after a TIA. This information helps establish the urgency of patient evaluation and risk factor management. A patient with an ABCD2 score of 4 or more should go straight to the emergency department, while a score of 3 or less indicates outpatient evaluation is appropriate. The Neuro Toolkit app will run the numbers.
Dr. Burke is keeping a watchful eye on a number of other clinical decision rules that, while promising, aren’t quite ready for prime time in his view. These include the FRAX score, the TIMI score, and the Marburg Heart Score. The Marburg score, for example, has been extensively validated as a tool to help primary care physicians decide whether chest pain is cardiac or noncardiac. But in the clinical trials, the score wasn’t compared to clinical intuition. That’s a problem.
"I think our clinical intuition here is relatively good. So I’d like to see data showing the rule adds something to clinical intuition before I recommend it," he said.
In a head-to-head comparative trial, the Pittsburgh Knee Rule outperformed the older Ottawa Knee Rule as an aid in figuring out who needs imaging after a knee injury. Impressive, in Dr. Burke’s view, but he’d like to see the results confirmed in a second study.
He reported having no financial conflicts.
ESTES PARK, COLO. – These days there’s a smartphone app for everything. But not all apps for clinical decision rules are truly helpful in making better patient care decisions in frontline primary care medicine, Dr. Robert E. Burke cautioned at a conference on internal medicine sponsored by the University of Colorado.
Five clinical decision rules have proven merit, each accessible via app as well as by an online website, he said. All five address medical issues that are common, important, and complex. What these rules have in common is excellent – not merely good – predictive value, thorough validation in multiple populations, a high likelihood that their use will influence patient management in individual cases, and an enthusiastic thumbs-up vote by physician-users.
These top-tier clinical decision rules address the following situations: determining which patients with community-acquired pneumonia can safely be managed at home, assessing whether a patient with chronic liver disease is likely to have advanced fibrosis or cirrhosis without resorting to liver biopsy, identifying who can be sent home safely after an episode of syncope, determining whether to prescribe oral anticoagulation for atrial fibrillation, and stratifying risk after a transient ischemic attack (TIA) or stroke.
These clinical decision rules are not a replacement for clinical judgment, but they do make risk/benefit calculations a lot easier, said Dr. Burke, a hospitalist at the Denver VA Medical Center and the university.
Triage of pneumonia patients. Pneumonia is the third most common reason for hospital admission as well as early readmission in the United States. So lots of different pneumonia severity scores have been developed. But few of them are any good, according to Dr. Burke.
Many of these subpar scores measure the likelihood that a patient with pneumonia will be admitted to the intensive care unit. That’s not what primary care physicians really want to know.
"Unfortunately, ICU admission rates vary widely in the U.S. and have nothing to do with how sick patients are or their comorbid conditions. It’s really not clear why the rates vary so much, but the predictive value of those scores is pretty poor, since ICU admission is a subjective thing," he explained.
The score he recommends is the Pneumonia Severity Index. It has been validated as an admission rule in several randomized trials totaling more than 4,000 patients. The score places patients into one of five risk categories. In the randomized trials, patients in the three lowest-risk categories had no negative outcomes when treated as outpatients. Plus, the use of the Pneumonia Severity Index reduced hospital admissions by up to 20%.
The score is calculated using 20 factors readily obtainable from the patient history, physical exam, and lab work. It’s a laborious calculation that’s perfect for an app. And the app exists: It’s called Simpli PSI.
Assessing fibrosis/cirrhosis risk in patients with chronic liver disease. Liver biopsy is painful, costly, decidedly not risk free, and often misleading due to the small tissue sample obtained. Transient elastography, a noninvasive ultrasound-based alternative, is promising but not ready for prime time. Yet knowing whether a patient has advanced fibrosis or cirrhosis is important in terms of prognosis, treatment, and surveillance strategy.
This is where the FIB-4 Index, a serum score for fibrosis, is of value. The FIB-4 Index is easily calculated from basic laboratory data. Findings from multiple studies have shown excellent discrimination regardless of whether patients had hepatitis C, hepatitis B, or nonalcoholic fatty liver disease.
"It has a c-statistic [equivalent to the area under the receiver operating characteristic curve] of 0.84. That’s about as good as it gets," according to the hospitalist.
The app is called Liver Calc. Like all the other apps Dr. Burke highlighted, it is available to iPhone users at the App Store.
"Or if you were to type in ‘FIB-4 Index’ on Google, you’ll find a website that will actually calculate the score online," he noted.
Whom to hospitalize for syncope. "Syncope is one of the most common things I see as a physician of in-patients," Dr. Burke said. "It accounts for maybe 1%-3% of emergency department visits and 6% of hospitalizations in the United States."
The San Francisco Syncope Rule is of proven value in helping to identify patients at low risk of serious outcomes in the 30 days following a syncopal episode. These are the patients who don’t need to undergo emergency department evaluation. The rule has been prospectively validated in tens of thousands of patients. It had a negative predictive value of 97% in a systematic review. The rule works less well in patients over age 65, where the likelihood of arrhythmia as the cause of syncope increases sharply. And the rule works best when applied only after a thorough history and physical exam aimed at finding a cause for the patient’s syncope.
"For example, the rule assumes you’ve already checked for hypoglycemia, a common cause of syncope," the hospitalist explained.
The San Francisco Syncope Rule is available in app form as Doctor Tools of the Trade.
Atrial fibrillation: To anticoagulate or not? This is a decision that entails balancing the reduction in stroke risk obtained with anticoagulation against the potential harm in the form of bleeding. The best tool for assessing the potential stroke-risk benefit is the CHA2DS2-VASc score, which represents a significant advance over the CHADS2 score, in Dr. Burke’s view.
"What the CHA2DS2-VASc score is really useful for, I think, is in putting people into low- or high-risk buckets. It takes people out of that intermediate-risk category in CHADS2," he explained.
It turns out that when physicians rely upon clinical intuition to estimate the risk of clinically important bleeding in patients on oral anticoagulation, they tend to overestimate the true risk. This observation has led to a proliferation of scales aimed at predicting who is likely to bleed when placed on warfarin. The best performer among them, regardless of whether the endpoint is any clinically relevant bleeding, major bleeding, or all-cause mortality, is the HAS-BLED score.
"I would encourage you to use both the CHA2DS2-VASc and HAS-BLED, and to use them at the same time. In some cases you’ll find the numbers are really discordant; there may be much more benefit than you thought, or much more risk," Dr. Burke said.
The focus-AF calculator is the app that will do the work.
Risk stratification after TIA or stroke. The ABCD2 score provides an estimate of stroke risk within 7 or 90 days after a TIA. This information helps establish the urgency of patient evaluation and risk factor management. A patient with an ABCD2 score of 4 or more should go straight to the emergency department, while a score of 3 or less indicates outpatient evaluation is appropriate. The Neuro Toolkit app will run the numbers.
Dr. Burke is keeping a watchful eye on a number of other clinical decision rules that, while promising, aren’t quite ready for prime time in his view. These include the FRAX score, the TIMI score, and the Marburg Heart Score. The Marburg score, for example, has been extensively validated as a tool to help primary care physicians decide whether chest pain is cardiac or noncardiac. But in the clinical trials, the score wasn’t compared to clinical intuition. That’s a problem.
"I think our clinical intuition here is relatively good. So I’d like to see data showing the rule adds something to clinical intuition before I recommend it," he said.
In a head-to-head comparative trial, the Pittsburgh Knee Rule outperformed the older Ottawa Knee Rule as an aid in figuring out who needs imaging after a knee injury. Impressive, in Dr. Burke’s view, but he’d like to see the results confirmed in a second study.
He reported having no financial conflicts.
EXPERT ANALYSIS FROM THE ANNUAL INTERNAL MEDICINE PROGRAM
Current diagnostic criteria for early rheumatoid arthritis must be used judiciously
ESTES PARK, COLO. – The most important thing to know about the current American College of Rheumatology/European League Against Rheumatism classification criteria for rheumatoid arthritis is that they are primarily a research tool and should only be applied diagnostically in selected circumstances.
The current criteria, known as the 2010 criteria, are markedly more effective at detecting RA early on – when it is far more treatment-responsive – than were the former 1987 criteria. That’s the upside. The downside of the 2010 criteria is unless they are employed judiciously, many patients will be inappropriately labeled as having RA and subjected to treatments they don’t actually need, Dr. Jason Kolfenbach explained at a conference on internal medicine sponsored by the University of Colorado.
Two essential preconditions must be met before the 2010 criteria can appropriately be brought to bear in diagnosing RA in the clinic. First, the patient has to have at least one swollen joint; joint pain without swelling isn’t sufficient.
Second, any alternative diagnoses that might better explain an individual’s synovitis must first be ruled out. It has been demonstrated that if the 2010 RA criteria are applied without first ruling out conditions including gout, lupus, and sarcoid, the false-positive rate, even in rheumatologists’ hands, is roughly 20%. When rheumatologists took the time to first remove the cases they thought likely to be something other than RA, however, the false-positive rate using the 2010 criteria fell to 9%, noted Dr. Kolfenbach, a rheumatologist at the university.
And then there’s the whole squirrelly matter of transient joint swelling.
Among patients with one or more swollen joints and no obvious etiology for their arthritis, the spontaneous remission rate approaches 50%. But among the subset of patients with at least one swollen joint who fulfill the 2010 criteria, the spontaneous remission rate appears to be much lower, on the order of 10% (Arthritis Rheum. 2012;64:389-93).
The 1987 criteria required radiographic evidence of erosions as well as the presence of subcutaneous rheumatoid nodules. Those are highly specific features of long-standing RA, but they’re not helpful in identifying patients with early disease. The impetus for developing the 2010 criteria was a persuasive body of evidence that in order to maximize outcomes physicians need to intervene earlier in the disease process than was possible using the 1987 criteria.
"The window for intervention is actually quite small. If you delay more than 3 or 4 months after symptom onset, your response to disease-modifying antirheumatic therapy is worse," he said.
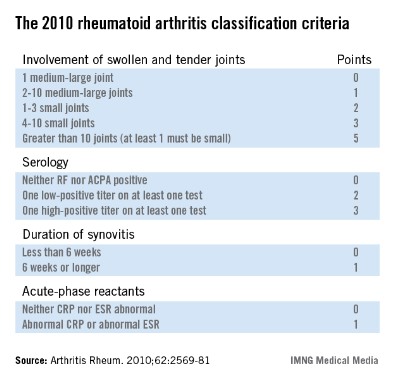
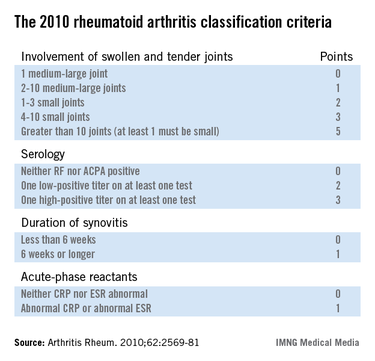
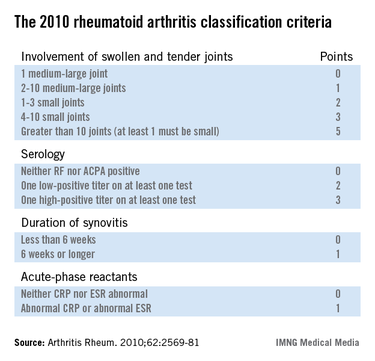
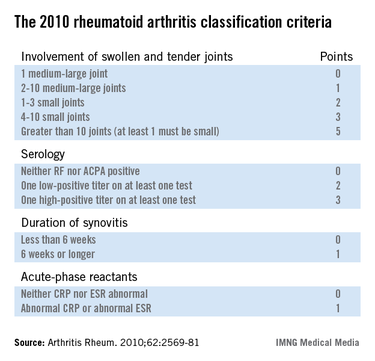
The 2010 criteria (Arthritis Rheum. 2010;62:2569-81) were developed through longitudinal follow-up of a cohort of patients who presented with an inflammatory arthritis that didn’t meet the 1987 criteria for RA. Investigators looked for features present initially that helped predict later definite RA. They found four: inflammatory joint involvement; antibody status; duration of synovitis; and the presence of inflammatory mediators, also known as acute phase reactants. Under the 2010 criteria, a score of 6 or more out of a possible 10 based upon these four elements is deemed definite RA. Of note, erosions and rheumatoid nodules aren’t part of the current diagnostic criteria.
Dr. Kolfenbach noted that in a large Dutch study, the sensitivity of the 2010 criteria for the diagnosis of RA as defined by the use of methotrexate or any other disease-modifying antirheumatic therapy within the first year of follow-up was 84%, an impressive absolute 23% improvement over the 61% sensitivity using the outmoded 1987 criteria (Arthritis Rheum. 2011;63:37-42).
"The problem, like with any test, is if we improve sensitivity it reduces specificity – and that increases the probability of inappropriately labeling someone as having rheumatoid arthritis," he observed.
Indeed, the Dutch study also showed that the diagnostic specificity of the 2010 criteria was only 60%, down from 74% when the 1987 criteria were applied to the same population.
So what’s the smart way to apply the 2010 classification criteria for RA?
"Clinical history and the physical exam are still king. If a patient comes through your office door with polyarticular swelling, mostly in the fingers and wrists, and it’s symmetrical, with a lack of systemic organ disease, that’s a person at much higher risk of having rheumatoid arthritis. It’s really reasonable then to apply the 2010 criteria and test for serologic antibodies and inflammatory markers. And if those are positive, then you’ve really cemented your feeling that this person very likely has rheumatoid arthritis," according to Dr. Kolfenbach.
