User login
Phase III trial: VZV protects auto-HCT patients
ORLANDO – An inactivated varicella zoster virus vaccine currently in development for adult patients undergoing autologous hematopoietic stem cell transplantation is efficacious and well tolerated, according to findings from a randomized, placebo-controlled, phase III trial.
During the course of the 2 1/2-year pivotal multicenter trial, confirmed herpes zoster infections occurred in 42 of 560 patients who were randomized to receive inactivated varicella zoster virus vaccine (ZVIN) consistency lot (overall incidence of 32.8 cases/1,000 patient-years), compared with 113 of 564 patients who received placebo (overall incidence of 91.8/1,000 patient-years). The estimated vaccine efficacy was 63.8% after adjusting for age and duration of antiviral prophylaxis, Drew J. Winston, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
The vaccine also was effective for reducing moderate and severe herpes zoster pain (estimated vaccine efficacy, 69.5%), for preventing postherpetic neuralgia (estimated vaccine efficacy, 83.7%), and for prevention of herpes zoster–related complications (estimated vaccine efficacy, 73.5%), he noted.
Study subjects were adults aged 18 years or older who were undergoing autologous hematopoietic stem cell transplantation (auto-HCT) for a malignancy or other indication. The most common underlying diseases were lymphoma and multiple myeloma. All patients had a history of varicella infection or were seropositive for varicella zoster virus (VZV) antibody, and had no history of VZV vaccine or herpes zoster infection within the prior year.
They were randomized to receive a four-dose regimen of either ZVIN consistency lot, ZVIN high-antigen lot, or placebo. A group of 106 patients who received the ZVIN high-antigen lot were included in the safety analysis only. The first ZVIN dose was administered about a month before transplantation, and doses two through four were administered about 30, 60, and 90 days after transplantation. About 90% in each group received antiviral agents after transplantation, and the duration of the use of antivirals also was similar in the groups. All patients were followed for the duration of the study, and those who developed herpes zoster were followed for 6 months after onset.
Herpes zoster cases were confirmed by polymerase chain reaction or by blinded endpoint committee adjudication.
Serious adverse events and vaccine-related serious adverse events occurred in a similar proportion of patients in the treatment and placebo groups (32.9% and 32.7%, and 0.8% and 0.9%, respectively). Vaccine-related events were primarily injection-site reactions. Systemic adverse events that occurred up to 28 days after vaccination were mainly gastrointestinal side effects, such as diarrhea, nausea, and vomiting. Pyrexia, oral mucositis, thrombocytopenia, and febrile neutropenia also were reported.
The most common serious adverse events were infectious complications, such as febrile neutropenia and relapse of underlying disease.
The findings are notable, as patients undergoing auto-HCT have an increased risk of developing herpes zoster infection and its complications, including postherpetic neuralgia, secondary bacterial infections, and disseminated VZV infection, as well as an increased risk of hospitalization and mortality, Dr. Winston explained.
Herpes zoster infections are associated primarily with cell-mediated immunity, and in older studies done prior to the routine use of antiviral prophylaxis, the reported incidence in auto-HCT patients was between 16% and 25%. Because of this high risk, current guidelines call for antiviral prophylaxis during auto-HCT, but even in this current era of acyclovir or valacyclovir prophylaxis, infections occur at relatively high rates after auto-HCT, he noted.
“Now another approach to prevention of herpes zoster infection is vaccination,” he said.
The live attenuated vaccine currently on the market is generally contraindicated in immunocompromised patients – at least in early period after transplantation, but ZVIN showed promise with respect to safety in earlier studies, which led to the current trial.
“This study demonstrated that the inactivated varicella vaccine is very effective for preventing herpes zoster after autologous stem cell transplantation,” Dr. Winston said, noting that efficacy was observed both in those younger than age 50 years and in those aged 50 and older, and also in those who received prophylaxis for less than 3 months and for 3-6 months.
“Finally!” said one audience member, who noted during a discussion of the findings that there has long been a need for a vaccine to prevent herpes zoster in auto-HCT patients.
