User login
VIDEO: Intestinal remodeling contributes to HbA1c drop after Roux-en-Y gastric bypass
CHICAGO – Of medical and surgical tactics to tackle long-term weight loss, , and gene expression in the Roux limb may hold the key to the surgery’s efficacy, according to an ongoing study.
“We know that Roux-en-Y gastric bypass surgery is highly effective as not only a weight-loss therapy, but more and more we’re appreciating its role as a diabetes therapy as well,” said Margaret Stefater, MD, PhD, speaking in an interview at the annual meeting of the Endocrine Society.
The study, she said, was designed to learn more about the intestine’s contribution to the salubrious effect that Roux-en-Y surgery has on diabetes.
“We used microarray in order to characterize gene expression in the intestine” to gain a broad understanding of the processes that are altered after surgery, said Dr. Stefater, a pediatric endocrinology fellow at Boston Children’s Hospital. More specifically, though, the study looked at an individual’s changes in gene expression over time and correlated those changes with that patient’s clinical picture.
The data reported by Dr. Stefater and shared in a press conference, represent part of an ongoing longitudinal prospective study of 32 patients.
“The study aims to characterize gene expression for the first postoperative year,” and findings from the first 6 postoperative months of 19 patients were shared at the meeting, said Dr. Stefater. “This is the first look at our cohort.”
So far, she and her colleagues have compared gene expression using microarray at 1 month and 6 months post-surgery, comparing change across time and change from baseline data.
From hundreds of candidate genes, Dr. Stefater and her colleagues have developed a smaller gene list that, even in the first postoperative month, is predictive of changes in hemoglobin A1c levels over time. “Remarkably, the changes in a select list of genes out to 1 month is actually able to predict hemoglobin A1c levels out to 1 year,” she said. “This speaks to the fact that biological reprogramming in the intestine is somehow related to glycemic response in patients.
“We hope that by understanding these processes, we can home in on those processes that are most likely to be mechanistically responsible for these changes, and then to reverse-engineer this surgery to identify processes or targets which may be good places to start when we think about creating better, or nonsurgical, therapies for people who have obesity and diabetes,” said Dr. Stefater.
Dr. Stefater reported no relevant financial disclosures.
SOURCE: Stefater MA et al. ENDO 2018, Abstract OR 12-6.
CHICAGO – Of medical and surgical tactics to tackle long-term weight loss, , and gene expression in the Roux limb may hold the key to the surgery’s efficacy, according to an ongoing study.
“We know that Roux-en-Y gastric bypass surgery is highly effective as not only a weight-loss therapy, but more and more we’re appreciating its role as a diabetes therapy as well,” said Margaret Stefater, MD, PhD, speaking in an interview at the annual meeting of the Endocrine Society.
The study, she said, was designed to learn more about the intestine’s contribution to the salubrious effect that Roux-en-Y surgery has on diabetes.
“We used microarray in order to characterize gene expression in the intestine” to gain a broad understanding of the processes that are altered after surgery, said Dr. Stefater, a pediatric endocrinology fellow at Boston Children’s Hospital. More specifically, though, the study looked at an individual’s changes in gene expression over time and correlated those changes with that patient’s clinical picture.
The data reported by Dr. Stefater and shared in a press conference, represent part of an ongoing longitudinal prospective study of 32 patients.
“The study aims to characterize gene expression for the first postoperative year,” and findings from the first 6 postoperative months of 19 patients were shared at the meeting, said Dr. Stefater. “This is the first look at our cohort.”
So far, she and her colleagues have compared gene expression using microarray at 1 month and 6 months post-surgery, comparing change across time and change from baseline data.
From hundreds of candidate genes, Dr. Stefater and her colleagues have developed a smaller gene list that, even in the first postoperative month, is predictive of changes in hemoglobin A1c levels over time. “Remarkably, the changes in a select list of genes out to 1 month is actually able to predict hemoglobin A1c levels out to 1 year,” she said. “This speaks to the fact that biological reprogramming in the intestine is somehow related to glycemic response in patients.
“We hope that by understanding these processes, we can home in on those processes that are most likely to be mechanistically responsible for these changes, and then to reverse-engineer this surgery to identify processes or targets which may be good places to start when we think about creating better, or nonsurgical, therapies for people who have obesity and diabetes,” said Dr. Stefater.
Dr. Stefater reported no relevant financial disclosures.
SOURCE: Stefater MA et al. ENDO 2018, Abstract OR 12-6.
CHICAGO – Of medical and surgical tactics to tackle long-term weight loss, , and gene expression in the Roux limb may hold the key to the surgery’s efficacy, according to an ongoing study.
“We know that Roux-en-Y gastric bypass surgery is highly effective as not only a weight-loss therapy, but more and more we’re appreciating its role as a diabetes therapy as well,” said Margaret Stefater, MD, PhD, speaking in an interview at the annual meeting of the Endocrine Society.
The study, she said, was designed to learn more about the intestine’s contribution to the salubrious effect that Roux-en-Y surgery has on diabetes.
“We used microarray in order to characterize gene expression in the intestine” to gain a broad understanding of the processes that are altered after surgery, said Dr. Stefater, a pediatric endocrinology fellow at Boston Children’s Hospital. More specifically, though, the study looked at an individual’s changes in gene expression over time and correlated those changes with that patient’s clinical picture.
The data reported by Dr. Stefater and shared in a press conference, represent part of an ongoing longitudinal prospective study of 32 patients.
“The study aims to characterize gene expression for the first postoperative year,” and findings from the first 6 postoperative months of 19 patients were shared at the meeting, said Dr. Stefater. “This is the first look at our cohort.”
So far, she and her colleagues have compared gene expression using microarray at 1 month and 6 months post-surgery, comparing change across time and change from baseline data.
From hundreds of candidate genes, Dr. Stefater and her colleagues have developed a smaller gene list that, even in the first postoperative month, is predictive of changes in hemoglobin A1c levels over time. “Remarkably, the changes in a select list of genes out to 1 month is actually able to predict hemoglobin A1c levels out to 1 year,” she said. “This speaks to the fact that biological reprogramming in the intestine is somehow related to glycemic response in patients.
“We hope that by understanding these processes, we can home in on those processes that are most likely to be mechanistically responsible for these changes, and then to reverse-engineer this surgery to identify processes or targets which may be good places to start when we think about creating better, or nonsurgical, therapies for people who have obesity and diabetes,” said Dr. Stefater.
Dr. Stefater reported no relevant financial disclosures.
SOURCE: Stefater MA et al. ENDO 2018, Abstract OR 12-6.
REPORTING FROM ENDO 2018
Think about breast cancer surveillance for transgender patients
CHICAGO – , said Christel de Blok, MD, sharing results of a Dutch national study.
The study included 3,078 transgender people (2,064 transgender women) who began hormone therapy (HT) at age 18 years or older. The mean age at which transgender women began HT was 33 years; for transgender men, the mean age was 25 years. In all, transgender women in the study had a total of 30,699 person-years of exposure to HT; for transgender men, the figure was 13,155 person-years.