Under the 2010 criteria, antibody testing remains "hugely important" in establishing the diagnosis of RA, he continued.
"If you don’t have a positive rheumatoid factor or anti-CCP [anti–cyclic citrullinated peptide] antibodies, you have to have more than 10 clinically involved joints to get to a score of 6. So we make the diagnosis of rheumatoid arthritis clinically and by listening to the patients and examining them, but antibodies are the icing on the cake. They’re a very, very important piece. And higher titers are specific for rheumatoid arthritis. A high-titer anti-CCP antibody level makes it very unlikely that it’s a false-positive test," the rheumatologist said.
He reported having no financial conflicts.
ESTES PARK, COLO. – The most important thing to know about the current American College of Rheumatology/European League Against Rheumatism classification criteria for rheumatoid arthritis is that they are primarily a research tool and should only be applied diagnostically in selected circumstances.
The current criteria, known as the 2010 criteria, are markedly more effective at detecting RA early on – when it is far more treatment-responsive – than were the former 1987 criteria. That’s the upside. The downside of the 2010 criteria is unless they are employed judiciously, many patients will be inappropriately labeled as having RA and subjected to treatments they don’t actually need, Dr. Jason Kolfenbach explained at a conference on internal medicine sponsored by the University of Colorado.
Two essential preconditions must be met before the 2010 criteria can appropriately be brought to bear in diagnosing RA in the clinic. First, the patient has to have at least one swollen joint; joint pain without swelling isn’t sufficient.
Second, any alternative diagnoses that might better explain an individual’s synovitis must first be ruled out. It has been demonstrated that if the 2010 RA criteria are applied without first ruling out conditions including gout, lupus, and sarcoid, the false-positive rate, even in rheumatologists’ hands, is roughly 20%. When rheumatologists took the time to first remove the cases they thought likely to be something other than RA, however, the false-positive rate using the 2010 criteria fell to 9%, noted Dr. Kolfenbach, a rheumatologist at the university.
And then there’s the whole squirrelly matter of transient joint swelling.
Among patients with one or more swollen joints and no obvious etiology for their arthritis, the spontaneous remission rate approaches 50%. But among the subset of patients with at least one swollen joint who fulfill the 2010 criteria, the spontaneous remission rate appears to be much lower, on the order of 10% (Arthritis Rheum. 2012;64:389-93).
The 1987 criteria required radiographic evidence of erosions as well as the presence of subcutaneous rheumatoid nodules. Those are highly specific features of long-standing RA, but they’re not helpful in identifying patients with early disease. The impetus for developing the 2010 criteria was a persuasive body of evidence that in order to maximize outcomes physicians need to intervene earlier in the disease process than was possible using the 1987 criteria.
"The window for intervention is actually quite small. If you delay more than 3 or 4 months after symptom onset, your response to disease-modifying antirheumatic therapy is worse," he said.
The 2010 criteria (Arthritis Rheum. 2010;62:2569-81) were developed through longitudinal follow-up of a cohort of patients who presented with an inflammatory arthritis that didn’t meet the 1987 criteria for RA. Investigators looked for features present initially that helped predict later definite RA. They found four: inflammatory joint involvement; antibody status; duration of synovitis; and the presence of inflammatory mediators, also known as acute phase reactants. Under the 2010 criteria, a score of 6 or more out of a possible 10 based upon these four elements is deemed definite RA. Of note, erosions and rheumatoid nodules aren’t part of the current diagnostic criteria.
Dr. Kolfenbach noted that in a large Dutch study, the sensitivity of the 2010 criteria for the diagnosis of RA as defined by the use of methotrexate or any other disease-modifying antirheumatic therapy within the first year of follow-up was 84%, an impressive absolute 23% improvement over the 61% sensitivity using the outmoded 1987 criteria (Arthritis Rheum. 2011;63:37-42).
"The problem, like with any test, is if we improve sensitivity it reduces specificity – and that increases the probability of inappropriately labeling someone as having rheumatoid arthritis," he observed.
Indeed, the Dutch study also showed that the diagnostic specificity of the 2010 criteria was only 60%, down from 74% when the 1987 criteria were applied to the same population.
So what’s the smart way to apply the 2010 classification criteria for RA?
"Clinical history and the physical exam are still king. If a patient comes through your office door with polyarticular swelling, mostly in the fingers and wrists, and it’s symmetrical, with a lack of systemic organ disease, that’s a person at much higher risk of having rheumatoid arthritis. It’s really reasonable then to apply the 2010 criteria and test for serologic antibodies and inflammatory markers. And if those are positive, then you’ve really cemented your feeling that this person very likely has rheumatoid arthritis," according to Dr. Kolfenbach.
Under the 2010 criteria, antibody testing remains "hugely important" in establishing the diagnosis of RA, he continued.
"If you don’t have a positive rheumatoid factor or anti-CCP [anti–cyclic citrullinated peptide] antibodies, you have to have more than 10 clinically involved joints to get to a score of 6. So we make the diagnosis of rheumatoid arthritis clinically and by listening to the patients and examining them, but antibodies are the icing on the cake. They’re a very, very important piece. And higher titers are specific for rheumatoid arthritis. A high-titer anti-CCP antibody level makes it very unlikely that it’s a false-positive test," the rheumatologist said.
He reported having no financial conflicts.
ESTES PARK, COLO. – The most important thing to know about the current American College of Rheumatology/European League Against Rheumatism classification criteria for rheumatoid arthritis is that they are primarily a research tool and should only be applied diagnostically in selected circumstances.
The current criteria, known as the 2010 criteria, are markedly more effective at detecting RA early on – when it is far more treatment-responsive – than were the former 1987 criteria. That’s the upside. The downside of the 2010 criteria is unless they are employed judiciously, many patients will be inappropriately labeled as having RA and subjected to treatments they don’t actually need, Dr. Jason Kolfenbach explained at a conference on internal medicine sponsored by the University of Colorado.
Two essential preconditions must be met before the 2010 criteria can appropriately be brought to bear in diagnosing RA in the clinic. First, the patient has to have at least one swollen joint; joint pain without swelling isn’t sufficient.
Second, any alternative diagnoses that might better explain an individual’s synovitis must first be ruled out. It has been demonstrated that if the 2010 RA criteria are applied without first ruling out conditions including gout, lupus, and sarcoid, the false-positive rate, even in rheumatologists’ hands, is roughly 20%. When rheumatologists took the time to first remove the cases they thought likely to be something other than RA, however, the false-positive rate using the 2010 criteria fell to 9%, noted Dr. Kolfenbach, a rheumatologist at the university.
And then there’s the whole squirrelly matter of transient joint swelling.
Among patients with one or more swollen joints and no obvious etiology for their arthritis, the spontaneous remission rate approaches 50%. But among the subset of patients with at least one swollen joint who fulfill the 2010 criteria, the spontaneous remission rate appears to be much lower, on the order of 10% (Arthritis Rheum. 2012;64:389-93).
The 1987 criteria required radiographic evidence of erosions as well as the presence of subcutaneous rheumatoid nodules. Those are highly specific features of long-standing RA, but they’re not helpful in identifying patients with early disease. The impetus for developing the 2010 criteria was a persuasive body of evidence that in order to maximize outcomes physicians need to intervene earlier in the disease process than was possible using the 1987 criteria.
"The window for intervention is actually quite small. If you delay more than 3 or 4 months after symptom onset, your response to disease-modifying antirheumatic therapy is worse," he said.
The 2010 criteria (Arthritis Rheum. 2010;62:2569-81) were developed through longitudinal follow-up of a cohort of patients who presented with an inflammatory arthritis that didn’t meet the 1987 criteria for RA. Investigators looked for features present initially that helped predict later definite RA. They found four: inflammatory joint involvement; antibody status; duration of synovitis; and the presence of inflammatory mediators, also known as acute phase reactants. Under the 2010 criteria, a score of 6 or more out of a possible 10 based upon these four elements is deemed definite RA. Of note, erosions and rheumatoid nodules aren’t part of the current diagnostic criteria.
Dr. Kolfenbach noted that in a large Dutch study, the sensitivity of the 2010 criteria for the diagnosis of RA as defined by the use of methotrexate or any other disease-modifying antirheumatic therapy within the first year of follow-up was 84%, an impressive absolute 23% improvement over the 61% sensitivity using the outmoded 1987 criteria (Arthritis Rheum. 2011;63:37-42).
"The problem, like with any test, is if we improve sensitivity it reduces specificity – and that increases the probability of inappropriately labeling someone as having rheumatoid arthritis," he observed.
Indeed, the Dutch study also showed that the diagnostic specificity of the 2010 criteria was only 60%, down from 74% when the 1987 criteria were applied to the same population.
So what’s the smart way to apply the 2010 classification criteria for RA?
"Clinical history and the physical exam are still king. If a patient comes through your office door with polyarticular swelling, mostly in the fingers and wrists, and it’s symmetrical, with a lack of systemic organ disease, that’s a person at much higher risk of having rheumatoid arthritis. It’s really reasonable then to apply the 2010 criteria and test for serologic antibodies and inflammatory markers. And if those are positive, then you’ve really cemented your feeling that this person very likely has rheumatoid arthritis," according to Dr. Kolfenbach.
Under the 2010 criteria, antibody testing remains "hugely important" in establishing the diagnosis of RA, he continued.
"If you don’t have a positive rheumatoid factor or anti-CCP [anti–cyclic citrullinated peptide] antibodies, you have to have more than 10 clinically involved joints to get to a score of 6. So we make the diagnosis of rheumatoid arthritis clinically and by listening to the patients and examining them, but antibodies are the icing on the cake. They’re a very, very important piece. And higher titers are specific for rheumatoid arthritis. A high-titer anti-CCP antibody level makes it very unlikely that it’s a false-positive test," the rheumatologist said.
He reported having no financial conflicts.
EXPERT ANALYSIS FROM THE ANNUAL INTERNAL MEDICINE PROGRAM
Anserine bursitis: Often-overlooked cause of knee pain
ESTES PARK, COLO. – Anserine bursitis is a common overuse injury frequently misinterpreted as osteoarthritis, according to Dr. Robert W. Janson.
The pain is focused at the medial aspect of the knee about 2 inches below the tibial plateau, or joint line. The bursa is located at the anatomic site known as the pes anserinus, or goose foot, where the conjoined tendons of the semitendinosus, gracilis, and sartorius muscles insert at the tibia, Dr. Janson explained at a conference on internal medicine sponsored by the University of Colorado.
"How do you find this bursa? It’s very easy. Take two fingers, grab the hamstring, and just run the two fingers down until they meet and you’re right there," said Dr. Janson, a rheumatologist at the university.
An affected patient will report the pain is worse with stair climbing or lying on one side with the knees opposed.
"Obese women with valgus knees tend to get this injury a lot," according to Dr. Janson.
Other risk factors for anserine bursitis are gait abnormalities or running and jogging.
Management is via the general measures utilized in treating overuse syndromes: rest, ice or heat, full-dose NSAIDs, and hamstring stretching.
If the pain persists for 6-8 weeks, a local injection of 10-20 mg of methylprednisolone with 1% lidocaine is enormously helpful. Find the tender area, mark it, direct the needle down to the bone, then back off about 1 mm and simply infiltrate that area, the rheumatologist advised.
He reported having no relevant financial conflicts.
ESTES PARK, COLO. – Anserine bursitis is a common overuse injury frequently misinterpreted as osteoarthritis, according to Dr. Robert W. Janson.
The pain is focused at the medial aspect of the knee about 2 inches below the tibial plateau, or joint line. The bursa is located at the anatomic site known as the pes anserinus, or goose foot, where the conjoined tendons of the semitendinosus, gracilis, and sartorius muscles insert at the tibia, Dr. Janson explained at a conference on internal medicine sponsored by the University of Colorado.
"How do you find this bursa? It’s very easy. Take two fingers, grab the hamstring, and just run the two fingers down until they meet and you’re right there," said Dr. Janson, a rheumatologist at the university.
An affected patient will report the pain is worse with stair climbing or lying on one side with the knees opposed.
"Obese women with valgus knees tend to get this injury a lot," according to Dr. Janson.
Other risk factors for anserine bursitis are gait abnormalities or running and jogging.
Management is via the general measures utilized in treating overuse syndromes: rest, ice or heat, full-dose NSAIDs, and hamstring stretching.
If the pain persists for 6-8 weeks, a local injection of 10-20 mg of methylprednisolone with 1% lidocaine is enormously helpful. Find the tender area, mark it, direct the needle down to the bone, then back off about 1 mm and simply infiltrate that area, the rheumatologist advised.
He reported having no relevant financial conflicts.
ESTES PARK, COLO. – Anserine bursitis is a common overuse injury frequently misinterpreted as osteoarthritis, according to Dr. Robert W. Janson.
The pain is focused at the medial aspect of the knee about 2 inches below the tibial plateau, or joint line. The bursa is located at the anatomic site known as the pes anserinus, or goose foot, where the conjoined tendons of the semitendinosus, gracilis, and sartorius muscles insert at the tibia, Dr. Janson explained at a conference on internal medicine sponsored by the University of Colorado.
"How do you find this bursa? It’s very easy. Take two fingers, grab the hamstring, and just run the two fingers down until they meet and you’re right there," said Dr. Janson, a rheumatologist at the university.
An affected patient will report the pain is worse with stair climbing or lying on one side with the knees opposed.