Dr. Winston reported receiving research funding from Oxford, and serving as a consultant to Merck and Chimerix.
ORLANDO – An inactivated varicella zoster virus vaccine currently in development for adult patients undergoing autologous hematopoietic stem cell transplantation is efficacious and well tolerated, according to findings from a randomized, placebo-controlled, phase III trial.
During the course of the 2 1/2-year pivotal multicenter trial, confirmed herpes zoster infections occurred in 42 of 560 patients who were randomized to receive inactivated varicella zoster virus vaccine (ZVIN) consistency lot (overall incidence of 32.8 cases/1,000 patient-years), compared with 113 of 564 patients who received placebo (overall incidence of 91.8/1,000 patient-years). The estimated vaccine efficacy was 63.8% after adjusting for age and duration of antiviral prophylaxis, Drew J. Winston, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
The vaccine also was effective for reducing moderate and severe herpes zoster pain (estimated vaccine efficacy, 69.5%), for preventing postherpetic neuralgia (estimated vaccine efficacy, 83.7%), and for prevention of herpes zoster–related complications (estimated vaccine efficacy, 73.5%), he noted.
Study subjects were adults aged 18 years or older who were undergoing autologous hematopoietic stem cell transplantation (auto-HCT) for a malignancy or other indication. The most common underlying diseases were lymphoma and multiple myeloma. All patients had a history of varicella infection or were seropositive for varicella zoster virus (VZV) antibody, and had no history of VZV vaccine or herpes zoster infection within the prior year.
They were randomized to receive a four-dose regimen of either ZVIN consistency lot, ZVIN high-antigen lot, or placebo. A group of 106 patients who received the ZVIN high-antigen lot were included in the safety analysis only. The first ZVIN dose was administered about a month before transplantation, and doses two through four were administered about 30, 60, and 90 days after transplantation. About 90% in each group received antiviral agents after transplantation, and the duration of the use of antivirals also was similar in the groups. All patients were followed for the duration of the study, and those who developed herpes zoster were followed for 6 months after onset.
Herpes zoster cases were confirmed by polymerase chain reaction or by blinded endpoint committee adjudication.
Serious adverse events and vaccine-related serious adverse events occurred in a similar proportion of patients in the treatment and placebo groups (32.9% and 32.7%, and 0.8% and 0.9%, respectively). Vaccine-related events were primarily injection-site reactions. Systemic adverse events that occurred up to 28 days after vaccination were mainly gastrointestinal side effects, such as diarrhea, nausea, and vomiting. Pyrexia, oral mucositis, thrombocytopenia, and febrile neutropenia also were reported.
The most common serious adverse events were infectious complications, such as febrile neutropenia and relapse of underlying disease.
The findings are notable, as patients undergoing auto-HCT have an increased risk of developing herpes zoster infection and its complications, including postherpetic neuralgia, secondary bacterial infections, and disseminated VZV infection, as well as an increased risk of hospitalization and mortality, Dr. Winston explained.
Herpes zoster infections are associated primarily with cell-mediated immunity, and in older studies done prior to the routine use of antiviral prophylaxis, the reported incidence in auto-HCT patients was between 16% and 25%. Because of this high risk, current guidelines call for antiviral prophylaxis during auto-HCT, but even in this current era of acyclovir or valacyclovir prophylaxis, infections occur at relatively high rates after auto-HCT, he noted.
“Now another approach to prevention of herpes zoster infection is vaccination,” he said.
The live attenuated vaccine currently on the market is generally contraindicated in immunocompromised patients – at least in early period after transplantation, but ZVIN showed promise with respect to safety in earlier studies, which led to the current trial.
“This study demonstrated that the inactivated varicella vaccine is very effective for preventing herpes zoster after autologous stem cell transplantation,” Dr. Winston said, noting that efficacy was observed both in those younger than age 50 years and in those aged 50 and older, and also in those who received prophylaxis for less than 3 months and for 3-6 months.
“Finally!” said one audience member, who noted during a discussion of the findings that there has long been a need for a vaccine to prevent herpes zoster in auto-HCT patients.