Overall, there were 16 observed cases of breast cancer in transgender women and four in transgender men. After gender-affirming surgery, the transgender women were followed for a median of 146 months, and experienced a median of 193 months of HT. Transgender men who had mastectomies were followed for a median 93 months, and those who had a hysterectomy-oophorectomy were followed for a median 144 months. Transgender men received a median 176 months of HT.
“Breast cancer can still occur after mastectomy in [transgender] men,” Dr. de Blok said at the annual meeting of the Endocrine Society. “What is interesting is that three out of the four cases of breast cancer in [transgender] men happened after mastectomy.”
In the Netherlands, one in eight women and one in 1,000 men will develop cancer at some point during their lives. In patients who have had a subtotal mastectomy and who are BRCA-1/2 carriers, there is still an approximate 5% residual risk of breast cancer, said Dr. de Blok.
A literature review conducted by Dr. de Blok and her colleagues revealed 19 cases of breast cancer in transgender women and 13 in transgender men. However, a more general study of incidence and characteristics of breast cancer in transgender people receiving hormone treatment had not been done, said Dr. de Blok, of the VU University Medical Center, Amsterdam.
The investigators examined data for adult transgender people seen at their center from 1991 to 2017 and started on hormone treatment. This clinic, said Dr. de Blok, sees about 95% of the transgender individuals in the Netherlands.
The study was able to capitalize on comprehensive information from national databases and registries. Investigators drew from a national histopathology and cytopathology registry as well as from a national vital statistics database. A comprehensive cancer database was used to establish both reference incidence values for males and females and the number of expected cases within the study group.
In both transgender men and women, exactly 50% of cases were ductal carcinoma, compared to 85% in the group of reference women.
An additional 31% of the breast cancers in transgender women were lobular, 6% were ductal carcinoma in situ (DCIS), and the remainder were of other types. Of the cancers in transgender women, 82% were estrogen receptor positive, 64% were progesterone receptor positive, and 9% were Her2/neu positive.
For transgender men, there were no lobular carcinomas; 25% were DCIS, and 25% were of other types. Half of the cancers were estrogen receptor positive, and half were progesterone receptor positive; 25% were Her2/neu positive, and there was one case of androgen receptor positive breast cancer.
Dr. de Blok explained that their analysis compared the observed cases in both transgender men and women to the expected number of cases for the same number of males and females, yielding two standardized incidence ratios (SIRs) for each transgender group.
For transgender women, the SIR for breast cancer compared with males was 50.9 (95% confidence interval, 30.1-80.9). The SIR compared to females was 0.3 (95% CI, 0.2-0.4). This reflected the expected case number of 0.3 for males and the 58 expected cases for a matched group of females.
For transgender men, the SIR for breast cancer compared with males was 59.8 (95% CI, 19-144.3), while the SIR compared to females was 0.2 (95% CI, 0.1-0.5). The expected cases for a similar group of males would be 0.1, and for females, 18.
In many cases, whether a transgender person receives standardized screening mammogram reminders will depend on which sex is assigned to that individual in insurance and other administrative databases, Mr. de Blok noted. When electronic health records and other databases have a binary system, at-risk individuals may fall through the cracks.
Dr. de Blok reported no conflicts of interest.
SOURCE: de Blok C, et al. ENDO 2018, abstract OR 25-6.
CHICAGO – , said Christel de Blok, MD, sharing results of a Dutch national study.
The study included 3,078 transgender people (2,064 transgender women) who began hormone therapy (HT) at age 18 years or older. The mean age at which transgender women began HT was 33 years; for transgender men, the mean age was 25 years. In all, transgender women in the study had a total of 30,699 person-years of exposure to HT; for transgender men, the figure was 13,155 person-years.
Overall, there were 16 observed cases of breast cancer in transgender women and four in transgender men. After gender-affirming surgery, the transgender women were followed for a median of 146 months, and experienced a median of 193 months of HT. Transgender men who had mastectomies were followed for a median 93 months, and those who had a hysterectomy-oophorectomy were followed for a median 144 months. Transgender men received a median 176 months of HT.
“Breast cancer can still occur after mastectomy in [transgender] men,” Dr. de Blok said at the annual meeting of the Endocrine Society. “What is interesting is that three out of the four cases of breast cancer in [transgender] men happened after mastectomy.”
In the Netherlands, one in eight women and one in 1,000 men will develop cancer at some point during their lives. In patients who have had a subtotal mastectomy and who are BRCA-1/2 carriers, there is still an approximate 5% residual risk of breast cancer, said Dr. de Blok.
A literature review conducted by Dr. de Blok and her colleagues revealed 19 cases of breast cancer in transgender women and 13 in transgender men. However, a more general study of incidence and characteristics of breast cancer in transgender people receiving hormone treatment had not been done, said Dr. de Blok, of the VU University Medical Center, Amsterdam.
The investigators examined data for adult transgender people seen at their center from 1991 to 2017 and started on hormone treatment. This clinic, said Dr. de Blok, sees about 95% of the transgender individuals in the Netherlands.
The study was able to capitalize on comprehensive information from national databases and registries. Investigators drew from a national histopathology and cytopathology registry as well as from a national vital statistics database. A comprehensive cancer database was used to establish both reference incidence values for males and females and the number of expected cases within the study group.
In both transgender men and women, exactly 50% of cases were ductal carcinoma, compared to 85% in the group of reference women.
An additional 31% of the breast cancers in transgender women were lobular, 6% were ductal carcinoma in situ (DCIS), and the remainder were of other types. Of the cancers in transgender women, 82% were estrogen receptor positive, 64% were progesterone receptor positive, and 9% were Her2/neu positive.
For transgender men, there were no lobular carcinomas; 25% were DCIS, and 25% were of other types. Half of the cancers were estrogen receptor positive, and half were progesterone receptor positive; 25% were Her2/neu positive, and there was one case of androgen receptor positive breast cancer.
Dr. de Blok explained that their analysis compared the observed cases in both transgender men and women to the expected number of cases for the same number of males and females, yielding two standardized incidence ratios (SIRs) for each transgender group.
For transgender women, the SIR for breast cancer compared with males was 50.9 (95% confidence interval, 30.1-80.9). The SIR compared to females was 0.3 (95% CI, 0.2-0.4). This reflected the expected case number of 0.3 for males and the 58 expected cases for a matched group of females.
For transgender men, the SIR for breast cancer compared with males was 59.8 (95% CI, 19-144.3), while the SIR compared to females was 0.2 (95% CI, 0.1-0.5). The expected cases for a similar group of males would be 0.1, and for females, 18.
In many cases, whether a transgender person receives standardized screening mammogram reminders will depend on which sex is assigned to that individual in insurance and other administrative databases, Mr. de Blok noted. When electronic health records and other databases have a binary system, at-risk individuals may fall through the cracks.