"Obese women with valgus knees tend to get this injury a lot," according to Dr. Janson.
Other risk factors for anserine bursitis are gait abnormalities or running and jogging.
Management is via the general measures utilized in treating overuse syndromes: rest, ice or heat, full-dose NSAIDs, and hamstring stretching.
If the pain persists for 6-8 weeks, a local injection of 10-20 mg of methylprednisolone with 1% lidocaine is enormously helpful. Find the tender area, mark it, direct the needle down to the bone, then back off about 1 mm and simply infiltrate that area, the rheumatologist advised.
He reported having no relevant financial conflicts.
EXPERT ANALYSIS from the annual internal medicine program
Expect miracles: New drug for hepatitis C may put treatment in the hands of primary care
ESTES PARK, COLO. – Treatment of hepatitis C infection is likely to shift from gastroenterology and hepatology clinics to primary care physicians’ offices, perhaps as early as next year.
That’s the prediction of Dr. Gregory T. Everson, who cited rapid progress in developing interferon-free treatment regimens as the driving force behind what is anticipated to be a huge change in clinical practice, given that there are an estimated 5 million or more patients with hepatitis C virus (HCV) infection in the United States
Five major pharmaceutical companies are developing oral, interferon-free HCV treatment regimens based upon still-investigational direct-acting antiviral agents (DAAs) that target HCV proteins and their functions. The clinical trials experience to date indicates these DAA-based regimens have substantially higher cure rates, far better tolerability and safety, and a much lower pill burden. Also, they are vastly simpler to administer than are current standard therapies. And all this is being achieved with a 12-week treatment duration instead of the 24 weeks required with standard therapy in 2013, Dr. Everson said at a conference on internal medicine sponsored by the University of Colorado.
"In the past I could say we really had pretty [intolerable] therapy, and it was pretty difficult for patients to take it. Interferon-free therapy is evolving rapidly, and I hope that it will be in primary care physicians’ backyards in the near future. I think this is probably going to be a treatment that you all provide," added Dr. Everson, professor of medicine and director of hepatology at the university.
Indeed, at hepatology clinics around the country, patients with early-stage HCV and their physicians are taking a "wait until next year" attitude toward starting treatment in anticipation that the Food and Drug Administration could approve the first of these new DAAs, sofosbuvir, before the year’s end.
The number of prescriptions for HCV therapy for treatment-naive patients at the University of Colorado clinic has plummeted in 2013 compared with 2012. The only patients starting treatment now are those with advanced HCV liver disease, to halt further disease progression and reduce the risk of developing hepatocellular carcinoma, according to Dr. Everson.
The FDA has granted Gilead Sciences priority review status for sofosbuvir, an oral inhibitor of nucleotide N55b polymerase, with a target decision date in early December. The application for marketing approval is for two indications. One involves sofosbuvir as part of a 12-week, triple-therapy regimen including pegylated interferon and ribavirin in treatment-naive patients with HCV genotypes 1, 4, 5, and 6, based in large part upon the highly favorable results of the phase III NEUTRINO trial (N. Engl. J. Med. 2013;368:1878-87).
The other proposed indication is sofosbuvir in combination with ribavirin as an interferon-free, 12-week regimen in patients with HCV genotypes 2 or 3, based upon the results of the FISSION and POSITRON trials (N. Engl. J. Med. 2013;368:1867-77).
In the NEUTRINO trial, 12 weeks of triple-therapy with sofosbuvir/interferon/ribavirin resulted in a 90% cure rate in patients with HCV genotype 1, which accounts for three-quarters of all HCV infections in the United States. The dropout rate due to side effects was a mere 2%. In contrast, today’s standard therapy, consisting of either of the protease inhibitors telaprevir (Incivek) or boceprevir (Victrelis) combined with pegylated interferon and ribavirin, has a 70%-75% cure rate. And many patients can’t tolerate or are ineligible for interferon.
"When I started treating hepatitis C patients 25 years ago, I was happy because the ALT would normalize in half the patients with genotype 1, but I wasn’t curing anybody. And now triple therapy with sofosbuvir, with a 90% cure rate, could be approved by the end of the year," Dr. Everson marveled.
In the FISSION trial, treatment-naive patients with HCV genotype 2 had a 97% cure rate with 12 weeks of sofosbuvir/ribavirin compared with 78% in those assigned to today’s standard regimen of 24 weeks of pegylated interferon/ribavirin. And sofosbuvir is just one pill per day, coupled with ribavirin at two or three pills twice daily.
In POSITRON, conducted in patients who had relapsed or were nonresponders to the standard 24 weeks of pegylated interferon/ribavirin, 12 weeks of sofosbuvir/ribavirin had an 86% response rate in patients with HCV genotype 2. With an additional 4 weeks of the interferon-free regimen, the cure rate climbed to 94%. Cure rates were lower in genotype 3 patients, but of note, the cure rate in treatment-experienced genotype 3 patients with cirrhosis more than tripled from 19% with 12 weeks of sofosbuvir/ribavirin to 61% with 16 weeks.
Other oral DAAs in the developmental pipeline include simeprevir, daclatasvir, and asunaprevir. The clinical trials experience to date demonstrate that combination therapy with more than one DAA boosts the cure rate even higher than with sofosbuvir/ribavirin. For example, in the phase II, open-label AVIATOR study, 12 weeks of a cocktail comprising three DAAs plus ribavirin brought a 96% cure rate in treatment-naive patients with HCV genotype 1 and a 93% cure rate in those who had previously failed on standard interferon-containing therapy. The AVIATOR cocktail is being formulated as a two-pills-per-day regimen.
Further, Dr. Everson was principal investigator in a Bristol-Myers Squibb–sponsored study of a totally interferon- and ribavirin-free regimen consisting of triple-DAA therapy. Each of the DAAs has a different mechanism of action: Daclatasvir is an inhibitor of the HCV NS5a protein; asunaprevir is an NS3 protease inhibitor; and the agent known for now as BMS-791325 is a nonnucleoside polymerase NS5b inhibitor. The cure rate with 12 weeks of triple-DAA therapy in treatment-naive, noncirrhotic patients with HCV genotype 1 was 94%.
Hepatologists define cure of HCV as an SVR12, or a sustained virologic response featuring no detectable HCV RNA in the blood for 12 weeks after the conclusion of therapy. The likelihood that a patient who achieves an SVR12 will remain HCV free through 10 years is 99%-100% (Gastroenterology 2010;139:1593-1601).
"The future looks pretty good for hepatitis C patients," Dr. Everson observed.
Moreover, curing HCV is going to have major downstream benefits for the health care system, he added. Today, 36% of all patients on the liver transplantation waiting list have HCV; that proportion will drop substantially. There will be fewer cases of hepatocellular carcinoma, B-cell lymphoma, and adult-onset diabetes, a drop in HCV-related autoimmune disorders, and reduced costs of care for patients with chronic HCV.
Dr. Everson reported that he receives research grants from and/or serves as a consultant to or advisory board member for roughly two dozen pharmaceutical companies.
ESTES PARK, COLO. – Treatment of hepatitis C infection is likely to shift from gastroenterology and hepatology clinics to primary care physicians’ offices, perhaps as early as next year.
That’s the prediction of Dr. Gregory T. Everson, who cited rapid progress in developing interferon-free treatment regimens as the driving force behind what is anticipated to be a huge change in clinical practice, given that there are an estimated 5 million or more patients with hepatitis C virus (HCV) infection in the United States
Five major pharmaceutical companies are developing oral, interferon-free HCV treatment regimens based upon still-investigational direct-acting antiviral agents (DAAs) that target HCV proteins and their functions. The clinical trials experience to date indicates these DAA-based regimens have substantially higher cure rates, far better tolerability and safety, and a much lower pill burden. Also, they are vastly simpler to administer than are current standard therapies. And all this is being achieved with a 12-week treatment duration instead of the 24 weeks required with standard therapy in 2013, Dr. Everson said at a conference on internal medicine sponsored by the University of Colorado.
"In the past I could say we really had pretty [intolerable] therapy, and it was pretty difficult for patients to take it. Interferon-free therapy is evolving rapidly, and I hope that it will be in primary care physicians’ backyards in the near future. I think this is probably going to be a treatment that you all provide," added Dr. Everson, professor of medicine and director of hepatology at the university.
Indeed, at hepatology clinics around the country, patients with early-stage HCV and their physicians are taking a "wait until next year" attitude toward starting treatment in anticipation that the Food and Drug Administration could approve the first of these new DAAs, sofosbuvir, before the year’s end.
The number of prescriptions for HCV therapy for treatment-naive patients at the University of Colorado clinic has plummeted in 2013 compared with 2012. The only patients starting treatment now are those with advanced HCV liver disease, to halt further disease progression and reduce the risk of developing hepatocellular carcinoma, according to Dr. Everson.
The FDA has granted Gilead Sciences priority review status for sofosbuvir, an oral inhibitor of nucleotide N55b polymerase, with a target decision date in early December. The application for marketing approval is for two indications. One involves sofosbuvir as part of a 12-week, triple-therapy regimen including pegylated interferon and ribavirin in treatment-naive patients with HCV genotypes 1, 4, 5, and 6, based in large part upon the highly favorable results of the phase III NEUTRINO trial (N. Engl. J. Med. 2013;368:1878-87).
The other proposed indication is sofosbuvir in combination with ribavirin as an interferon-free, 12-week regimen in patients with HCV genotypes 2 or 3, based upon the results of the FISSION and POSITRON trials (N. Engl. J. Med. 2013;368:1867-77).
In the NEUTRINO trial, 12 weeks of triple-therapy with sofosbuvir/interferon/ribavirin resulted in a 90% cure rate in patients with HCV genotype 1, which accounts for three-quarters of all HCV infections in the United States. The dropout rate due to side effects was a mere 2%. In contrast, today’s standard therapy, consisting of either of the protease inhibitors telaprevir (Incivek) or boceprevir (Victrelis) combined with pegylated interferon and ribavirin, has a 70%-75% cure rate. And many patients can’t tolerate or are ineligible for interferon.
"When I started treating hepatitis C patients 25 years ago, I was happy because the ALT would normalize in half the patients with genotype 1, but I wasn’t curing anybody. And now triple therapy with sofosbuvir, with a 90% cure rate, could be approved by the end of the year," Dr. Everson marveled.
In the FISSION trial, treatment-naive patients with HCV genotype 2 had a 97% cure rate with 12 weeks of sofosbuvir/ribavirin compared with 78% in those assigned to today’s standard regimen of 24 weeks of pegylated interferon/ribavirin. And sofosbuvir is just one pill per day, coupled with ribavirin at two or three pills twice daily.
In POSITRON, conducted in patients who had relapsed or were nonresponders to the standard 24 weeks of pegylated interferon/ribavirin, 12 weeks of sofosbuvir/ribavirin had an 86% response rate in patients with HCV genotype 2. With an additional 4 weeks of the interferon-free regimen, the cure rate climbed to 94%. Cure rates were lower in genotype 3 patients, but of note, the cure rate in treatment-experienced genotype 3 patients with cirrhosis more than tripled from 19% with 12 weeks of sofosbuvir/ribavirin to 61% with 16 weeks.
Other oral DAAs in the developmental pipeline include simeprevir, daclatasvir, and asunaprevir. The clinical trials experience to date demonstrate that combination therapy with more than one DAA boosts the cure rate even higher than with sofosbuvir/ribavirin. For example, in the phase II, open-label AVIATOR study, 12 weeks of a cocktail comprising three DAAs plus ribavirin brought a 96% cure rate in treatment-naive patients with HCV genotype 1 and a 93% cure rate in those who had previously failed on standard interferon-containing therapy. The AVIATOR cocktail is being formulated as a two-pills-per-day regimen.
Further, Dr. Everson was principal investigator in a Bristol-Myers Squibb–sponsored study of a totally interferon- and ribavirin-free regimen consisting of triple-DAA therapy. Each of the DAAs has a different mechanism of action: Daclatasvir is an inhibitor of the HCV NS5a protein; asunaprevir is an NS3 protease inhibitor; and the agent known for now as BMS-791325 is a nonnucleoside polymerase NS5b inhibitor. The cure rate with 12 weeks of triple-DAA therapy in treatment-naive, noncirrhotic patients with HCV genotype 1 was 94%.
Hepatologists define cure of HCV as an SVR12, or a sustained virologic response featuring no detectable HCV RNA in the blood for 12 weeks after the conclusion of therapy. The likelihood that a patient who achieves an SVR12 will remain HCV free through 10 years is 99%-100% (Gastroenterology 2010;139:1593-1601).
"The future looks pretty good for hepatitis C patients," Dr. Everson observed.
Moreover, curing HCV is going to have major downstream benefits for the health care system, he added. Today, 36% of all patients on the liver transplantation waiting list have HCV; that proportion will drop substantially. There will be fewer cases of hepatocellular carcinoma, B-cell lymphoma, and adult-onset diabetes, a drop in HCV-related autoimmune disorders, and reduced costs of care for patients with chronic HCV.
Dr. Everson reported that he receives research grants from and/or serves as a consultant to or advisory board member for roughly two dozen pharmaceutical companies.
ESTES PARK, COLO. – Treatment of hepatitis C infection is likely to shift from gastroenterology and hepatology clinics to primary care physicians’ offices, perhaps as early as next year.