Dr. Winston reported receiving research funding from Oxford, and serving as a consultant to Merck and Chimerix.
ORLANDO – An inactivated varicella zoster virus vaccine currently in development for adult patients undergoing autologous hematopoietic stem cell transplantation is efficacious and well tolerated, according to findings from a randomized, placebo-controlled, phase III trial.
During the course of the 2 1/2-year pivotal multicenter trial, confirmed herpes zoster infections occurred in 42 of 560 patients who were randomized to receive inactivated varicella zoster virus vaccine (ZVIN) consistency lot (overall incidence of 32.8 cases/1,000 patient-years), compared with 113 of 564 patients who received placebo (overall incidence of 91.8/1,000 patient-years). The estimated vaccine efficacy was 63.8% after adjusting for age and duration of antiviral prophylaxis, Drew J. Winston, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
The vaccine also was effective for reducing moderate and severe herpes zoster pain (estimated vaccine efficacy, 69.5%), for preventing postherpetic neuralgia (estimated vaccine efficacy, 83.7%), and for prevention of herpes zoster–related complications (estimated vaccine efficacy, 73.5%), he noted.
Study subjects were adults aged 18 years or older who were undergoing autologous hematopoietic stem cell transplantation (auto-HCT) for a malignancy or other indication. The most common underlying diseases were lymphoma and multiple myeloma. All patients had a history of varicella infection or were seropositive for varicella zoster virus (VZV) antibody, and had no history of VZV vaccine or herpes zoster infection within the prior year.
They were randomized to receive a four-dose regimen of either ZVIN consistency lot, ZVIN high-antigen lot, or placebo. A group of 106 patients who received the ZVIN high-antigen lot were included in the safety analysis only. The first ZVIN dose was administered about a month before transplantation, and doses two through four were administered about 30, 60, and 90 days after transplantation. About 90% in each group received antiviral agents after transplantation, and the duration of the use of antivirals also was similar in the groups. All patients were followed for the duration of the study, and those who developed herpes zoster were followed for 6 months after onset.
Herpes zoster cases were confirmed by polymerase chain reaction or by blinded endpoint committee adjudication.
Serious adverse events and vaccine-related serious adverse events occurred in a similar proportion of patients in the treatment and placebo groups (32.9% and 32.7%, and 0.8% and 0.9%, respectively). Vaccine-related events were primarily injection-site reactions. Systemic adverse events that occurred up to 28 days after vaccination were mainly gastrointestinal side effects, such as diarrhea, nausea, and vomiting. Pyrexia, oral mucositis, thrombocytopenia, and febrile neutropenia also were reported.
The most common serious adverse events were infectious complications, such as febrile neutropenia and relapse of underlying disease.
The findings are notable, as patients undergoing auto-HCT have an increased risk of developing herpes zoster infection and its complications, including postherpetic neuralgia, secondary bacterial infections, and disseminated VZV infection, as well as an increased risk of hospitalization and mortality, Dr. Winston explained.
Herpes zoster infections are associated primarily with cell-mediated immunity, and in older studies done prior to the routine use of antiviral prophylaxis, the reported incidence in auto-HCT patients was between 16% and 25%. Because of this high risk, current guidelines call for antiviral prophylaxis during auto-HCT, but even in this current era of acyclovir or valacyclovir prophylaxis, infections occur at relatively high rates after auto-HCT, he noted.
“Now another approach to prevention of herpes zoster infection is vaccination,” he said.
The live attenuated vaccine currently on the market is generally contraindicated in immunocompromised patients – at least in early period after transplantation, but ZVIN showed promise with respect to safety in earlier studies, which led to the current trial.
“This study demonstrated that the inactivated varicella vaccine is very effective for preventing herpes zoster after autologous stem cell transplantation,” Dr. Winston said, noting that efficacy was observed both in those younger than age 50 years and in those aged 50 and older, and also in those who received prophylaxis for less than 3 months and for 3-6 months.
“Finally!” said one audience member, who noted during a discussion of the findings that there has long been a need for a vaccine to prevent herpes zoster in auto-HCT patients.