Dr. de Blok reported no conflicts of interest.
SOURCE: de Blok C, et al. ENDO 2018, abstract OR 25-6.
CHICAGO – , said Christel de Blok, MD, sharing results of a Dutch national study.
The study included 3,078 transgender people (2,064 transgender women) who began hormone therapy (HT) at age 18 years or older. The mean age at which transgender women began HT was 33 years; for transgender men, the mean age was 25 years. In all, transgender women in the study had a total of 30,699 person-years of exposure to HT; for transgender men, the figure was 13,155 person-years.
Overall, there were 16 observed cases of breast cancer in transgender women and four in transgender men. After gender-affirming surgery, the transgender women were followed for a median of 146 months, and experienced a median of 193 months of HT. Transgender men who had mastectomies were followed for a median 93 months, and those who had a hysterectomy-oophorectomy were followed for a median 144 months. Transgender men received a median 176 months of HT.
“Breast cancer can still occur after mastectomy in [transgender] men,” Dr. de Blok said at the annual meeting of the Endocrine Society. “What is interesting is that three out of the four cases of breast cancer in [transgender] men happened after mastectomy.”
In the Netherlands, one in eight women and one in 1,000 men will develop cancer at some point during their lives. In patients who have had a subtotal mastectomy and who are BRCA-1/2 carriers, there is still an approximate 5% residual risk of breast cancer, said Dr. de Blok.
A literature review conducted by Dr. de Blok and her colleagues revealed 19 cases of breast cancer in transgender women and 13 in transgender men. However, a more general study of incidence and characteristics of breast cancer in transgender people receiving hormone treatment had not been done, said Dr. de Blok, of the VU University Medical Center, Amsterdam.
The investigators examined data for adult transgender people seen at their center from 1991 to 2017 and started on hormone treatment. This clinic, said Dr. de Blok, sees about 95% of the transgender individuals in the Netherlands.
The study was able to capitalize on comprehensive information from national databases and registries. Investigators drew from a national histopathology and cytopathology registry as well as from a national vital statistics database. A comprehensive cancer database was used to establish both reference incidence values for males and females and the number of expected cases within the study group.
In both transgender men and women, exactly 50% of cases were ductal carcinoma, compared to 85% in the group of reference women.
An additional 31% of the breast cancers in transgender women were lobular, 6% were ductal carcinoma in situ (DCIS), and the remainder were of other types. Of the cancers in transgender women, 82% were estrogen receptor positive, 64% were progesterone receptor positive, and 9% were Her2/neu positive.
For transgender men, there were no lobular carcinomas; 25% were DCIS, and 25% were of other types. Half of the cancers were estrogen receptor positive, and half were progesterone receptor positive; 25% were Her2/neu positive, and there was one case of androgen receptor positive breast cancer.
Dr. de Blok explained that their analysis compared the observed cases in both transgender men and women to the expected number of cases for the same number of males and females, yielding two standardized incidence ratios (SIRs) for each transgender group.
For transgender women, the SIR for breast cancer compared with males was 50.9 (95% confidence interval, 30.1-80.9). The SIR compared to females was 0.3 (95% CI, 0.2-0.4). This reflected the expected case number of 0.3 for males and the 58 expected cases for a matched group of females.
For transgender men, the SIR for breast cancer compared with males was 59.8 (95% CI, 19-144.3), while the SIR compared to females was 0.2 (95% CI, 0.1-0.5). The expected cases for a similar group of males would be 0.1, and for females, 18.
In many cases, whether a transgender person receives standardized screening mammogram reminders will depend on which sex is assigned to that individual in insurance and other administrative databases, Mr. de Blok noted. When electronic health records and other databases have a binary system, at-risk individuals may fall through the cracks.
Dr. de Blok reported no conflicts of interest.
SOURCE: de Blok C, et al. ENDO 2018, abstract OR 25-6.
REPORTING FROM ENDO 2018
Key clinical point: Transgender individuals had increased risk of breast cancer similar to a female reference population.
Major finding: Transgender men had a standardized incidence ratio of 59.8 compared to a male reference population.
Study details: Study of 3,078 transgender adults receiving hormone therapy.
Disclosures: Dr. de Blok reported no conflicts of interest.
Source: de Blok C, et al. ENDO 2018, abstract OR 25-6.
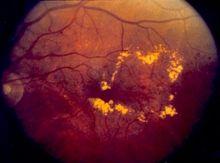
Robocalls increase diabetic retinopathy screenings in low-income patients
CHICAGO – according to a presentation at the annual meeting of the Endocrine Society.
Patients with diabetes require routine diabetic retinopathy (DR) screenings as it is usually asymptomatic until vision loss, explained presenter Eli K. Ipp, MD, professor of medicine at the University of California, Los Angeles. Sending robocalls is an easy, relatively cheap solution to encourage patients to seek screening, especially for certain populations that may be less inclined to spend the time and money to do so.
Investigators used EHRs to randomly selected 350 patients with diabetes to receive either a prerecorded message 1-7 days ahead of an existing appointment or a phone call from a staff member reminding patients of an upcoming appointment, during the course of 7 weeks.
Patients included were aged 54-58 years, and 70% were Hispanic and 30% were African American, with more than half this population having less than a high school education and three-quarters having an income less than $25,000.
Overall show rate for screenings was almost 14% higher in the robocall group (59.9%) than in the control group (46.3%).
Among African Americans, the program worked especially well, closing the gap with Hispanic patients, who reported attending their appointments nearly twice as often as did African American patients the previous year.
“Automated robocall reminders are an effective, potentially low-cost approach to appointment reminders in safety-net clinics,” Dr. Ipp explained to attendees. “Robocall almost eliminated the African American disparity seen with usual care in this population.”
Implementation of the robocalls is also relatively simple since the programs used to find the patients and create the calls are readily available, although investigators chose to gather the data for this study by hand, according to Dr. Ipp.
Screening rates in the United States are disconcertingly low, Dr. Ipp pointed out. While screening rates were around 70% in Medicare patients, rates among Medicaid and commercially insured patients hovered between 47.5%-54.9%, according to data collected by the National Committee for Quality Assurance.
Rates are especially low among minorities, as seen by a difference in screenings between minorities and non-Hispanic whites that ranged from 7% to15% during 2002-2009, according to a study cited by Dr. Ipp.
Dr. Ipp reported no relevant financial disclosures.
SOURCE: Mehranbod C et al. ENDO 2018, Abstract OR27-4.
CHICAGO – according to a presentation at the annual meeting of the Endocrine Society.
Patients with diabetes require routine diabetic retinopathy (DR) screenings as it is usually asymptomatic until vision loss, explained presenter Eli K. Ipp, MD, professor of medicine at the University of California, Los Angeles. Sending robocalls is an easy, relatively cheap solution to encourage patients to seek screening, especially for certain populations that may be less inclined to spend the time and money to do so.