That’s the prediction of Dr. Gregory T. Everson, who cited rapid progress in developing interferon-free treatment regimens as the driving force behind what is anticipated to be a huge change in clinical practice, given that there are an estimated 5 million or more patients with hepatitis C virus (HCV) infection in the United States
Five major pharmaceutical companies are developing oral, interferon-free HCV treatment regimens based upon still-investigational direct-acting antiviral agents (DAAs) that target HCV proteins and their functions. The clinical trials experience to date indicates these DAA-based regimens have substantially higher cure rates, far better tolerability and safety, and a much lower pill burden. Also, they are vastly simpler to administer than are current standard therapies. And all this is being achieved with a 12-week treatment duration instead of the 24 weeks required with standard therapy in 2013, Dr. Everson said at a conference on internal medicine sponsored by the University of Colorado.
"In the past I could say we really had pretty [intolerable] therapy, and it was pretty difficult for patients to take it. Interferon-free therapy is evolving rapidly, and I hope that it will be in primary care physicians’ backyards in the near future. I think this is probably going to be a treatment that you all provide," added Dr. Everson, professor of medicine and director of hepatology at the university.
Indeed, at hepatology clinics around the country, patients with early-stage HCV and their physicians are taking a "wait until next year" attitude toward starting treatment in anticipation that the Food and Drug Administration could approve the first of these new DAAs, sofosbuvir, before the year’s end.
The number of prescriptions for HCV therapy for treatment-naive patients at the University of Colorado clinic has plummeted in 2013 compared with 2012. The only patients starting treatment now are those with advanced HCV liver disease, to halt further disease progression and reduce the risk of developing hepatocellular carcinoma, according to Dr. Everson.
The FDA has granted Gilead Sciences priority review status for sofosbuvir, an oral inhibitor of nucleotide N55b polymerase, with a target decision date in early December. The application for marketing approval is for two indications. One involves sofosbuvir as part of a 12-week, triple-therapy regimen including pegylated interferon and ribavirin in treatment-naive patients with HCV genotypes 1, 4, 5, and 6, based in large part upon the highly favorable results of the phase III NEUTRINO trial (N. Engl. J. Med. 2013;368:1878-87).
The other proposed indication is sofosbuvir in combination with ribavirin as an interferon-free, 12-week regimen in patients with HCV genotypes 2 or 3, based upon the results of the FISSION and POSITRON trials (N. Engl. J. Med. 2013;368:1867-77).
In the NEUTRINO trial, 12 weeks of triple-therapy with sofosbuvir/interferon/ribavirin resulted in a 90% cure rate in patients with HCV genotype 1, which accounts for three-quarters of all HCV infections in the United States. The dropout rate due to side effects was a mere 2%. In contrast, today’s standard therapy, consisting of either of the protease inhibitors telaprevir (Incivek) or boceprevir (Victrelis) combined with pegylated interferon and ribavirin, has a 70%-75% cure rate. And many patients can’t tolerate or are ineligible for interferon.
"When I started treating hepatitis C patients 25 years ago, I was happy because the ALT would normalize in half the patients with genotype 1, but I wasn’t curing anybody. And now triple therapy with sofosbuvir, with a 90% cure rate, could be approved by the end of the year," Dr. Everson marveled.
In the FISSION trial, treatment-naive patients with HCV genotype 2 had a 97% cure rate with 12 weeks of sofosbuvir/ribavirin compared with 78% in those assigned to today’s standard regimen of 24 weeks of pegylated interferon/ribavirin. And sofosbuvir is just one pill per day, coupled with ribavirin at two or three pills twice daily.
In POSITRON, conducted in patients who had relapsed or were nonresponders to the standard 24 weeks of pegylated interferon/ribavirin, 12 weeks of sofosbuvir/ribavirin had an 86% response rate in patients with HCV genotype 2. With an additional 4 weeks of the interferon-free regimen, the cure rate climbed to 94%. Cure rates were lower in genotype 3 patients, but of note, the cure rate in treatment-experienced genotype 3 patients with cirrhosis more than tripled from 19% with 12 weeks of sofosbuvir/ribavirin to 61% with 16 weeks.
Other oral DAAs in the developmental pipeline include simeprevir, daclatasvir, and asunaprevir. The clinical trials experience to date demonstrate that combination therapy with more than one DAA boosts the cure rate even higher than with sofosbuvir/ribavirin. For example, in the phase II, open-label AVIATOR study, 12 weeks of a cocktail comprising three DAAs plus ribavirin brought a 96% cure rate in treatment-naive patients with HCV genotype 1 and a 93% cure rate in those who had previously failed on standard interferon-containing therapy. The AVIATOR cocktail is being formulated as a two-pills-per-day regimen.
Further, Dr. Everson was principal investigator in a Bristol-Myers Squibb–sponsored study of a totally interferon- and ribavirin-free regimen consisting of triple-DAA therapy. Each of the DAAs has a different mechanism of action: Daclatasvir is an inhibitor of the HCV NS5a protein; asunaprevir is an NS3 protease inhibitor; and the agent known for now as BMS-791325 is a nonnucleoside polymerase NS5b inhibitor. The cure rate with 12 weeks of triple-DAA therapy in treatment-naive, noncirrhotic patients with HCV genotype 1 was 94%.
Hepatologists define cure of HCV as an SVR12, or a sustained virologic response featuring no detectable HCV RNA in the blood for 12 weeks after the conclusion of therapy. The likelihood that a patient who achieves an SVR12 will remain HCV free through 10 years is 99%-100% (Gastroenterology 2010;139:1593-1601).
"The future looks pretty good for hepatitis C patients," Dr. Everson observed.
Moreover, curing HCV is going to have major downstream benefits for the health care system, he added. Today, 36% of all patients on the liver transplantation waiting list have HCV; that proportion will drop substantially. There will be fewer cases of hepatocellular carcinoma, B-cell lymphoma, and adult-onset diabetes, a drop in HCV-related autoimmune disorders, and reduced costs of care for patients with chronic HCV.
Dr. Everson reported that he receives research grants from and/or serves as a consultant to or advisory board member for roughly two dozen pharmaceutical companies.
AT THE ANNUAL INTERNAL MEDICINE PROGRAM
Adult ADHD: Nonpharmacologic interventions are useful adjuncts
ESTES PARK, COLO. – Hands down, the most effective treatment for adult attention-deficit/hyperactivity disorder is psychostimulants.
The nonstimulant medications are a second-line alternative with less robust benefits, but they come in quite handy in selected situations, Dr. Robert D. Davies noted at a conference on internal medicine sponsored by the University of Colorado.
Also, a wealth of nonpharmacologic treatments are available. These include mindfulness exercises, cognitive behavioral therapy, life coaching, psychoeducational self-help audio books, and support groups.
"They’re great adjunct treatments, but in and of themselves not great solo treatments," according to Dr. Davies. "There’s an analogy to having poor near vision, so you never learned to read, and then suddenly you get glasses. That’s kind of like getting on medications: You still wouldn’t know how to read, but now you could learn how. So trying the nonpharmacologic interventions will be pretty frustrating for somebody who wants to avoid medications. You can try using those tools to help them with organization and those sorts of things, but it’s usually a huge struggle. Instead, put them on meds, teach them some of those things, and then see if off meds they can maintain those gains," advised Dr. Davies, a psychiatrist at the university.
A tip on self-help books geared to adults with attention-deficit/hyperactivity disorder (ADHD): "If you have a patient who’s never been able to get through a book in their life, don’t recommend a book that’s going to help them. ADHD folks do better with books on tape." Among the many on the market, Dr. Davies mentioned "Driven to Distraction" by Dr. Edward M. Hallowell and Dr. John J. Ratey as particularly good.
The psychostimulants fall into two categories: methylphenidate formulations and dextroamphetamine formulations. They’re equally effective, with the caveat that 20% of the population doesn’t respond to the methylphenidate drugs; however, they do respond to the dextroamphetamines. It’s a class effect, so when a patient isn’t doing well on a methylphenidate, don’t bother switching to a different methylphenidate drug; move on to a dextroamphetamine formulation.
Only four stimulants are approved by the Food and Drug Administration for adults: Adderal XR (dextroamphetamine/amphetamine), with a 9-hour duration of action and 15- to 30-mg dosage range; Focalin XR (dexmethylphenidate), with an 8- to 12-hour duration of action and dosage range of 20-40 mg; Vyvanse (lisdexamfetamine dimesylate), with a duration of 12 hours and dosing at 30-70 mg; and Concerta (methylphenidate extended-release), with a 12-hour duration of action and dosage range of 18-54 mg.
A history of drug abuse is a consideration in choosing a pharmacologic agent, but it isn’t necessarily a deal breaker in prescribing a stimulant. Some individuals with ADHD used stimulants or cocaine illicitly while students as a form of self-medication to enhance academic performance; they may be reasonable candidates for Concerta or Vyvanse, which have extremely low abuse potential. On the other hand, Dr. Davies recommended against prescribing stimulants for adult ADHD patients with a history of opiate or methamphetamine abuse.
Other situations where stimulant medications are best avoided include patients with medical conditions including heart disease, hypertension, and seizure disorders.
Only one nonstimulant medication is approved in adults: Strattera (atomoxetine). The reduction in ADHD symptoms is roughly 30% less than with stimulants. However, it is a once-daily drug, which is an advantage.
"When I’m treating anxiety or ADHD, especially in adults, a longer-acting drug is better. I always try to get patients away from that on-off phenomenon. That’s a feeling they don’t like," the psychiatrist continued.
Adults with ADHD may need pharmacologic assistance not only during a lengthy workday, but in the evening as well.
Nonstimulants that are sometimes used off-label in adults include Wellbutrin (bupropion), which is approved for children with ADHD. It is about half as effective as a stimulant medication. Effexor (venlafaxine) and Provigil (modafanil) are other nonstimulants used off-label; neither has been well studied in adult ADHD, according to Dr. Davies.
Adults with ADHD don’t develop tolerance to stimulant medications, unlike amphetamine abusers. Asked if there is an upper age limit for the use of psychostimulants in treating ADHD, the psychiatrist replied no.
"My oldest patient is 75 and I’ve been treating him for the last 15 years," he added.
Dr. Davies reported having no financial conflicts.
ESTES PARK, COLO. – Hands down, the most effective treatment for adult attention-deficit/hyperactivity disorder is psychostimulants.
The nonstimulant medications are a second-line alternative with less robust benefits, but they come in quite handy in selected situations, Dr. Robert D. Davies noted at a conference on internal medicine sponsored by the University of Colorado.
Also, a wealth of nonpharmacologic treatments are available. These include mindfulness exercises, cognitive behavioral therapy, life coaching, psychoeducational self-help audio books, and support groups.
"They’re great adjunct treatments, but in and of themselves not great solo treatments," according to Dr. Davies. "There’s an analogy to having poor near vision, so you never learned to read, and then suddenly you get glasses. That’s kind of like getting on medications: You still wouldn’t know how to read, but now you could learn how. So trying the nonpharmacologic interventions will be pretty frustrating for somebody who wants to avoid medications. You can try using those tools to help them with organization and those sorts of things, but it’s usually a huge struggle. Instead, put them on meds, teach them some of those things, and then see if off meds they can maintain those gains," advised Dr. Davies, a psychiatrist at the university.
A tip on self-help books geared to adults with attention-deficit/hyperactivity disorder (ADHD): "If you have a patient who’s never been able to get through a book in their life, don’t recommend a book that’s going to help them. ADHD folks do better with books on tape." Among the many on the market, Dr. Davies mentioned "Driven to Distraction" by Dr. Edward M. Hallowell and Dr. John J. Ratey as particularly good.
The psychostimulants fall into two categories: methylphenidate formulations and dextroamphetamine formulations. They’re equally effective, with the caveat that 20% of the population doesn’t respond to the methylphenidate drugs; however, they do respond to the dextroamphetamines. It’s a class effect, so when a patient isn’t doing well on a methylphenidate, don’t bother switching to a different methylphenidate drug; move on to a dextroamphetamine formulation.
Only four stimulants are approved by the Food and Drug Administration for adults: Adderal XR (dextroamphetamine/amphetamine), with a 9-hour duration of action and 15- to 30-mg dosage range; Focalin XR (dexmethylphenidate), with an 8- to 12-hour duration of action and dosage range of 20-40 mg; Vyvanse (lisdexamfetamine dimesylate), with a duration of 12 hours and dosing at 30-70 mg; and Concerta (methylphenidate extended-release), with a 12-hour duration of action and dosage range of 18-54 mg.
A history of drug abuse is a consideration in choosing a pharmacologic agent, but it isn’t necessarily a deal breaker in prescribing a stimulant. Some individuals with ADHD used stimulants or cocaine illicitly while students as a form of self-medication to enhance academic performance; they may be reasonable candidates for Concerta or Vyvanse, which have extremely low abuse potential. On the other hand, Dr. Davies recommended against prescribing stimulants for adult ADHD patients with a history of opiate or methamphetamine abuse.
Other situations where stimulant medications are best avoided include patients with medical conditions including heart disease, hypertension, and seizure disorders.
Only one nonstimulant medication is approved in adults: Strattera (atomoxetine). The reduction in ADHD symptoms is roughly 30% less than with stimulants. However, it is a once-daily drug, which is an advantage.
"When I’m treating anxiety or ADHD, especially in adults, a longer-acting drug is better. I always try to get patients away from that on-off phenomenon. That’s a feeling they don’t like," the psychiatrist continued.
Adults with ADHD may need pharmacologic assistance not only during a lengthy workday, but in the evening as well.