Dr. Winston reported receiving research funding from Oxford, and serving as a consultant to Merck and Chimerix.
AT THE 2017 BMT TANDEM MEETINGS
Key clinical point:
Major finding: Overall incidence of herpes zoster was 32.8 cases/1,000 patient-years vs. 91.8/1,000 patient-years in patients in the vaccine and placebo groups, respectively.
Data source: A randomized, placebo-controlled phase III trial involving 1,230 patients.
Disclosures: Dr. Winston reported receiving research funding from Oxford, and serving as a consultant to Merck and Chimerix.
Fewer post-transplant CMV infections with novel antiviral prophylaxis
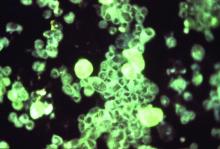
ORLANDO – A first-in-class antiviral drug was safe and effective when used to prevent clinically significant cytomegalovirus infections in adults undergoing hematopoietic cell transplantation.
At 24 weeks post-transplant, 38% (122/325) of those receiving the novel antiviral letermovir were considered treatment failures, compared with 61% (103/170) of those receiving placebo (P less than .0001). All-cause mortality was 10% (n=32/325) for patients receiving letermovir and 16%, (n=27/170) for the placebo group (log rank two-sided P = 0.0317).
The study findings show that “we [can] prevent patients from getting CMV infections from the beginning of the transplant and that [result can] confer a mortality benefit,” lead author Francisco Marty, MD, said in an interview.
Dr. Marty said that letermovir has received fast-track status both from the Food and Drug Administration and from the European Medicines Agency.
HCT recipients who are CMV-positive but who do not have clinically significant disease are not preemptively treated in current practice. “Previously, there wasn’t a primary prevention strategy in bone marrow transplantation. When myelosuppressive drugs were tried such as ganciclovir, any benefit was offset by increased myelosuppression, with resulting increases in bacterial and fungal infections,” said Dr. Marty, professor of medicine at Harvard Medical School, Boston.
Letermovir was generally well-tolerated in the clinical trial; myelotoxicity and nephrotoxicity levels were comparable in patients receiving letermovir and placebo. Letermovir targets the terminase complex, which is a viral replication process specific to CMV and not otherwise present in humans. That fact may explain, in part, letermovir’s limited toxicity, Dr. Marty said. The primary outcome measure of the phase III randomized, double-blind, placebo-controlled trial was the stratum-adjusted proportion of patients who had clinically significant CMV at post-transplant week 24, examining only the patients in the trials who had no detectable CMV DNA at the time of randomization. If patients did not complete the study, or had missing data at week 24, they were considered to have failed the trial.
Overall, 31% of patients were considered at high risk for CMV disease. Half of the patients received myeloablative conditioning, and about a third (35%) received antithymocyte globulin. Donor sources, whose characteristics were balanced between study arms, included 14% mismatched unrelated donors, 13% haploidentical donors, and 4% cord blood.
The multinational study’s 24-week results were presented at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation.
“This was an international study, conducted at multiple sites in multiple countries. We used two-to-one randomization, and stratified participants by their risk of CMV disease and by study sites. We wanted to make sure the groups were balanced by disease risk and by study sites, to account for regional variations in bone marrow transplant procedures and CMV treatment patterns,” said Dr. Marty.
For the study, clinically significant CMV infection was defined as either CMV disease, such as pneumonia, colitis, or hepatitis, or CMV viremia that would trigger preemptive treatment.
Letermovir, which can be administered orally or intravenously, was dosed at 480 mg per day. Because of the risk for a drug-drug interaction, patients on cyclosporine received 240 mg of letermovir per day. Having intravenous dosing as an option helped patients who were not tolerating oral intake to stay on the study drug during the post-transplant period, he said.
The study drug was begun a median of 9 days post-transplant. Some patients received letermovir or placebo as early as the day of transplant; all patients began the study drug by 28 days post-transplant. The study drug was continued through week 14, or until at least 100 days post-transplant. Overall, 37% of patients had engrafted at the time they began the study drug.