Investigators used EHRs to randomly selected 350 patients with diabetes to receive either a prerecorded message 1-7 days ahead of an existing appointment or a phone call from a staff member reminding patients of an upcoming appointment, during the course of 7 weeks.
Patients included were aged 54-58 years, and 70% were Hispanic and 30% were African American, with more than half this population having less than a high school education and three-quarters having an income less than $25,000.
Overall show rate for screenings was almost 14% higher in the robocall group (59.9%) than in the control group (46.3%).
Among African Americans, the program worked especially well, closing the gap with Hispanic patients, who reported attending their appointments nearly twice as often as did African American patients the previous year.
“Automated robocall reminders are an effective, potentially low-cost approach to appointment reminders in safety-net clinics,” Dr. Ipp explained to attendees. “Robocall almost eliminated the African American disparity seen with usual care in this population.”
Implementation of the robocalls is also relatively simple since the programs used to find the patients and create the calls are readily available, although investigators chose to gather the data for this study by hand, according to Dr. Ipp.
Screening rates in the United States are disconcertingly low, Dr. Ipp pointed out. While screening rates were around 70% in Medicare patients, rates among Medicaid and commercially insured patients hovered between 47.5%-54.9%, according to data collected by the National Committee for Quality Assurance.
Rates are especially low among minorities, as seen by a difference in screenings between minorities and non-Hispanic whites that ranged from 7% to15% during 2002-2009, according to a study cited by Dr. Ipp.
Dr. Ipp reported no relevant financial disclosures.
SOURCE: Mehranbod C et al. ENDO 2018, Abstract OR27-4.
CHICAGO – according to a presentation at the annual meeting of the Endocrine Society.
Patients with diabetes require routine diabetic retinopathy (DR) screenings as it is usually asymptomatic until vision loss, explained presenter Eli K. Ipp, MD, professor of medicine at the University of California, Los Angeles. Sending robocalls is an easy, relatively cheap solution to encourage patients to seek screening, especially for certain populations that may be less inclined to spend the time and money to do so.
Investigators used EHRs to randomly selected 350 patients with diabetes to receive either a prerecorded message 1-7 days ahead of an existing appointment or a phone call from a staff member reminding patients of an upcoming appointment, during the course of 7 weeks.
Patients included were aged 54-58 years, and 70% were Hispanic and 30% were African American, with more than half this population having less than a high school education and three-quarters having an income less than $25,000.
Overall show rate for screenings was almost 14% higher in the robocall group (59.9%) than in the control group (46.3%).
Among African Americans, the program worked especially well, closing the gap with Hispanic patients, who reported attending their appointments nearly twice as often as did African American patients the previous year.
“Automated robocall reminders are an effective, potentially low-cost approach to appointment reminders in safety-net clinics,” Dr. Ipp explained to attendees. “Robocall almost eliminated the African American disparity seen with usual care in this population.”
Implementation of the robocalls is also relatively simple since the programs used to find the patients and create the calls are readily available, although investigators chose to gather the data for this study by hand, according to Dr. Ipp.
Screening rates in the United States are disconcertingly low, Dr. Ipp pointed out. While screening rates were around 70% in Medicare patients, rates among Medicaid and commercially insured patients hovered between 47.5%-54.9%, according to data collected by the National Committee for Quality Assurance.
Rates are especially low among minorities, as seen by a difference in screenings between minorities and non-Hispanic whites that ranged from 7% to15% during 2002-2009, according to a study cited by Dr. Ipp.
Dr. Ipp reported no relevant financial disclosures.
SOURCE: Mehranbod C et al. ENDO 2018, Abstract OR27-4.
REPORTING FROM ENDO 2018
Key clinical point: Robocalls increase diabetic retinopathy screenings in low-income, minority patients.
Major finding: Overall rate of patients who showed up to DR screenings increased from 46.3% to 59.9% in the robocall test group (P = .036).
Data source: Controlled study of 301 patients who received a robocall over 7 weeks.
Disclosures: Dr. Ipp reported no relevant financial disclosures.
Source: Mehranbod C et al. ENDO 2018, Abstract OR27-4.
VIDEO: Adipogenic genes upregulated in high-BMI sucralose users
CHICAGO – , there was significant upregulation of genes that promote intracellular glucose transport. Genes known to be adipogenic and those governing sweet taste receptors also were significantly upregulated with sucralose exposure.
“Effects of sucralose are particularly more detrimental in obese individuals who are prediabetic or diabetic, rather than nonobese consumers of low-calorie sweetener,” said Sabyasachi Sen, MD, during a press conference at the annual meeting of the Endocrine Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
These new findings, together with in vitro examination of human adipose-derived mesenchymal stromal cells (MSCs) exposed to sucralose, are helping solve the puzzle of how a sweetener that delivers no energy may contribute to metabolic derangement, said Dr. Sen, professor of endocrinology at George Washington University in Washington.
Dr. Sen and his collaborators first exposed the MSCs to concentrations of sucralose ranging from 0 mM to 0.2 mM – a physiologic level for high sucralose consumers – to the supraphysiologic concentration of 1 mM.
The adipogenic genes CEBPa and FABP4 were upregulated in the sucralose-exposed MSCs, which also showed more intracellular fat droplet accumulation. Reactive oxygen species increased in the MSCs in a dose-dependent fashion as well, said Dr. Sen in a video interview.
All of this upregulation, said Dr. Sen, was pushing the MSCs toward becoming fat cells. “At the same time, we saw that there are certain genes that were upregulating that were allowing more glucose to enter the cell.” The increase in reactive oxygen species paralleled what was seen in a similar model that used glucose rather than sucralose, he said.
The investigators then took subcutaneous fat biopsies from four normal-weight individuals (body mass index, 23.4-24.8 kg/m2), and from 14 obese individuals (BMI, 32-64 kg/m2). Each group had sucralose users and nonusers. Using mRNA gene expression profiles, they saw that glucose transporter genes, adipogenic genes, and antioxidant genes were upregulated among sucralose consumers with obesity, significantly more than for the normal-weight participants.
The pattern, said Dr. Sen, was strikingly similar to what had been seen with the MSC-sucralose exposure findings. “The upregulation that we saw in the petri dish could now be seen in the human fat samples,” he said.
“We think that the sucralose is … allowing more glucose to enter the cell,” said Dr. Sen. “We think that we actually have figured out a mechanism.” He and his colleagues next plan to tag glucose molecules to follow what actually happens as they enter cells in the presence of sucralose.
When Dr. Sen’s patients ask whether they should switch to low-calorie sweetened beverages, he answers with an emphatic “no.” “I say, ‘It’s not going to do you any good, because it still may allow glucose to enter the cells … you’re going to come back to the same status quo’ ” in the context of obesity and insulin resistance, he said.
Dr. Sen reported that he has no relevant disclosures.
SOURCE: Sen S et al. ENDO 2018, Abstract SUN-071.