Nonstimulants that are sometimes used off-label in adults include Wellbutrin (bupropion), which is approved for children with ADHD. It is about half as effective as a stimulant medication. Effexor (venlafaxine) and Provigil (modafanil) are other nonstimulants used off-label; neither has been well studied in adult ADHD, according to Dr. Davies.
Adults with ADHD don’t develop tolerance to stimulant medications, unlike amphetamine abusers. Asked if there is an upper age limit for the use of psychostimulants in treating ADHD, the psychiatrist replied no.
"My oldest patient is 75 and I’ve been treating him for the last 15 years," he added.
Dr. Davies reported having no financial conflicts.
ESTES PARK, COLO. – Hands down, the most effective treatment for adult attention-deficit/hyperactivity disorder is psychostimulants.
The nonstimulant medications are a second-line alternative with less robust benefits, but they come in quite handy in selected situations, Dr. Robert D. Davies noted at a conference on internal medicine sponsored by the University of Colorado.
Also, a wealth of nonpharmacologic treatments are available. These include mindfulness exercises, cognitive behavioral therapy, life coaching, psychoeducational self-help audio books, and support groups.
"They’re great adjunct treatments, but in and of themselves not great solo treatments," according to Dr. Davies. "There’s an analogy to having poor near vision, so you never learned to read, and then suddenly you get glasses. That’s kind of like getting on medications: You still wouldn’t know how to read, but now you could learn how. So trying the nonpharmacologic interventions will be pretty frustrating for somebody who wants to avoid medications. You can try using those tools to help them with organization and those sorts of things, but it’s usually a huge struggle. Instead, put them on meds, teach them some of those things, and then see if off meds they can maintain those gains," advised Dr. Davies, a psychiatrist at the university.
A tip on self-help books geared to adults with attention-deficit/hyperactivity disorder (ADHD): "If you have a patient who’s never been able to get through a book in their life, don’t recommend a book that’s going to help them. ADHD folks do better with books on tape." Among the many on the market, Dr. Davies mentioned "Driven to Distraction" by Dr. Edward M. Hallowell and Dr. John J. Ratey as particularly good.
The psychostimulants fall into two categories: methylphenidate formulations and dextroamphetamine formulations. They’re equally effective, with the caveat that 20% of the population doesn’t respond to the methylphenidate drugs; however, they do respond to the dextroamphetamines. It’s a class effect, so when a patient isn’t doing well on a methylphenidate, don’t bother switching to a different methylphenidate drug; move on to a dextroamphetamine formulation.
Only four stimulants are approved by the Food and Drug Administration for adults: Adderal XR (dextroamphetamine/amphetamine), with a 9-hour duration of action and 15- to 30-mg dosage range; Focalin XR (dexmethylphenidate), with an 8- to 12-hour duration of action and dosage range of 20-40 mg; Vyvanse (lisdexamfetamine dimesylate), with a duration of 12 hours and dosing at 30-70 mg; and Concerta (methylphenidate extended-release), with a 12-hour duration of action and dosage range of 18-54 mg.
A history of drug abuse is a consideration in choosing a pharmacologic agent, but it isn’t necessarily a deal breaker in prescribing a stimulant. Some individuals with ADHD used stimulants or cocaine illicitly while students as a form of self-medication to enhance academic performance; they may be reasonable candidates for Concerta or Vyvanse, which have extremely low abuse potential. On the other hand, Dr. Davies recommended against prescribing stimulants for adult ADHD patients with a history of opiate or methamphetamine abuse.
Other situations where stimulant medications are best avoided include patients with medical conditions including heart disease, hypertension, and seizure disorders.
Only one nonstimulant medication is approved in adults: Strattera (atomoxetine). The reduction in ADHD symptoms is roughly 30% less than with stimulants. However, it is a once-daily drug, which is an advantage.
"When I’m treating anxiety or ADHD, especially in adults, a longer-acting drug is better. I always try to get patients away from that on-off phenomenon. That’s a feeling they don’t like," the psychiatrist continued.
Adults with ADHD may need pharmacologic assistance not only during a lengthy workday, but in the evening as well.
Nonstimulants that are sometimes used off-label in adults include Wellbutrin (bupropion), which is approved for children with ADHD. It is about half as effective as a stimulant medication. Effexor (venlafaxine) and Provigil (modafanil) are other nonstimulants used off-label; neither has been well studied in adult ADHD, according to Dr. Davies.
Adults with ADHD don’t develop tolerance to stimulant medications, unlike amphetamine abusers. Asked if there is an upper age limit for the use of psychostimulants in treating ADHD, the psychiatrist replied no.
"My oldest patient is 75 and I’ve been treating him for the last 15 years," he added.
Dr. Davies reported having no financial conflicts.
EXPERT ANALYSIS FROM THE ANNUAL INTERNAL MEDICINE PROGRAM
Trochanteric bursitis: Easily misdiagnosed, readily treatable
ESTES PARK, COLO. – Trochanteric bursitis is an often overlooked cause of hip pain that’s sometimes so severe it can mimic a septic hip.
This overuse syndrome, common among weekend warriors, is also often mistaken for lumbar radiculopathy. The distinction is this: The pseudoradiculopathy of trochanteric bursitis doesn’t extend below the knee, while lumbar radiculopathy with sciatica typically goes past the knee laterally and runs down the leg, often as far as the foot, Dr. Robert W. Janson said at a conference on internal medicine sponsored by the University of Colorado.
Patients with trochanteric bursitis report pain over the trochanteric area and lateral thigh. This lateral hip pain is accentuated by walking, climbing stairs, or sitting in a deep chair. Patients report discomfort sleeping on the affected side. The range of motion in the hip joint is normal, but there is local point tenderness over the greater tuberosity that is exacerbated with external rotation of the hip and hip abduction against resistance.
"It just takes a second. Feel the greater tuberosity. You push in there, and they respond with the positive chandelier sign," the rheumatologist said, using a term for a pain response so sudden and electrifying that the patient figuratively rises up off the examination table and grabs for the ceiling lights.
The etiology of trochanteric bursitis is often a gait abnormality from a leg-length discrepancy. A difference of 2 cm or more is deemed clinically significant. The two static anatomic landmarks used in measuring leg-length discrepancy are the anterior superior iliac spine located right under the belt line and the medial malleolus.
"We’re concerned if the difference between the two legs is more than 2 cm. We typically work with a podiatrist to give the patient an insert or shoe lift. Remember, if you have a 2-cm leg-length discrepancy, you don’t replace all 2 cm. The podiatrist will start at one-eighth or one-quarter of an inch and work up as tolerated," according to Dr. Janson, chief of the rheumatology section at the Denver Veterans Affairs Medical Center.
Other common causes of trochanteric bursitis include osteoarthritis of the hip or lumbosacral spine, scoliosis, or a pathologically tight tensor fascia latae caused by running. This common running overuse injury entails tightness of the iliotibial band, with resultant inflammation of the bursa from repeated snapping of the shortened band over the greater tuberosity.
Treatment, beyond correction of any biomechanical causes, involves the usual general measures employed in overuse injuries: rest, with possible partial weight bearing; ice; full-anti-inflammatory-dose NSAIDs for at least several weeks; and physical therapy directed at stretching the gluteus medius and a possibly tight iliotibial band.
A local injection of 10-20 mg of long-acting methylprednisolone mixed with a few milliliters of lidocaine will bring much-appreciated symptomatic relief.
"The greater tuberosity is about the size of a silver dollar. When you inject the bursa, mark the greater tuberosity and go straight down the center as the patient lies laterally. A few seconds spent palpating that area and outlining the greater tuberosity can really be beneficial for your steroid injection," Dr. Janson commented.
Use a long needle, and bear in mind a time-honored rheumatologic pearl: "All injections in rheumatology should flow easily. If you find you’re against resistance, you’re in the wrong place," according to Dr. Janson.
He reported having no financial conflicts.
ESTES PARK, COLO. – Trochanteric bursitis is an often overlooked cause of hip pain that’s sometimes so severe it can mimic a septic hip.
This overuse syndrome, common among weekend warriors, is also often mistaken for lumbar radiculopathy. The distinction is this: The pseudoradiculopathy of trochanteric bursitis doesn’t extend below the knee, while lumbar radiculopathy with sciatica typically goes past the knee laterally and runs down the leg, often as far as the foot, Dr. Robert W. Janson said at a conference on internal medicine sponsored by the University of Colorado.
Patients with trochanteric bursitis report pain over the trochanteric area and lateral thigh. This lateral hip pain is accentuated by walking, climbing stairs, or sitting in a deep chair. Patients report discomfort sleeping on the affected side. The range of motion in the hip joint is normal, but there is local point tenderness over the greater tuberosity that is exacerbated with external rotation of the hip and hip abduction against resistance.
"It just takes a second. Feel the greater tuberosity. You push in there, and they respond with the positive chandelier sign," the rheumatologist said, using a term for a pain response so sudden and electrifying that the patient figuratively rises up off the examination table and grabs for the ceiling lights.
The etiology of trochanteric bursitis is often a gait abnormality from a leg-length discrepancy. A difference of 2 cm or more is deemed clinically significant. The two static anatomic landmarks used in measuring leg-length discrepancy are the anterior superior iliac spine located right under the belt line and the medial malleolus.
"We’re concerned if the difference between the two legs is more than 2 cm. We typically work with a podiatrist to give the patient an insert or shoe lift. Remember, if you have a 2-cm leg-length discrepancy, you don’t replace all 2 cm. The podiatrist will start at one-eighth or one-quarter of an inch and work up as tolerated," according to Dr. Janson, chief of the rheumatology section at the Denver Veterans Affairs Medical Center.
Other common causes of trochanteric bursitis include osteoarthritis of the hip or lumbosacral spine, scoliosis, or a pathologically tight tensor fascia latae caused by running. This common running overuse injury entails tightness of the iliotibial band, with resultant inflammation of the bursa from repeated snapping of the shortened band over the greater tuberosity.
Treatment, beyond correction of any biomechanical causes, involves the usual general measures employed in overuse injuries: rest, with possible partial weight bearing; ice; full-anti-inflammatory-dose NSAIDs for at least several weeks; and physical therapy directed at stretching the gluteus medius and a possibly tight iliotibial band.
A local injection of 10-20 mg of long-acting methylprednisolone mixed with a few milliliters of lidocaine will bring much-appreciated symptomatic relief.
"The greater tuberosity is about the size of a silver dollar. When you inject the bursa, mark the greater tuberosity and go straight down the center as the patient lies laterally. A few seconds spent palpating that area and outlining the greater tuberosity can really be beneficial for your steroid injection," Dr. Janson commented.
Use a long needle, and bear in mind a time-honored rheumatologic pearl: "All injections in rheumatology should flow easily. If you find you’re against resistance, you’re in the wrong place," according to Dr. Janson.
He reported having no financial conflicts.
ESTES PARK, COLO. – Trochanteric bursitis is an often overlooked cause of hip pain that’s sometimes so severe it can mimic a septic hip.
This overuse syndrome, common among weekend warriors, is also often mistaken for lumbar radiculopathy. The distinction is this: The pseudoradiculopathy of trochanteric bursitis doesn’t extend below the knee, while lumbar radiculopathy with sciatica typically goes past the knee laterally and runs down the leg, often as far as the foot, Dr. Robert W. Janson said at a conference on internal medicine sponsored by the University of Colorado.
Patients with trochanteric bursitis report pain over the trochanteric area and lateral thigh. This lateral hip pain is accentuated by walking, climbing stairs, or sitting in a deep chair. Patients report discomfort sleeping on the affected side. The range of motion in the hip joint is normal, but there is local point tenderness over the greater tuberosity that is exacerbated with external rotation of the hip and hip abduction against resistance.
"It just takes a second. Feel the greater tuberosity. You push in there, and they respond with the positive chandelier sign," the rheumatologist said, using a term for a pain response so sudden and electrifying that the patient figuratively rises up off the examination table and grabs for the ceiling lights.
The etiology of trochanteric bursitis is often a gait abnormality from a leg-length discrepancy. A difference of 2 cm or more is deemed clinically significant. The two static anatomic landmarks used in measuring leg-length discrepancy are the anterior superior iliac spine located right under the belt line and the medial malleolus.
"We’re concerned if the difference between the two legs is more than 2 cm. We typically work with a podiatrist to give the patient an insert or shoe lift. Remember, if you have a 2-cm leg-length discrepancy, you don’t replace all 2 cm. The podiatrist will start at one-eighth or one-quarter of an inch and work up as tolerated," according to Dr. Janson, chief of the rheumatology section at the Denver Veterans Affairs Medical Center.
Other common causes of trochanteric bursitis include osteoarthritis of the hip or lumbosacral spine, scoliosis, or a pathologically tight tensor fascia latae caused by running. This common running overuse injury entails tightness of the iliotibial band, with resultant inflammation of the bursa from repeated snapping of the shortened band over the greater tuberosity.
Treatment, beyond correction of any biomechanical causes, involves the usual general measures employed in overuse injuries: rest, with possible partial weight bearing; ice; full-anti-inflammatory-dose NSAIDs for at least several weeks; and physical therapy directed at stretching the gluteus medius and a possibly tight iliotibial band.
A local injection of 10-20 mg of long-acting methylprednisolone mixed with a few milliliters of lidocaine will bring much-appreciated symptomatic relief.
"The greater tuberosity is about the size of a silver dollar. When you inject the bursa, mark the greater tuberosity and go straight down the center as the patient lies laterally. A few seconds spent palpating that area and outlining the greater tuberosity can really be beneficial for your steroid injection," Dr. Janson commented.