Patients had weekly serum CMV assays performed until week 14, with biweekly sampling done through week 24. If patients developed clinically significant CMV, or if their serum samples yielded CMV DNA warranting preemptive treatment, they discontinued the study drug and began treatment for CMV.
The safety analysis, which was carried through week 48, tracked adverse events from the first dose of study drug until 14 days after discontinuation. Adverse events that were more common with letermovir than placebo included vomiting (19% versus 14%), edema (15% versus 9%), atrial arrhythmias (10% versus 5%), and having alanine aspartate levels more than five times the upper limit of normal (4% versus 2%). Graft versus host disease occurred in 39% of patients in each group; diarrhea and nausea occurred in approximately one fourth of patients in each group.
In response to a question after the presentation, Dr. Marty said, “The higher the risk of CMV disease, the higher the benefit in terms of survival.” Answering another question, about who should receive letermovir. Dr. Marty replied, “Like acyclovir, we should give it during times of risk. And CMV risk is different for different populations. It’s a matter of managing risks and benefits.”
Though letermovir was safe and well-tolerated in this trial, it’s different from acyclovir in that “it’s not a one dollar a day drug,” Dr. Marty acknowledged.
Merck, which plans to market letermovir, was the sponsor of the study and plans to submit applications for approval in both the United States and in the European Union in 2017. Dr. Marty reported receiving research grants from Merck as well as Astellas, Chimerix, and Shire. Additionally, he has received honoraria from Alexion, Chimerix, LFB, Merck, Roche Molecular Diagnostics, and Shire.
This article was updated 2/27/17.
koakes@frontlinemedcom.com
On Twitter @karioakes
ORLANDO – A first-in-class antiviral drug was safe and effective when used to prevent clinically significant cytomegalovirus infections in adults undergoing hematopoietic cell transplantation.
At 24 weeks post-transplant, 38% (122/325) of those receiving the novel antiviral letermovir were considered treatment failures, compared with 61% (103/170) of those receiving placebo (P less than .0001). All-cause mortality was 10% (n=32/325) for patients receiving letermovir and 16%, (n=27/170) for the placebo group (log rank two-sided P = 0.0317).
The study findings show that “we [can] prevent patients from getting CMV infections from the beginning of the transplant and that [result can] confer a mortality benefit,” lead author Francisco Marty, MD, said in an interview.
Dr. Marty said that letermovir has received fast-track status both from the Food and Drug Administration and from the European Medicines Agency.
HCT recipients who are CMV-positive but who do not have clinically significant disease are not preemptively treated in current practice. “Previously, there wasn’t a primary prevention strategy in bone marrow transplantation. When myelosuppressive drugs were tried such as ganciclovir, any benefit was offset by increased myelosuppression, with resulting increases in bacterial and fungal infections,” said Dr. Marty, professor of medicine at Harvard Medical School, Boston.
Letermovir was generally well-tolerated in the clinical trial; myelotoxicity and nephrotoxicity levels were comparable in patients receiving letermovir and placebo. Letermovir targets the terminase complex, which is a viral replication process specific to CMV and not otherwise present in humans. That fact may explain, in part, letermovir’s limited toxicity, Dr. Marty said. The primary outcome measure of the phase III randomized, double-blind, placebo-controlled trial was the stratum-adjusted proportion of patients who had clinically significant CMV at post-transplant week 24, examining only the patients in the trials who had no detectable CMV DNA at the time of randomization. If patients did not complete the study, or had missing data at week 24, they were considered to have failed the trial.
Overall, 31% of patients were considered at high risk for CMV disease. Half of the patients received myeloablative conditioning, and about a third (35%) received antithymocyte globulin. Donor sources, whose characteristics were balanced between study arms, included 14% mismatched unrelated donors, 13% haploidentical donors, and 4% cord blood.
The multinational study’s 24-week results were presented at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation.