CHICAGO – , there was significant upregulation of genes that promote intracellular glucose transport. Genes known to be adipogenic and those governing sweet taste receptors also were significantly upregulated with sucralose exposure.
“Effects of sucralose are particularly more detrimental in obese individuals who are prediabetic or diabetic, rather than nonobese consumers of low-calorie sweetener,” said Sabyasachi Sen, MD, during a press conference at the annual meeting of the Endocrine Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
These new findings, together with in vitro examination of human adipose-derived mesenchymal stromal cells (MSCs) exposed to sucralose, are helping solve the puzzle of how a sweetener that delivers no energy may contribute to metabolic derangement, said Dr. Sen, professor of endocrinology at George Washington University in Washington.
Dr. Sen and his collaborators first exposed the MSCs to concentrations of sucralose ranging from 0 mM to 0.2 mM – a physiologic level for high sucralose consumers – to the supraphysiologic concentration of 1 mM.
The adipogenic genes CEBPa and FABP4 were upregulated in the sucralose-exposed MSCs, which also showed more intracellular fat droplet accumulation. Reactive oxygen species increased in the MSCs in a dose-dependent fashion as well, said Dr. Sen in a video interview.
All of this upregulation, said Dr. Sen, was pushing the MSCs toward becoming fat cells. “At the same time, we saw that there are certain genes that were upregulating that were allowing more glucose to enter the cell.” The increase in reactive oxygen species paralleled what was seen in a similar model that used glucose rather than sucralose, he said.
The investigators then took subcutaneous fat biopsies from four normal-weight individuals (body mass index, 23.4-24.8 kg/m2), and from 14 obese individuals (BMI, 32-64 kg/m2). Each group had sucralose users and nonusers. Using mRNA gene expression profiles, they saw that glucose transporter genes, adipogenic genes, and antioxidant genes were upregulated among sucralose consumers with obesity, significantly more than for the normal-weight participants.
The pattern, said Dr. Sen, was strikingly similar to what had been seen with the MSC-sucralose exposure findings. “The upregulation that we saw in the petri dish could now be seen in the human fat samples,” he said.
“We think that the sucralose is … allowing more glucose to enter the cell,” said Dr. Sen. “We think that we actually have figured out a mechanism.” He and his colleagues next plan to tag glucose molecules to follow what actually happens as they enter cells in the presence of sucralose.
When Dr. Sen’s patients ask whether they should switch to low-calorie sweetened beverages, he answers with an emphatic “no.” “I say, ‘It’s not going to do you any good, because it still may allow glucose to enter the cells … you’re going to come back to the same status quo’ ” in the context of obesity and insulin resistance, he said.
Dr. Sen reported that he has no relevant disclosures.
SOURCE: Sen S et al. ENDO 2018, Abstract SUN-071.
CHICAGO – , there was significant upregulation of genes that promote intracellular glucose transport. Genes known to be adipogenic and those governing sweet taste receptors also were significantly upregulated with sucralose exposure.
“Effects of sucralose are particularly more detrimental in obese individuals who are prediabetic or diabetic, rather than nonobese consumers of low-calorie sweetener,” said Sabyasachi Sen, MD, during a press conference at the annual meeting of the Endocrine Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
These new findings, together with in vitro examination of human adipose-derived mesenchymal stromal cells (MSCs) exposed to sucralose, are helping solve the puzzle of how a sweetener that delivers no energy may contribute to metabolic derangement, said Dr. Sen, professor of endocrinology at George Washington University in Washington.
Dr. Sen and his collaborators first exposed the MSCs to concentrations of sucralose ranging from 0 mM to 0.2 mM – a physiologic level for high sucralose consumers – to the supraphysiologic concentration of 1 mM.
The adipogenic genes CEBPa and FABP4 were upregulated in the sucralose-exposed MSCs, which also showed more intracellular fat droplet accumulation. Reactive oxygen species increased in the MSCs in a dose-dependent fashion as well, said Dr. Sen in a video interview.
All of this upregulation, said Dr. Sen, was pushing the MSCs toward becoming fat cells. “At the same time, we saw that there are certain genes that were upregulating that were allowing more glucose to enter the cell.” The increase in reactive oxygen species paralleled what was seen in a similar model that used glucose rather than sucralose, he said.
The investigators then took subcutaneous fat biopsies from four normal-weight individuals (body mass index, 23.4-24.8 kg/m2), and from 14 obese individuals (BMI, 32-64 kg/m2). Each group had sucralose users and nonusers. Using mRNA gene expression profiles, they saw that glucose transporter genes, adipogenic genes, and antioxidant genes were upregulated among sucralose consumers with obesity, significantly more than for the normal-weight participants.
The pattern, said Dr. Sen, was strikingly similar to what had been seen with the MSC-sucralose exposure findings. “The upregulation that we saw in the petri dish could now be seen in the human fat samples,” he said.
“We think that the sucralose is … allowing more glucose to enter the cell,” said Dr. Sen. “We think that we actually have figured out a mechanism.” He and his colleagues next plan to tag glucose molecules to follow what actually happens as they enter cells in the presence of sucralose.
When Dr. Sen’s patients ask whether they should switch to low-calorie sweetened beverages, he answers with an emphatic “no.” “I say, ‘It’s not going to do you any good, because it still may allow glucose to enter the cells … you’re going to come back to the same status quo’ ” in the context of obesity and insulin resistance, he said.
Dr. Sen reported that he has no relevant disclosures.
SOURCE: Sen S et al. ENDO 2018, Abstract SUN-071.
REPORTING FROM ENDO 2018
Declining androgen levels correlated with increased frailty
CHICAGO – according to a study presented at the annual meeting of the Endocrine Society.
The findings provide more evidence of the relationship between function and lower levels of androgens such as testosterone and introduce the possibility of using hormones to offset frailty in older patients.
“The decline in total and free [testosterone] and DHEA-S [dehydroepiandrosterone sulfate] was significantly associated with small deteriorations in physical function and worsening frailty,” according to presenter Frederick C. Wu, MD, an endocrinologist at the University of Manchester (England). “The present results are consistent with and support our hypothesis that the decline in these hormones can contribute to a worsening physical function and frailty in the elderly.”
Investigators gathered data on 2,278 men from eight centers across Europe to conduct an observational study of their physical functions.
Patients were all men, an average of 58 years old, and had an average body mass index of 27.6 kg/m2 and average free testosterone and DHEA-S levels at 16.9 nmol/L and 4.7 micromol/L, respectively.
At follow-up, which was on average conducted 4.4 years later, average age was 63 years, and average testosterone and DHEA-S levels had dropped to 287.3 nmol/L and 4 micromol/L respectively, which Dr. Wu described as a moderate drop.
Decreases of free testosterone or DHEA-S by one standard deviation – 86.8 nmol/L and 2.6 micromol/L, respectively – accounted for 11%-17% of the average rate of deterioration of physical function, according to Dr. Wu.