Use a long needle, and bear in mind a time-honored rheumatologic pearl: "All injections in rheumatology should flow easily. If you find you’re against resistance, you’re in the wrong place," according to Dr. Janson.
He reported having no financial conflicts.
EXPERT ANALYSIS FROM THE ANNUAL INTERNAL MEDICINE PROGRAM
Trochanteric bursitis: Easily misdiagnosed, readily treatable
ESTES PARK, COLO. – Trochanteric bursitis is an often overlooked cause of hip pain that’s sometimes so severe it can mimic a septic hip.
This overuse syndrome, common among weekend warriors, is also often mistaken for lumbar radiculopathy. The distinction is this: The pseudoradiculopathy of trochanteric bursitis doesn’t extend below the knee, while lumbar radiculopathy with sciatica typically goes past the knee laterally and runs down the leg, often as far as the foot, Dr. Robert W. Janson said at a conference on internal medicine sponsored by the University of Colorado.
Patients with trochanteric bursitis report pain over the trochanteric area and lateral thigh. This lateral hip pain is accentuated by walking, climbing stairs, or sitting in a deep chair. Patients report discomfort sleeping on the affected side. The range of motion in the hip joint is normal, but there is local point tenderness over the greater tuberosity that is exacerbated with external rotation of the hip and hip abduction against resistance.
"It just takes a second. Feel the greater tuberosity. You push in there, and they respond with the positive chandelier sign," the rheumatologist said, using a term for a pain response so sudden and electrifying that the patient figuratively rises up off the examination table and grabs for the ceiling lights.
The etiology of trochanteric bursitis is often a gait abnormality from a leg-length discrepancy. A difference of 2 cm or more is deemed clinically significant. The two static anatomic landmarks used in measuring leg-length discrepancy are the anterior superior iliac spine located right under the belt line and the medial malleolus.
"We’re concerned if the difference between the two legs is more than 2 cm. We typically work with a podiatrist to give the patient an insert or shoe lift. Remember, if you have a 2-cm leg-length discrepancy, you don’t replace all 2 cm. The podiatrist will start at one-eighth or one-quarter of an inch and work up as tolerated," according to Dr. Janson, chief of the rheumatology section at the Denver Veterans Affairs Medical Center.
Other common causes of trochanteric bursitis include osteoarthritis of the hip or lumbosacral spine, scoliosis, or a pathologically tight tensor fascia latae caused by running. This common running overuse injury entails tightness of the iliotibial band, with resultant inflammation of the bursa from repeated snapping of the shortened band over the greater tuberosity.
Treatment, beyond correction of any biomechanical causes, involves the usual general measures employed in overuse injuries: rest, with possible partial weight bearing; ice; full-anti-inflammatory-dose NSAIDs for at least several weeks; and physical therapy directed at stretching the gluteus medius and a possibly tight iliotibial band.
A local injection of 10-20 mg of long-acting methylprednisolone mixed with a few milliliters of lidocaine will bring much-appreciated symptomatic relief.
"The greater tuberosity is about the size of a silver dollar. When you inject the bursa, mark the greater tuberosity and go straight down the center as the patient lies laterally. A few seconds spent palpating that area and outlining the greater tuberosity can really be beneficial for your steroid injection," Dr. Janson commented.
Use a long needle, and bear in mind a time-honored rheumatologic pearl: "All injections in rheumatology should flow easily. If you find you’re against resistance, you’re in the wrong place," according to Dr. Janson.
He reported having no financial conflicts.
ESTES PARK, COLO. – Trochanteric bursitis is an often overlooked cause of hip pain that’s sometimes so severe it can mimic a septic hip.
This overuse syndrome, common among weekend warriors, is also often mistaken for lumbar radiculopathy. The distinction is this: The pseudoradiculopathy of trochanteric bursitis doesn’t extend below the knee, while lumbar radiculopathy with sciatica typically goes past the knee laterally and runs down the leg, often as far as the foot, Dr. Robert W. Janson said at a conference on internal medicine sponsored by the University of Colorado.
Patients with trochanteric bursitis report pain over the trochanteric area and lateral thigh. This lateral hip pain is accentuated by walking, climbing stairs, or sitting in a deep chair. Patients report discomfort sleeping on the affected side. The range of motion in the hip joint is normal, but there is local point tenderness over the greater tuberosity that is exacerbated with external rotation of the hip and hip abduction against resistance.
"It just takes a second. Feel the greater tuberosity. You push in there, and they respond with the positive chandelier sign," the rheumatologist said, using a term for a pain response so sudden and electrifying that the patient figuratively rises up off the examination table and grabs for the ceiling lights.
The etiology of trochanteric bursitis is often a gait abnormality from a leg-length discrepancy. A difference of 2 cm or more is deemed clinically significant. The two static anatomic landmarks used in measuring leg-length discrepancy are the anterior superior iliac spine located right under the belt line and the medial malleolus.
"We’re concerned if the difference between the two legs is more than 2 cm. We typically work with a podiatrist to give the patient an insert or shoe lift. Remember, if you have a 2-cm leg-length discrepancy, you don’t replace all 2 cm. The podiatrist will start at one-eighth or one-quarter of an inch and work up as tolerated," according to Dr. Janson, chief of the rheumatology section at the Denver Veterans Affairs Medical Center.
Other common causes of trochanteric bursitis include osteoarthritis of the hip or lumbosacral spine, scoliosis, or a pathologically tight tensor fascia latae caused by running. This common running overuse injury entails tightness of the iliotibial band, with resultant inflammation of the bursa from repeated snapping of the shortened band over the greater tuberosity.
Treatment, beyond correction of any biomechanical causes, involves the usual general measures employed in overuse injuries: rest, with possible partial weight bearing; ice; full-anti-inflammatory-dose NSAIDs for at least several weeks; and physical therapy directed at stretching the gluteus medius and a possibly tight iliotibial band.
A local injection of 10-20 mg of long-acting methylprednisolone mixed with a few milliliters of lidocaine will bring much-appreciated symptomatic relief.
"The greater tuberosity is about the size of a silver dollar. When you inject the bursa, mark the greater tuberosity and go straight down the center as the patient lies laterally. A few seconds spent palpating that area and outlining the greater tuberosity can really be beneficial for your steroid injection," Dr. Janson commented.
Use a long needle, and bear in mind a time-honored rheumatologic pearl: "All injections in rheumatology should flow easily. If you find you’re against resistance, you’re in the wrong place," according to Dr. Janson.
He reported having no financial conflicts.
ESTES PARK, COLO. – Trochanteric bursitis is an often overlooked cause of hip pain that’s sometimes so severe it can mimic a septic hip.
This overuse syndrome, common among weekend warriors, is also often mistaken for lumbar radiculopathy. The distinction is this: The pseudoradiculopathy of trochanteric bursitis doesn’t extend below the knee, while lumbar radiculopathy with sciatica typically goes past the knee laterally and runs down the leg, often as far as the foot, Dr. Robert W. Janson said at a conference on internal medicine sponsored by the University of Colorado.
Patients with trochanteric bursitis report pain over the trochanteric area and lateral thigh. This lateral hip pain is accentuated by walking, climbing stairs, or sitting in a deep chair. Patients report discomfort sleeping on the affected side. The range of motion in the hip joint is normal, but there is local point tenderness over the greater tuberosity that is exacerbated with external rotation of the hip and hip abduction against resistance.
"It just takes a second. Feel the greater tuberosity. You push in there, and they respond with the positive chandelier sign," the rheumatologist said, using a term for a pain response so sudden and electrifying that the patient figuratively rises up off the examination table and grabs for the ceiling lights.
The etiology of trochanteric bursitis is often a gait abnormality from a leg-length discrepancy. A difference of 2 cm or more is deemed clinically significant. The two static anatomic landmarks used in measuring leg-length discrepancy are the anterior superior iliac spine located right under the belt line and the medial malleolus.
"We’re concerned if the difference between the two legs is more than 2 cm. We typically work with a podiatrist to give the patient an insert or shoe lift. Remember, if you have a 2-cm leg-length discrepancy, you don’t replace all 2 cm. The podiatrist will start at one-eighth or one-quarter of an inch and work up as tolerated," according to Dr. Janson, chief of the rheumatology section at the Denver Veterans Affairs Medical Center.
Other common causes of trochanteric bursitis include osteoarthritis of the hip or lumbosacral spine, scoliosis, or a pathologically tight tensor fascia latae caused by running. This common running overuse injury entails tightness of the iliotibial band, with resultant inflammation of the bursa from repeated snapping of the shortened band over the greater tuberosity.
Treatment, beyond correction of any biomechanical causes, involves the usual general measures employed in overuse injuries: rest, with possible partial weight bearing; ice; full-anti-inflammatory-dose NSAIDs for at least several weeks; and physical therapy directed at stretching the gluteus medius and a possibly tight iliotibial band.
A local injection of 10-20 mg of long-acting methylprednisolone mixed with a few milliliters of lidocaine will bring much-appreciated symptomatic relief.
"The greater tuberosity is about the size of a silver dollar. When you inject the bursa, mark the greater tuberosity and go straight down the center as the patient lies laterally. A few seconds spent palpating that area and outlining the greater tuberosity can really be beneficial for your steroid injection," Dr. Janson commented.
Use a long needle, and bear in mind a time-honored rheumatologic pearl: "All injections in rheumatology should flow easily. If you find you’re against resistance, you’re in the wrong place," according to Dr. Janson.
He reported having no financial conflicts.
EXPERT ANALYSIS FROM THE ANNUAL INTERNAL MEDICINE PROGRAM
Adult ADHD: Making the diagnosis
ESTES PARK, COLO. – Adult attention-deficit/hyperactivity disorder is a common and treatable psychiatric condition the diagnosis of which is made more challenging because the disorder looks different than the classic picture in children.
Trying to apply the Diagnostic and Statistical Manual of Mental Disorders diagnostic criteria for attention-deficit/hyperactivity disorder (ADHD) to adults is problematic. The DSM-IV symptoms focus mainly on childhood activities, particularly school and play. Plus, hyperactivity – the most recognizable symptom of ADHD in childhood – tends to diminish with age, becoming a more subjective experience of internal restlessness, Dr. Robert D. Davies explained at a conference on internal medicine sponsored by the University of Colorado.
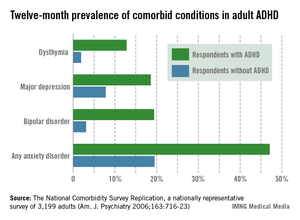
Yet ADHD by definition always first develops in childhood, even if an affected adult hasn’t previously been diagnosed and doesn’t recall the early impairment.
"Very often patients first present in adulthood because things have changed in their life, but if you go back and look carefully, it has been there since childhood. If you have a patient who comes in saying, ‘In the last few years all of a sudden I can’t concentrate, I can’t focus, I’m not doing well at work’ and there’s never been any hint of that before, I don’t know what it is, but it’s not ADHD," declared Dr. Davies, a psychiatrist at the university.
The adult presentation of ADHD is more subtle than in children. It includes disorganization and poor time-management skills; impulsivity with poor self-control often demonstrated via rude comments and frequent interruption of others; emotional difficulties rooted in low self-esteem and poor affect regulation; and difficulty in concentrating and completing even simple tasks.
"Adults with ADHD make great salespeople. They can really close the sale. But I’ve had so many salespeople I’ve treated who are failing at work because they never get the paperwork in and actually file the order. They don’t follow up on those things, but they’re great at the beginning," he observed.
The hyperactivity component can look much like mania: thrill seeking, racing thoughts, excessive talking, and difficulty in falling asleep.
All these adult ADHD symptoms add up to increased risks of divorce, difficulties at work, substance abuse, incarceration, a poor driving history – "lots of fender benders," according to Dr. Davies – and high rates of comorbid depression and anxiety that have been well documented in a landmark national study sponsored by the National Institute of Mental Health. The study, the National Comorbidity Survey Replication, placed the prevalence of adult ADHD among the general population at 4.4% (see accompanying graphic).
Substance abuse, hearing loss, and hyperthyroidism need to be ruled out before arriving at the diagnosis of adult ADHD. More challenging is to sort out adult ADHD from several commonly comorbid psychiatric conditions, most notably bipolar disorder, generalized anxiety disorder, and personality disorder.
The patient’s sleep pattern can provide useful information in this regard. Adult ADHD is characterized by a phase shift: The internal hyperactivity leads to difficulty in falling asleep until quite late, with subsequent trouble in waking up in the morning. In contrast, the manic phase of bipolar disorder is marked by a decreased sleep requirement. Patients with generalized anxiety disorder, unlike those with bipolar mania, really need their sleep, but their difficulty in falling asleep stems from worries about what might happen in the future. Individuals with adult ADHD typically can’t sleep because they’re ruminating about mistakes they’ve made.
"They’re worried about things that are real: what they forgot to do, who they’ve offended. In contrast, anytime you’re talking to a patient and they’re saying a lot of ‘what ifs,’ that’s a clue that the problem is generalized anxiety disorder," he explained.
While ADHD is a lifelong condition that begins in childhood, bipolar disorder is episodic and starts in the late teen years or later.
As for the differential between adult ADHD and borderline personality disorder, patients with ADHD typically have a sense of self as being harmed by their own failures and shortcomings coupled with the negative way others perceive them. In contrast, individuals with personality disorders often don’t have any real sense of self. The chaotic life that figures so prominently in the personal histories of many patients with adult ADHD dates back to childhood and results from their impulsivity and inattention, whereas the chaotic life of the patient with borderline personality disorder often starts in adolescence and is the result of their poor interpersonal relationships and rigid thinking.