“This was an international study, conducted at multiple sites in multiple countries. We used two-to-one randomization, and stratified participants by their risk of CMV disease and by study sites. We wanted to make sure the groups were balanced by disease risk and by study sites, to account for regional variations in bone marrow transplant procedures and CMV treatment patterns,” said Dr. Marty.
For the study, clinically significant CMV infection was defined as either CMV disease, such as pneumonia, colitis, or hepatitis, or CMV viremia that would trigger preemptive treatment.
Letermovir, which can be administered orally or intravenously, was dosed at 480 mg per day. Because of the risk for a drug-drug interaction, patients on cyclosporine received 240 mg of letermovir per day. Having intravenous dosing as an option helped patients who were not tolerating oral intake to stay on the study drug during the post-transplant period, he said.
The study drug was begun a median of 9 days post-transplant. Some patients received letermovir or placebo as early as the day of transplant; all patients began the study drug by 28 days post-transplant. The study drug was continued through week 14, or until at least 100 days post-transplant. Overall, 37% of patients had engrafted at the time they began the study drug.
Patients had weekly serum CMV assays performed until week 14, with biweekly sampling done through week 24. If patients developed clinically significant CMV, or if their serum samples yielded CMV DNA warranting preemptive treatment, they discontinued the study drug and began treatment for CMV.
The safety analysis, which was carried through week 48, tracked adverse events from the first dose of study drug until 14 days after discontinuation. Adverse events that were more common with letermovir than placebo included vomiting (19% versus 14%), edema (15% versus 9%), atrial arrhythmias (10% versus 5%), and having alanine aspartate levels more than five times the upper limit of normal (4% versus 2%). Graft versus host disease occurred in 39% of patients in each group; diarrhea and nausea occurred in approximately one fourth of patients in each group.
In response to a question after the presentation, Dr. Marty said, “The higher the risk of CMV disease, the higher the benefit in terms of survival.” Answering another question, about who should receive letermovir. Dr. Marty replied, “Like acyclovir, we should give it during times of risk. And CMV risk is different for different populations. It’s a matter of managing risks and benefits.”
Though letermovir was safe and well-tolerated in this trial, it’s different from acyclovir in that “it’s not a one dollar a day drug,” Dr. Marty acknowledged.
Merck, which plans to market letermovir, was the sponsor of the study and plans to submit applications for approval in both the United States and in the European Union in 2017. Dr. Marty reported receiving research grants from Merck as well as Astellas, Chimerix, and Shire. Additionally, he has received honoraria from Alexion, Chimerix, LFB, Merck, Roche Molecular Diagnostics, and Shire.
This article was updated 2/27/17.
koakes@frontlinemedcom.com
On Twitter @karioakes
ORLANDO – A first-in-class antiviral drug was safe and effective when used to prevent clinically significant cytomegalovirus infections in adults undergoing hematopoietic cell transplantation.
At 24 weeks post-transplant, 38% (122/325) of those receiving the novel antiviral letermovir were considered treatment failures, compared with 61% (103/170) of those receiving placebo (P less than .0001). All-cause mortality was 10% (n=32/325) for patients receiving letermovir and 16%, (n=27/170) for the placebo group (log rank two-sided P = 0.0317).
The study findings show that “we [can] prevent patients from getting CMV infections from the beginning of the transplant and that [result can] confer a mortality benefit,” lead author Francisco Marty, MD, said in an interview.
Dr. Marty said that letermovir has received fast-track status both from the Food and Drug Administration and from the European Medicines Agency.
HCT recipients who are CMV-positive but who do not have clinically significant disease are not preemptively treated in current practice. “Previously, there wasn’t a primary prevention strategy in bone marrow transplantation. When myelosuppressive drugs were tried such as ganciclovir, any benefit was offset by increased myelosuppression, with resulting increases in bacterial and fungal infections,” said Dr. Marty, professor of medicine at Harvard Medical School, Boston.