Patients with lower levels of free testosterone and DHEA-S experienced worsening 15-meter walk time, five chair-stands, physical quality of life, and overall worsening of frailty phenotypes at follow up.
Dr. Wu and his colleagues measured frailness in patients by looking for the presence of frailty phenotypes, which include slowness, sarcopenia, exhaustion, low activity, and weakness.
If one-two of these criteria were present, patients would be considered “prefrail,” and if three or more were present, patients would be deemed “frail.”
Patients experienced an average 2.5% increase in frailty per year during the time between baseline and follow up, Dr. Wu told attendees.
Investigators used the mean of 60 years old to adjust for age, Dr. Wu explained in response to a question from the audience; however, this may have been an overadjustment as free testosterone and DHEA-S are age dependent, Dr. Wu admitted.
Investigators also incorporated a frailty index of 39 health deficits – 16 physical or cognitive, 11 comorbidities, and 12 clinical – measuring on a 0-1 scale in order to measure different levels of frailty.
While the link between these androgens and frailty are evident, the potential benefits of hormonal intervention in elderly men are still in the air and demand further study.
“The decline in androgen levels in the physiological range, because of the modest degree of change, is unlikely to be the single greatest cause of deterioration in the majority of aging men in the population,” said Dr. Wu. “Therefore, the possible therapeutic roles of androgens in improving physical health may be limited to a minority of men with very low levels of testosterone.”
Dr. Wu is on the advisory board of Bayer-Schering, Eli Lilly, and Besins Healthcare. Dr. Wu is a research supporter or consultant for Repros Therapeutics, Merck Serono, and Mereo Biopharma. Investigators reported no additional relevant financial disclosures.
SOURCE: Wu F C et al. ENDO 2018, Abstract OR15-1.
CHICAGO – according to a study presented at the annual meeting of the Endocrine Society.
The findings provide more evidence of the relationship between function and lower levels of androgens such as testosterone and introduce the possibility of using hormones to offset frailty in older patients.
“The decline in total and free [testosterone] and DHEA-S [dehydroepiandrosterone sulfate] was significantly associated with small deteriorations in physical function and worsening frailty,” according to presenter Frederick C. Wu, MD, an endocrinologist at the University of Manchester (England). “The present results are consistent with and support our hypothesis that the decline in these hormones can contribute to a worsening physical function and frailty in the elderly.”
Investigators gathered data on 2,278 men from eight centers across Europe to conduct an observational study of their physical functions.
Patients were all men, an average of 58 years old, and had an average body mass index of 27.6 kg/m2 and average free testosterone and DHEA-S levels at 16.9 nmol/L and 4.7 micromol/L, respectively.
At follow-up, which was on average conducted 4.4 years later, average age was 63 years, and average testosterone and DHEA-S levels had dropped to 287.3 nmol/L and 4 micromol/L respectively, which Dr. Wu described as a moderate drop.
Decreases of free testosterone or DHEA-S by one standard deviation – 86.8 nmol/L and 2.6 micromol/L, respectively – accounted for 11%-17% of the average rate of deterioration of physical function, according to Dr. Wu.
Patients with lower levels of free testosterone and DHEA-S experienced worsening 15-meter walk time, five chair-stands, physical quality of life, and overall worsening of frailty phenotypes at follow up.
Dr. Wu and his colleagues measured frailness in patients by looking for the presence of frailty phenotypes, which include slowness, sarcopenia, exhaustion, low activity, and weakness.
If one-two of these criteria were present, patients would be considered “prefrail,” and if three or more were present, patients would be deemed “frail.”
Patients experienced an average 2.5% increase in frailty per year during the time between baseline and follow up, Dr. Wu told attendees.
Investigators used the mean of 60 years old to adjust for age, Dr. Wu explained in response to a question from the audience; however, this may have been an overadjustment as free testosterone and DHEA-S are age dependent, Dr. Wu admitted.
Investigators also incorporated a frailty index of 39 health deficits – 16 physical or cognitive, 11 comorbidities, and 12 clinical – measuring on a 0-1 scale in order to measure different levels of frailty.
While the link between these androgens and frailty are evident, the potential benefits of hormonal intervention in elderly men are still in the air and demand further study.
“The decline in androgen levels in the physiological range, because of the modest degree of change, is unlikely to be the single greatest cause of deterioration in the majority of aging men in the population,” said Dr. Wu. “Therefore, the possible therapeutic roles of androgens in improving physical health may be limited to a minority of men with very low levels of testosterone.”
Dr. Wu is on the advisory board of Bayer-Schering, Eli Lilly, and Besins Healthcare. Dr. Wu is a research supporter or consultant for Repros Therapeutics, Merck Serono, and Mereo Biopharma. Investigators reported no additional relevant financial disclosures.
SOURCE: Wu F C et al. ENDO 2018, Abstract OR15-1.
CHICAGO – according to a study presented at the annual meeting of the Endocrine Society.
The findings provide more evidence of the relationship between function and lower levels of androgens such as testosterone and introduce the possibility of using hormones to offset frailty in older patients.
“The decline in total and free [testosterone] and DHEA-S [dehydroepiandrosterone sulfate] was significantly associated with small deteriorations in physical function and worsening frailty,” according to presenter Frederick C. Wu, MD, an endocrinologist at the University of Manchester (England). “The present results are consistent with and support our hypothesis that the decline in these hormones can contribute to a worsening physical function and frailty in the elderly.”
Investigators gathered data on 2,278 men from eight centers across Europe to conduct an observational study of their physical functions.
Patients were all men, an average of 58 years old, and had an average body mass index of 27.6 kg/m2 and average free testosterone and DHEA-S levels at 16.9 nmol/L and 4.7 micromol/L, respectively.
At follow-up, which was on average conducted 4.4 years later, average age was 63 years, and average testosterone and DHEA-S levels had dropped to 287.3 nmol/L and 4 micromol/L respectively, which Dr. Wu described as a moderate drop.
Decreases of free testosterone or DHEA-S by one standard deviation – 86.8 nmol/L and 2.6 micromol/L, respectively – accounted for 11%-17% of the average rate of deterioration of physical function, according to Dr. Wu.
Patients with lower levels of free testosterone and DHEA-S experienced worsening 15-meter walk time, five chair-stands, physical quality of life, and overall worsening of frailty phenotypes at follow up.
Dr. Wu and his colleagues measured frailness in patients by looking for the presence of frailty phenotypes, which include slowness, sarcopenia, exhaustion, low activity, and weakness.
If one-two of these criteria were present, patients would be considered “prefrail,” and if three or more were present, patients would be deemed “frail.”
Patients experienced an average 2.5% increase in frailty per year during the time between baseline and follow up, Dr. Wu told attendees.
Investigators used the mean of 60 years old to adjust for age, Dr. Wu explained in response to a question from the audience; however, this may have been an overadjustment as free testosterone and DHEA-S are age dependent, Dr. Wu admitted.