Lots of adults are coming to the offices of primary care physicians and psychiatrists seeking help for what they believe is ADHD, brandishing their scores on self-report screening scales they find in popular magazines. Dr. Davies advises not attaching much weight to the self-report scales.
"I don’t use them routinely," he said. "If you think about the symptoms of ADHD, especially the ones that come out of magazines that they’re going to bring in to you, almost everybody at some point is going to fill these criteria. You want to ask people about those big, core ADHD symptoms: Are they really causing problems in your life?"
Dr. Davies acknowledged that adult ADHD is a disorder surrounded by considerable professional skepticism, even though the prevalence, serious consequences, and treatment responsiveness of adult ADHD are now well established.
"It’s a very controversial area outside of psychiatry but also inside psychiatry," according to Dr. Davies. "A psychiatric colleague of mine had diagnosed an adult patient with ADHD and then wanted to refer him to me. I asked why. He said, ‘Because I don’t believe in it.’"
Dr. Davies reported having no financial conflicts.
ESTES PARK, COLO. – Adult attention-deficit/hyperactivity disorder is a common and treatable psychiatric condition the diagnosis of which is made more challenging because the disorder looks different than the classic picture in children.
Trying to apply the Diagnostic and Statistical Manual of Mental Disorders diagnostic criteria for attention-deficit/hyperactivity disorder (ADHD) to adults is problematic. The DSM-IV symptoms focus mainly on childhood activities, particularly school and play. Plus, hyperactivity – the most recognizable symptom of ADHD in childhood – tends to diminish with age, becoming a more subjective experience of internal restlessness, Dr. Robert D. Davies explained at a conference on internal medicine sponsored by the University of Colorado.
Yet ADHD by definition always first develops in childhood, even if an affected adult hasn’t previously been diagnosed and doesn’t recall the early impairment.
"Very often patients first present in adulthood because things have changed in their life, but if you go back and look carefully, it has been there since childhood. If you have a patient who comes in saying, ‘In the last few years all of a sudden I can’t concentrate, I can’t focus, I’m not doing well at work’ and there’s never been any hint of that before, I don’t know what it is, but it’s not ADHD," declared Dr. Davies, a psychiatrist at the university.
The adult presentation of ADHD is more subtle than in children. It includes disorganization and poor time-management skills; impulsivity with poor self-control often demonstrated via rude comments and frequent interruption of others; emotional difficulties rooted in low self-esteem and poor affect regulation; and difficulty in concentrating and completing even simple tasks.
"Adults with ADHD make great salespeople. They can really close the sale. But I’ve had so many salespeople I’ve treated who are failing at work because they never get the paperwork in and actually file the order. They don’t follow up on those things, but they’re great at the beginning," he observed.
The hyperactivity component can look much like mania: thrill seeking, racing thoughts, excessive talking, and difficulty in falling asleep.
All these adult ADHD symptoms add up to increased risks of divorce, difficulties at work, substance abuse, incarceration, a poor driving history – "lots of fender benders," according to Dr. Davies – and high rates of comorbid depression and anxiety that have been well documented in a landmark national study sponsored by the National Institute of Mental Health. The study, the National Comorbidity Survey Replication, placed the prevalence of adult ADHD among the general population at 4.4% (see accompanying graphic).
Substance abuse, hearing loss, and hyperthyroidism need to be ruled out before arriving at the diagnosis of adult ADHD. More challenging is to sort out adult ADHD from several commonly comorbid psychiatric conditions, most notably bipolar disorder, generalized anxiety disorder, and personality disorder.
The patient’s sleep pattern can provide useful information in this regard. Adult ADHD is characterized by a phase shift: The internal hyperactivity leads to difficulty in falling asleep until quite late, with subsequent trouble in waking up in the morning. In contrast, the manic phase of bipolar disorder is marked by a decreased sleep requirement. Patients with generalized anxiety disorder, unlike those with bipolar mania, really need their sleep, but their difficulty in falling asleep stems from worries about what might happen in the future. Individuals with adult ADHD typically can’t sleep because they’re ruminating about mistakes they’ve made.
"They’re worried about things that are real: what they forgot to do, who they’ve offended. In contrast, anytime you’re talking to a patient and they’re saying a lot of ‘what ifs,’ that’s a clue that the problem is generalized anxiety disorder," he explained.
While ADHD is a lifelong condition that begins in childhood, bipolar disorder is episodic and starts in the late teen years or later.
As for the differential between adult ADHD and borderline personality disorder, patients with ADHD typically have a sense of self as being harmed by their own failures and shortcomings coupled with the negative way others perceive them. In contrast, individuals with personality disorders often don’t have any real sense of self. The chaotic life that figures so prominently in the personal histories of many patients with adult ADHD dates back to childhood and results from their impulsivity and inattention, whereas the chaotic life of the patient with borderline personality disorder often starts in adolescence and is the result of their poor interpersonal relationships and rigid thinking.
Lots of adults are coming to the offices of primary care physicians and psychiatrists seeking help for what they believe is ADHD, brandishing their scores on self-report screening scales they find in popular magazines. Dr. Davies advises not attaching much weight to the self-report scales.
"I don’t use them routinely," he said. "If you think about the symptoms of ADHD, especially the ones that come out of magazines that they’re going to bring in to you, almost everybody at some point is going to fill these criteria. You want to ask people about those big, core ADHD symptoms: Are they really causing problems in your life?"
Dr. Davies acknowledged that adult ADHD is a disorder surrounded by considerable professional skepticism, even though the prevalence, serious consequences, and treatment responsiveness of adult ADHD are now well established.
"It’s a very controversial area outside of psychiatry but also inside psychiatry," according to Dr. Davies. "A psychiatric colleague of mine had diagnosed an adult patient with ADHD and then wanted to refer him to me. I asked why. He said, ‘Because I don’t believe in it.’"
Dr. Davies reported having no financial conflicts.
ESTES PARK, COLO. – Adult attention-deficit/hyperactivity disorder is a common and treatable psychiatric condition the diagnosis of which is made more challenging because the disorder looks different than the classic picture in children.
Trying to apply the Diagnostic and Statistical Manual of Mental Disorders diagnostic criteria for attention-deficit/hyperactivity disorder (ADHD) to adults is problematic. The DSM-IV symptoms focus mainly on childhood activities, particularly school and play. Plus, hyperactivity – the most recognizable symptom of ADHD in childhood – tends to diminish with age, becoming a more subjective experience of internal restlessness, Dr. Robert D. Davies explained at a conference on internal medicine sponsored by the University of Colorado.
Yet ADHD by definition always first develops in childhood, even if an affected adult hasn’t previously been diagnosed and doesn’t recall the early impairment.
"Very often patients first present in adulthood because things have changed in their life, but if you go back and look carefully, it has been there since childhood. If you have a patient who comes in saying, ‘In the last few years all of a sudden I can’t concentrate, I can’t focus, I’m not doing well at work’ and there’s never been any hint of that before, I don’t know what it is, but it’s not ADHD," declared Dr. Davies, a psychiatrist at the university.
The adult presentation of ADHD is more subtle than in children. It includes disorganization and poor time-management skills; impulsivity with poor self-control often demonstrated via rude comments and frequent interruption of others; emotional difficulties rooted in low self-esteem and poor affect regulation; and difficulty in concentrating and completing even simple tasks.
"Adults with ADHD make great salespeople. They can really close the sale. But I’ve had so many salespeople I’ve treated who are failing at work because they never get the paperwork in and actually file the order. They don’t follow up on those things, but they’re great at the beginning," he observed.
The hyperactivity component can look much like mania: thrill seeking, racing thoughts, excessive talking, and difficulty in falling asleep.
All these adult ADHD symptoms add up to increased risks of divorce, difficulties at work, substance abuse, incarceration, a poor driving history – "lots of fender benders," according to Dr. Davies – and high rates of comorbid depression and anxiety that have been well documented in a landmark national study sponsored by the National Institute of Mental Health. The study, the National Comorbidity Survey Replication, placed the prevalence of adult ADHD among the general population at 4.4% (see accompanying graphic).
Substance abuse, hearing loss, and hyperthyroidism need to be ruled out before arriving at the diagnosis of adult ADHD. More challenging is to sort out adult ADHD from several commonly comorbid psychiatric conditions, most notably bipolar disorder, generalized anxiety disorder, and personality disorder.
The patient’s sleep pattern can provide useful information in this regard. Adult ADHD is characterized by a phase shift: The internal hyperactivity leads to difficulty in falling asleep until quite late, with subsequent trouble in waking up in the morning. In contrast, the manic phase of bipolar disorder is marked by a decreased sleep requirement. Patients with generalized anxiety disorder, unlike those with bipolar mania, really need their sleep, but their difficulty in falling asleep stems from worries about what might happen in the future. Individuals with adult ADHD typically can’t sleep because they’re ruminating about mistakes they’ve made.
"They’re worried about things that are real: what they forgot to do, who they’ve offended. In contrast, anytime you’re talking to a patient and they’re saying a lot of ‘what ifs,’ that’s a clue that the problem is generalized anxiety disorder," he explained.
While ADHD is a lifelong condition that begins in childhood, bipolar disorder is episodic and starts in the late teen years or later.
As for the differential between adult ADHD and borderline personality disorder, patients with ADHD typically have a sense of self as being harmed by their own failures and shortcomings coupled with the negative way others perceive them. In contrast, individuals with personality disorders often don’t have any real sense of self. The chaotic life that figures so prominently in the personal histories of many patients with adult ADHD dates back to childhood and results from their impulsivity and inattention, whereas the chaotic life of the patient with borderline personality disorder often starts in adolescence and is the result of their poor interpersonal relationships and rigid thinking.
Lots of adults are coming to the offices of primary care physicians and psychiatrists seeking help for what they believe is ADHD, brandishing their scores on self-report screening scales they find in popular magazines. Dr. Davies advises not attaching much weight to the self-report scales.
"I don’t use them routinely," he said. "If you think about the symptoms of ADHD, especially the ones that come out of magazines that they’re going to bring in to you, almost everybody at some point is going to fill these criteria. You want to ask people about those big, core ADHD symptoms: Are they really causing problems in your life?"
Dr. Davies acknowledged that adult ADHD is a disorder surrounded by considerable professional skepticism, even though the prevalence, serious consequences, and treatment responsiveness of adult ADHD are now well established.
"It’s a very controversial area outside of psychiatry but also inside psychiatry," according to Dr. Davies. "A psychiatric colleague of mine had diagnosed an adult patient with ADHD and then wanted to refer him to me. I asked why. He said, ‘Because I don’t believe in it.’"
Dr. Davies reported having no financial conflicts.
AT THE ANNUAL INTERNAL MEDICINE PROGRAM
Think ‘ceftaroline’ in suspected drug-resistant CAP
ESTES PARK, COLO. – For primary care physicians, ceftaroline is hands-down the most exciting and important of the four systemic antibacterial agents to reach the U.S. market since the great 7-year drought in approvals ended in 2008, an infectious disease expert observed.
Ceftaroline (Teflaro) is a novel cephalosporin with unique binding to penicillin-binding proteins, including the altered versions that confer resistance in methicillin-resistant Staphylococcus aureus and penicillin- and cephalosporin-resistant Streptococcus pneumoniae. Thus, ceftaroline is a potent and effective drug in the increasingly common situation of beta-lactam-resistant community-acquired pneumonia (CAP) or complicated skin and soft tissue infections, noted Dr. Mary T. Bessesen, chief of the infectious diseases section at Denver V.A. Medical Center.
In the pivotal FOCUS 1 and FOCUS 2 trials conducted in patients with CAP not due to MRSA, ceftaroline proved noninferior overall to ceftriaxone (Rocephin). Of note, in the 14% of FOCUS participants with CAP due to S. aureus, ceftaroline proved to be significantly more effective than ceftriaxone. Importantly, the same was true among the one-third of FOCUS participants in whom S. pneumoniae was isolated (Clin. Infect. Dis. 2010;51:1395-405).
"I think if you’re going to impact mortality in CAP, pneumococcus has to be the primary target. Ceftaroline is a good alternative when penicillin-resistant S. pneumoniae is suspected or proven," Dr. Bessesen said at a conference on internal medicine sponsored by the University of Colorado.
Other common pathogens in CAP that are sensitive to ceftaroline are Hemophilus influenza and Moraxella catarrhalis. The Gram-negative pathogens E. coli, Klebsiella pneumoniae, and Enterobacter cloacae are also ceftaroline sensitive, with activity similar to ceftriaxone and ceftazidime (Fortaz).
Not only is MRSA sensitive to ceftaroline, so are methicillin-sensitive S. aureus, vancomycin-intermediate S. aureus, vancomycin-resistant S. aureus, linezolid (Zyvox)-resistant S. aureus, and daptomycin (Cubicin)-nonsusceptible S. aureus.
Ceftaroline does not cover the atypical pneumonia pathogens Mycoplasma pneumoniae, Chlamydia pneumoniae, and Legionella pneumoniae, nor does it cover Pseudomonas aeruginosa or extended-spectrum beta-lactamase-producing Enterobacteriaceae, stressed Dr. Bessesen.
The current CAP guidelines don’t include recommendations for ceftaroline, because the drug received Food and Drug Administration approval for treatment of CAP and complicated skin and soft tissue infections after the guidelines were issued.