Letermovir was generally well-tolerated in the clinical trial; myelotoxicity and nephrotoxicity levels were comparable in patients receiving letermovir and placebo. Letermovir targets the terminase complex, which is a viral replication process specific to CMV and not otherwise present in humans. That fact may explain, in part, letermovir’s limited toxicity, Dr. Marty said. The primary outcome measure of the phase III randomized, double-blind, placebo-controlled trial was the stratum-adjusted proportion of patients who had clinically significant CMV at post-transplant week 24, examining only the patients in the trials who had no detectable CMV DNA at the time of randomization. If patients did not complete the study, or had missing data at week 24, they were considered to have failed the trial.
Overall, 31% of patients were considered at high risk for CMV disease. Half of the patients received myeloablative conditioning, and about a third (35%) received antithymocyte globulin. Donor sources, whose characteristics were balanced between study arms, included 14% mismatched unrelated donors, 13% haploidentical donors, and 4% cord blood.
The multinational study’s 24-week results were presented at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation.
“This was an international study, conducted at multiple sites in multiple countries. We used two-to-one randomization, and stratified participants by their risk of CMV disease and by study sites. We wanted to make sure the groups were balanced by disease risk and by study sites, to account for regional variations in bone marrow transplant procedures and CMV treatment patterns,” said Dr. Marty.
For the study, clinically significant CMV infection was defined as either CMV disease, such as pneumonia, colitis, or hepatitis, or CMV viremia that would trigger preemptive treatment.
Letermovir, which can be administered orally or intravenously, was dosed at 480 mg per day. Because of the risk for a drug-drug interaction, patients on cyclosporine received 240 mg of letermovir per day. Having intravenous dosing as an option helped patients who were not tolerating oral intake to stay on the study drug during the post-transplant period, he said.
The study drug was begun a median of 9 days post-transplant. Some patients received letermovir or placebo as early as the day of transplant; all patients began the study drug by 28 days post-transplant. The study drug was continued through week 14, or until at least 100 days post-transplant. Overall, 37% of patients had engrafted at the time they began the study drug.
Patients had weekly serum CMV assays performed until week 14, with biweekly sampling done through week 24. If patients developed clinically significant CMV, or if their serum samples yielded CMV DNA warranting preemptive treatment, they discontinued the study drug and began treatment for CMV.
The safety analysis, which was carried through week 48, tracked adverse events from the first dose of study drug until 14 days after discontinuation. Adverse events that were more common with letermovir than placebo included vomiting (19% versus 14%), edema (15% versus 9%), atrial arrhythmias (10% versus 5%), and having alanine aspartate levels more than five times the upper limit of normal (4% versus 2%). Graft versus host disease occurred in 39% of patients in each group; diarrhea and nausea occurred in approximately one fourth of patients in each group.
In response to a question after the presentation, Dr. Marty said, “The higher the risk of CMV disease, the higher the benefit in terms of survival.” Answering another question, about who should receive letermovir. Dr. Marty replied, “Like acyclovir, we should give it during times of risk. And CMV risk is different for different populations. It’s a matter of managing risks and benefits.”
Though letermovir was safe and well-tolerated in this trial, it’s different from acyclovir in that “it’s not a one dollar a day drug,” Dr. Marty acknowledged.
Merck, which plans to market letermovir, was the sponsor of the study and plans to submit applications for approval in both the United States and in the European Union in 2017. Dr. Marty reported receiving research grants from Merck as well as Astellas, Chimerix, and Shire. Additionally, he has received honoraria from Alexion, Chimerix, LFB, Merck, Roche Molecular Diagnostics, and Shire.
This article was updated 2/27/17.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT THE 2017 BMT TANDEM MEETINGS
Key clinical point:
Major finding: Cytomegalovirus (CMV) infection or viremia occurred in 38% of patients receiving post-HCT letermovir, compared with 61% of controls.
Data source: Randomized, double-blind, placebo-controlled study of 495 patients seropositive for CMV with no detectable CMV DNA at the time of HCT.
Disclosures: Merck, which plans to market letermovir, was the sponsor of the study. Dr. Marty reported receiving research grants from Merck as well as Astellas, Chimerix, and Shire. Additionally, he has received honoraria from Alexion, Chimerix, LFB, Merck, Roche Molecular Diagnostics, and Shire.