Investigators also incorporated a frailty index of 39 health deficits – 16 physical or cognitive, 11 comorbidities, and 12 clinical – measuring on a 0-1 scale in order to measure different levels of frailty.
While the link between these androgens and frailty are evident, the potential benefits of hormonal intervention in elderly men are still in the air and demand further study.
“The decline in androgen levels in the physiological range, because of the modest degree of change, is unlikely to be the single greatest cause of deterioration in the majority of aging men in the population,” said Dr. Wu. “Therefore, the possible therapeutic roles of androgens in improving physical health may be limited to a minority of men with very low levels of testosterone.”
Dr. Wu is on the advisory board of Bayer-Schering, Eli Lilly, and Besins Healthcare. Dr. Wu is a research supporter or consultant for Repros Therapeutics, Merck Serono, and Mereo Biopharma. Investigators reported no additional relevant financial disclosures.
SOURCE: Wu F C et al. ENDO 2018, Abstract OR15-1.
REPORTING FROM ENDO 2018
Key clinical point: Declining androgen levels correlates with lower physical function in elder men.
Major finding: Decline in testosterone by one standard deviation accounted for 11%-17% of the average population rate of physical function deterioration.
Data source: Prospective study of 2,278 men gathered from eight European centers.
Disclosures: Frederick C. Wu is on the advisory board of Bayer-Schering, Eli Lilly, and Besins Healthcare. Dr. Wu is a research supporter or consultant for Repros Therapeutics, Merck Serono, and Mereo Biopharma.
Source: Wu F C et al. ENDO 2018 OR15-1.
VIDEO: Women living with HIV have more myocardial steatosis, reduced diastolic function
CHICAGO – Median intramyocardial triglyceride content was nearly four times higher in a group of middle-age women living with HIV, compared with peers without the infection, according to a recent study that also found an association between high myocardial lipids and lower diastolic function.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
For women without HIV, the value was 0.13% (95% CI, 0.11-0.23; P = .004). Further, left atrial passive ejection fraction was significantly lower among women living with HIV, compared with those without HIV (28% vs. 38%, P = .02), said Mabel Toribio, MD, speaking at the annual meeting of the Endocrine Society.
“Probably the most important aspect is that we found an inverse relationship between the intramyocardial triglyceride content and the diastolic function; the higher the intracardiac lipid content of the women living with HIV, the worse their cardiac function,” Dr. Toribio said in an interview. She and her colleagues at Massachusetts General Hospital, Boston, where she is a clinical investigator, found a Spearman’s rank coefficient of –0.51 for the correlation (P = .03)
“The reason that this is important is that individuals with HIV do have an increased risk of heart failure,” said Dr. Toribio. People living with HIV have a hazard ratio for heart failure that ranges from about 1.2 to 1.7, she said.
For women living with HIV with heart failure, about 70% have heart failure with preserved ejection fraction (HFpEF), which is associated with diastolic dysfunction. “In women with HIV, this has been relatively understudied, and one of the mechanisms we were looking into is myocardial steatosis, where we have increased intramyocardial lipid content,” said Dr. Toribio.
“I think, certainly, our work has a lot of clinical implications,” said Dr. Toribio, noting that there are no therapies that improve survival after a diagnosis of HFpEF. In a population with increased rates of diastolic dysfunction, “It’s imperative that we understand the mechanism of this disease process in women living with HIV,” she said.
Intramyocardial lipid content was a reasonable line of inquiry, since it’s known that people living with HIV have increased deposition of fat in various organ systems, including the liver, skeletal muscle, and the heart, said Dr. Toribio. Both HIV and antiretroviral therapy can contribute to ectopic fat deposition, she said.
Women with (n = 18) and without (n = 6) HIV were matched according to age, body mass index (BMI), history of hypertension, and smoking status, said Dr. Toribio. For women with HIV, they had to be on stable antiretroviral therapy for at least 3 months and have no interruption in therapy greater than 2 weeks over the 3 months preceding enrollment.
The study excluded women who had known preexisting heart failure, diabetes, or atherosclerotic cardiovascular disease. Participants also could not be taking lipid-lowering agents or anti-inflammatory medications.
Participants were about 52 years old on average, and had a mean BMI of a little over 30 kg/m2. Lipid values did not differ significantly between groups, except that triglycerides were a mean 107 mg/dL in women living with HIV, compared with 69 mg/dL for women without HIV (P = .01).
Of the women living with HIV, 7/18 (38.5%) were white, the same number were black, and 2 were Hispanic. Three of six women without HIV were white, two were black, and one was Hispanic; racial and ethnic differences between the groups were not statistically significant overall.
Magnetic resonance spectroscopy was used to assess intramyocardial triglyceride levels, measured at the interventricular septum, a region where there’s little overlying pericardial fat.
“We found that the women living with HIV have an increased intramyocardial triglyceride content compared to women without HIV. And notably, we sought to see if there was any relationship between circulating triglyceride levels or body mass index, and there actually was no relationship between intramyocardial triglyceride content and these factors,” said Dr. Toribio in a video interview.
Next steps include two studies, said Dr. Toribio. The first is investigating whether statin therapy improves myocardial steatosis and heart function over time in women living with HIV. The second, involving the same population, is a pilot study to see if growth hormone releasing hormone – which is known to lessen visceral adiposity in people living with HIV – can reduce intramyocardial steatosis and boost cardiac function, she said.
Dr. Toribio reported no financial disclosures. The study was supported by funding from the National Institutes of Health.
SOURCE: Toribio M et al. ENDO 2018, Abstract OR11-2.
CHICAGO – Median intramyocardial triglyceride content was nearly four times higher in a group of middle-age women living with HIV, compared with peers without the infection, according to a recent study that also found an association between high myocardial lipids and lower diastolic function.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
For women without HIV, the value was 0.13% (95% CI, 0.11-0.23; P = .004). Further, left atrial passive ejection fraction was significantly lower among women living with HIV, compared with those without HIV (28% vs. 38%, P = .02), said Mabel Toribio, MD, speaking at the annual meeting of the Endocrine Society.
“Probably the most important aspect is that we found an inverse relationship between the intramyocardial triglyceride content and the diastolic function; the higher the intracardiac lipid content of the women living with HIV, the worse their cardiac function,” Dr. Toribio said in an interview. She and her colleagues at Massachusetts General Hospital, Boston, where she is a clinical investigator, found a Spearman’s rank coefficient of –0.51 for the correlation (P = .03)
“The reason that this is important is that individuals with HIV do have an increased risk of heart failure,” said Dr. Toribio. People living with HIV have a hazard ratio for heart failure that ranges from about 1.2 to 1.7, she said.
For women living with HIV with heart failure, about 70% have heart failure with preserved ejection fraction (HFpEF), which is associated with diastolic dysfunction. “In women with HIV, this has been relatively understudied, and one of the mechanisms we were looking into is myocardial steatosis, where we have increased intramyocardial lipid content,” said Dr. Toribio.