Clinical trials investigating ceftaroline in CAP caused by MRSA would be welcome, Dr. Bessesen noted, because the current CAP guidelines don’t include any recommendations for CAP pneumonia.
"It really leaves us wondering in high-risk cases what’s best to do," she said. "There’s been some controversy about vancomycin versus linezolid when you suspect MRSA pneumonia. Ceftaroline would be a nice way to get around all of that."
Ceftaroline is administered intravenously twice daily, with dose adjustment for renal function. The drug’s pharmacokinetics are favorable for intramuscular injection, but there are limited clinical data for this route, and it is not FDA approved.
Ceftaroline costs about $84 per day, or four times more than ceftriaxone, Dr. Bessesen said. As a result, formulary committees are reluctant to put ceftaroline on the list.
That makes Dr. Bessesen see red.
"I’ve never been on a drug company speakers bureau. I’ve never had any research money from drug companies. I speak only as someone who’s interested in us being able to continue to treat bacterial infections when I say we’ve got to change our attitude. We have to be willing to pay something for these antibiotics," she asserted.
The antibiotic development pipeline has failed as pharmaceutical companies have abandoned the field, Dr. Bessesen continued. There are three reasons for this. One is that all the easy drugs have already been discovered. Another is that the FDA regulatory approval system for antibacterial agents is seriously outdated; the European Medicines Agency is much more forward thinking in this area and would be a useful model for FDA modernization, she noted.
But the biggest reason for the broken pipeline is that antibiotics are not a good financial investment for pharmaceutical companies. "It’s much more profitable for them to develop a drug like lovastatin that you’re going to take every day for the rest of your life than to develop an antibiotic you’re going to prescribe for a week or two. And society expects antibiotics to be cheap," Dr. Bessesen observed.
Contrast the roughly $1,600 cost of 4 weeks of ceftriaxone for S. viridans endocarditis – a serious infection – with the $54,000 price tag for 1 year of trastuzumab for breast cancer or $240,000 for a course of induction therapy with ipilimumab for melanoma, Dr. Bessesen noted.
"I’m not saying drugs should cost that much. I’m simply pointing out how society looks differently at these," she said.
With regard to the other three systemic antibiotics approved by the FDA in the 5 years since the 7-year drought ended, bedaquiline (Sirturo) is the most important globally, because it is indicated for multidrug-resistant tuberculosis. However, few U.S. physicians will have occasion to prescribe it.
Fidaxomicin (Dificid) is an effective drug for Clostridium difficile diarrhea; it’s eight times more potent than vancomycin against C. difficile, has minimal systemic absorption, and offers the major advantage of producing little negative impact on favorable gut flora. Telavancin (Vibativ) is a once-daily agent for hospital-acquired and ventilator-associated bacterial pneumonia.
Dr. Bessesen reported having no conflicts of interest.
ESTES PARK, COLO. – For primary care physicians, ceftaroline is hands-down the most exciting and important of the four systemic antibacterial agents to reach the U.S. market since the great 7-year drought in approvals ended in 2008, an infectious disease expert observed.
Ceftaroline (Teflaro) is a novel cephalosporin with unique binding to penicillin-binding proteins, including the altered versions that confer resistance in methicillin-resistant Staphylococcus aureus and penicillin- and cephalosporin-resistant Streptococcus pneumoniae. Thus, ceftaroline is a potent and effective drug in the increasingly common situation of beta-lactam-resistant community-acquired pneumonia (CAP) or complicated skin and soft tissue infections, noted Dr. Mary T. Bessesen, chief of the infectious diseases section at Denver V.A. Medical Center.
In the pivotal FOCUS 1 and FOCUS 2 trials conducted in patients with CAP not due to MRSA, ceftaroline proved noninferior overall to ceftriaxone (Rocephin). Of note, in the 14% of FOCUS participants with CAP due to S. aureus, ceftaroline proved to be significantly more effective than ceftriaxone. Importantly, the same was true among the one-third of FOCUS participants in whom S. pneumoniae was isolated (Clin. Infect. Dis. 2010;51:1395-405).
"I think if you’re going to impact mortality in CAP, pneumococcus has to be the primary target. Ceftaroline is a good alternative when penicillin-resistant S. pneumoniae is suspected or proven," Dr. Bessesen said at a conference on internal medicine sponsored by the University of Colorado.
Other common pathogens in CAP that are sensitive to ceftaroline are Hemophilus influenza and Moraxella catarrhalis. The Gram-negative pathogens E. coli, Klebsiella pneumoniae, and Enterobacter cloacae are also ceftaroline sensitive, with activity similar to ceftriaxone and ceftazidime (Fortaz).
Not only is MRSA sensitive to ceftaroline, so are methicillin-sensitive S. aureus, vancomycin-intermediate S. aureus, vancomycin-resistant S. aureus, linezolid (Zyvox)-resistant S. aureus, and daptomycin (Cubicin)-nonsusceptible S. aureus.
Ceftaroline does not cover the atypical pneumonia pathogens Mycoplasma pneumoniae, Chlamydia pneumoniae, and Legionella pneumoniae, nor does it cover Pseudomonas aeruginosa or extended-spectrum beta-lactamase-producing Enterobacteriaceae, stressed Dr. Bessesen.
The current CAP guidelines don’t include recommendations for ceftaroline, because the drug received Food and Drug Administration approval for treatment of CAP and complicated skin and soft tissue infections after the guidelines were issued.
Clinical trials investigating ceftaroline in CAP caused by MRSA would be welcome, Dr. Bessesen noted, because the current CAP guidelines don’t include any recommendations for CAP pneumonia.
"It really leaves us wondering in high-risk cases what’s best to do," she said. "There’s been some controversy about vancomycin versus linezolid when you suspect MRSA pneumonia. Ceftaroline would be a nice way to get around all of that."
Ceftaroline is administered intravenously twice daily, with dose adjustment for renal function. The drug’s pharmacokinetics are favorable for intramuscular injection, but there are limited clinical data for this route, and it is not FDA approved.
Ceftaroline costs about $84 per day, or four times more than ceftriaxone, Dr. Bessesen said. As a result, formulary committees are reluctant to put ceftaroline on the list.
That makes Dr. Bessesen see red.
"I’ve never been on a drug company speakers bureau. I’ve never had any research money from drug companies. I speak only as someone who’s interested in us being able to continue to treat bacterial infections when I say we’ve got to change our attitude. We have to be willing to pay something for these antibiotics," she asserted.
The antibiotic development pipeline has failed as pharmaceutical companies have abandoned the field, Dr. Bessesen continued. There are three reasons for this. One is that all the easy drugs have already been discovered. Another is that the FDA regulatory approval system for antibacterial agents is seriously outdated; the European Medicines Agency is much more forward thinking in this area and would be a useful model for FDA modernization, she noted.
But the biggest reason for the broken pipeline is that antibiotics are not a good financial investment for pharmaceutical companies. "It’s much more profitable for them to develop a drug like lovastatin that you’re going to take every day for the rest of your life than to develop an antibiotic you’re going to prescribe for a week or two. And society expects antibiotics to be cheap," Dr. Bessesen observed.
Contrast the roughly $1,600 cost of 4 weeks of ceftriaxone for S. viridans endocarditis – a serious infection – with the $54,000 price tag for 1 year of trastuzumab for breast cancer or $240,000 for a course of induction therapy with ipilimumab for melanoma, Dr. Bessesen noted.
"I’m not saying drugs should cost that much. I’m simply pointing out how society looks differently at these," she said.
With regard to the other three systemic antibiotics approved by the FDA in the 5 years since the 7-year drought ended, bedaquiline (Sirturo) is the most important globally, because it is indicated for multidrug-resistant tuberculosis. However, few U.S. physicians will have occasion to prescribe it.
Fidaxomicin (Dificid) is an effective drug for Clostridium difficile diarrhea; it’s eight times more potent than vancomycin against C. difficile, has minimal systemic absorption, and offers the major advantage of producing little negative impact on favorable gut flora. Telavancin (Vibativ) is a once-daily agent for hospital-acquired and ventilator-associated bacterial pneumonia.
Dr. Bessesen reported having no conflicts of interest.
ESTES PARK, COLO. – For primary care physicians, ceftaroline is hands-down the most exciting and important of the four systemic antibacterial agents to reach the U.S. market since the great 7-year drought in approvals ended in 2008, an infectious disease expert observed.
Ceftaroline (Teflaro) is a novel cephalosporin with unique binding to penicillin-binding proteins, including the altered versions that confer resistance in methicillin-resistant Staphylococcus aureus and penicillin- and cephalosporin-resistant Streptococcus pneumoniae. Thus, ceftaroline is a potent and effective drug in the increasingly common situation of beta-lactam-resistant community-acquired pneumonia (CAP) or complicated skin and soft tissue infections, noted Dr. Mary T. Bessesen, chief of the infectious diseases section at Denver V.A. Medical Center.
In the pivotal FOCUS 1 and FOCUS 2 trials conducted in patients with CAP not due to MRSA, ceftaroline proved noninferior overall to ceftriaxone (Rocephin). Of note, in the 14% of FOCUS participants with CAP due to S. aureus, ceftaroline proved to be significantly more effective than ceftriaxone. Importantly, the same was true among the one-third of FOCUS participants in whom S. pneumoniae was isolated (Clin. Infect. Dis. 2010;51:1395-405).
"I think if you’re going to impact mortality in CAP, pneumococcus has to be the primary target. Ceftaroline is a good alternative when penicillin-resistant S. pneumoniae is suspected or proven," Dr. Bessesen said at a conference on internal medicine sponsored by the University of Colorado.
Other common pathogens in CAP that are sensitive to ceftaroline are Hemophilus influenza and Moraxella catarrhalis. The Gram-negative pathogens E. coli, Klebsiella pneumoniae, and Enterobacter cloacae are also ceftaroline sensitive, with activity similar to ceftriaxone and ceftazidime (Fortaz).
Not only is MRSA sensitive to ceftaroline, so are methicillin-sensitive S. aureus, vancomycin-intermediate S. aureus, vancomycin-resistant S. aureus, linezolid (Zyvox)-resistant S. aureus, and daptomycin (Cubicin)-nonsusceptible S. aureus.
Ceftaroline does not cover the atypical pneumonia pathogens Mycoplasma pneumoniae, Chlamydia pneumoniae, and Legionella pneumoniae, nor does it cover Pseudomonas aeruginosa or extended-spectrum beta-lactamase-producing Enterobacteriaceae, stressed Dr. Bessesen.
The current CAP guidelines don’t include recommendations for ceftaroline, because the drug received Food and Drug Administration approval for treatment of CAP and complicated skin and soft tissue infections after the guidelines were issued.
Clinical trials investigating ceftaroline in CAP caused by MRSA would be welcome, Dr. Bessesen noted, because the current CAP guidelines don’t include any recommendations for CAP pneumonia.
"It really leaves us wondering in high-risk cases what’s best to do," she said. "There’s been some controversy about vancomycin versus linezolid when you suspect MRSA pneumonia. Ceftaroline would be a nice way to get around all of that."
Ceftaroline is administered intravenously twice daily, with dose adjustment for renal function. The drug’s pharmacokinetics are favorable for intramuscular injection, but there are limited clinical data for this route, and it is not FDA approved.
Ceftaroline costs about $84 per day, or four times more than ceftriaxone, Dr. Bessesen said. As a result, formulary committees are reluctant to put ceftaroline on the list.
That makes Dr. Bessesen see red.
"I’ve never been on a drug company speakers bureau. I’ve never had any research money from drug companies. I speak only as someone who’s interested in us being able to continue to treat bacterial infections when I say we’ve got to change our attitude. We have to be willing to pay something for these antibiotics," she asserted.
The antibiotic development pipeline has failed as pharmaceutical companies have abandoned the field, Dr. Bessesen continued. There are three reasons for this. One is that all the easy drugs have already been discovered. Another is that the FDA regulatory approval system for antibacterial agents is seriously outdated; the European Medicines Agency is much more forward thinking in this area and would be a useful model for FDA modernization, she noted.
But the biggest reason for the broken pipeline is that antibiotics are not a good financial investment for pharmaceutical companies. "It’s much more profitable for them to develop a drug like lovastatin that you’re going to take every day for the rest of your life than to develop an antibiotic you’re going to prescribe for a week or two. And society expects antibiotics to be cheap," Dr. Bessesen observed.
Contrast the roughly $1,600 cost of 4 weeks of ceftriaxone for S. viridans endocarditis – a serious infection – with the $54,000 price tag for 1 year of trastuzumab for breast cancer or $240,000 for a course of induction therapy with ipilimumab for melanoma, Dr. Bessesen noted.
"I’m not saying drugs should cost that much. I’m simply pointing out how society looks differently at these," she said.
With regard to the other three systemic antibiotics approved by the FDA in the 5 years since the 7-year drought ended, bedaquiline (Sirturo) is the most important globally, because it is indicated for multidrug-resistant tuberculosis. However, few U.S. physicians will have occasion to prescribe it.
Fidaxomicin (Dificid) is an effective drug for Clostridium difficile diarrhea; it’s eight times more potent than vancomycin against C. difficile, has minimal systemic absorption, and offers the major advantage of producing little negative impact on favorable gut flora. Telavancin (Vibativ) is a once-daily agent for hospital-acquired and ventilator-associated bacterial pneumonia.
Dr. Bessesen reported having no conflicts of interest.
EXPERT ANALYSIS FROM THE ANNUAL INTERNAL MEDICINE PROGRAM