“I think, certainly, our work has a lot of clinical implications,” said Dr. Toribio, noting that there are no therapies that improve survival after a diagnosis of HFpEF. In a population with increased rates of diastolic dysfunction, “It’s imperative that we understand the mechanism of this disease process in women living with HIV,” she said.
Intramyocardial lipid content was a reasonable line of inquiry, since it’s known that people living with HIV have increased deposition of fat in various organ systems, including the liver, skeletal muscle, and the heart, said Dr. Toribio. Both HIV and antiretroviral therapy can contribute to ectopic fat deposition, she said.
Women with (n = 18) and without (n = 6) HIV were matched according to age, body mass index (BMI), history of hypertension, and smoking status, said Dr. Toribio. For women with HIV, they had to be on stable antiretroviral therapy for at least 3 months and have no interruption in therapy greater than 2 weeks over the 3 months preceding enrollment.
The study excluded women who had known preexisting heart failure, diabetes, or atherosclerotic cardiovascular disease. Participants also could not be taking lipid-lowering agents or anti-inflammatory medications.
Participants were about 52 years old on average, and had a mean BMI of a little over 30 kg/m2. Lipid values did not differ significantly between groups, except that triglycerides were a mean 107 mg/dL in women living with HIV, compared with 69 mg/dL for women without HIV (P = .01).
Of the women living with HIV, 7/18 (38.5%) were white, the same number were black, and 2 were Hispanic. Three of six women without HIV were white, two were black, and one was Hispanic; racial and ethnic differences between the groups were not statistically significant overall.
Magnetic resonance spectroscopy was used to assess intramyocardial triglyceride levels, measured at the interventricular septum, a region where there’s little overlying pericardial fat.
“We found that the women living with HIV have an increased intramyocardial triglyceride content compared to women without HIV. And notably, we sought to see if there was any relationship between circulating triglyceride levels or body mass index, and there actually was no relationship between intramyocardial triglyceride content and these factors,” said Dr. Toribio in a video interview.
Next steps include two studies, said Dr. Toribio. The first is investigating whether statin therapy improves myocardial steatosis and heart function over time in women living with HIV. The second, involving the same population, is a pilot study to see if growth hormone releasing hormone – which is known to lessen visceral adiposity in people living with HIV – can reduce intramyocardial steatosis and boost cardiac function, she said.
Dr. Toribio reported no financial disclosures. The study was supported by funding from the National Institutes of Health.
SOURCE: Toribio M et al. ENDO 2018, Abstract OR11-2.
CHICAGO – Median intramyocardial triglyceride content was nearly four times higher in a group of middle-age women living with HIV, compared with peers without the infection, according to a recent study that also found an association between high myocardial lipids and lower diastolic function.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
For women without HIV, the value was 0.13% (95% CI, 0.11-0.23; P = .004). Further, left atrial passive ejection fraction was significantly lower among women living with HIV, compared with those without HIV (28% vs. 38%, P = .02), said Mabel Toribio, MD, speaking at the annual meeting of the Endocrine Society.
“Probably the most important aspect is that we found an inverse relationship between the intramyocardial triglyceride content and the diastolic function; the higher the intracardiac lipid content of the women living with HIV, the worse their cardiac function,” Dr. Toribio said in an interview. She and her colleagues at Massachusetts General Hospital, Boston, where she is a clinical investigator, found a Spearman’s rank coefficient of –0.51 for the correlation (P = .03)
“The reason that this is important is that individuals with HIV do have an increased risk of heart failure,” said Dr. Toribio. People living with HIV have a hazard ratio for heart failure that ranges from about 1.2 to 1.7, she said.
For women living with HIV with heart failure, about 70% have heart failure with preserved ejection fraction (HFpEF), which is associated with diastolic dysfunction. “In women with HIV, this has been relatively understudied, and one of the mechanisms we were looking into is myocardial steatosis, where we have increased intramyocardial lipid content,” said Dr. Toribio.
“I think, certainly, our work has a lot of clinical implications,” said Dr. Toribio, noting that there are no therapies that improve survival after a diagnosis of HFpEF. In a population with increased rates of diastolic dysfunction, “It’s imperative that we understand the mechanism of this disease process in women living with HIV,” she said.
Intramyocardial lipid content was a reasonable line of inquiry, since it’s known that people living with HIV have increased deposition of fat in various organ systems, including the liver, skeletal muscle, and the heart, said Dr. Toribio. Both HIV and antiretroviral therapy can contribute to ectopic fat deposition, she said.
Women with (n = 18) and without (n = 6) HIV were matched according to age, body mass index (BMI), history of hypertension, and smoking status, said Dr. Toribio. For women with HIV, they had to be on stable antiretroviral therapy for at least 3 months and have no interruption in therapy greater than 2 weeks over the 3 months preceding enrollment.
The study excluded women who had known preexisting heart failure, diabetes, or atherosclerotic cardiovascular disease. Participants also could not be taking lipid-lowering agents or anti-inflammatory medications.
Participants were about 52 years old on average, and had a mean BMI of a little over 30 kg/m2. Lipid values did not differ significantly between groups, except that triglycerides were a mean 107 mg/dL in women living with HIV, compared with 69 mg/dL for women without HIV (P = .01).
Of the women living with HIV, 7/18 (38.5%) were white, the same number were black, and 2 were Hispanic. Three of six women without HIV were white, two were black, and one was Hispanic; racial and ethnic differences between the groups were not statistically significant overall.
Magnetic resonance spectroscopy was used to assess intramyocardial triglyceride levels, measured at the interventricular septum, a region where there’s little overlying pericardial fat.
“We found that the women living with HIV have an increased intramyocardial triglyceride content compared to women without HIV. And notably, we sought to see if there was any relationship between circulating triglyceride levels or body mass index, and there actually was no relationship between intramyocardial triglyceride content and these factors,” said Dr. Toribio in a video interview.
Next steps include two studies, said Dr. Toribio. The first is investigating whether statin therapy improves myocardial steatosis and heart function over time in women living with HIV. The second, involving the same population, is a pilot study to see if growth hormone releasing hormone – which is known to lessen visceral adiposity in people living with HIV – can reduce intramyocardial steatosis and boost cardiac function, she said.
Dr. Toribio reported no financial disclosures. The study was supported by funding from the National Institutes of Health.
SOURCE: Toribio M et al. ENDO 2018, Abstract OR11-2.
REPORTING FROM ENDO 2018
Oral SGLT-2 inhibitor reduced liver fat in diabetics with NAFLD
CHICAGO – and improved ALT in patients with nonalcoholic fatty liver disease (NAFLD) and type 2 diabetes mellitus, according to a study presented at the annual meeting of the Endocrine Society.
As insulin resistance is the mechanism for NAFLD development, this new addition to the list of drugs on offer to patients with diabetes could help decrease the chance of developing metabolic syndrome and cardiovascular disease.
“SGLT-2 inhibitors are newer antidiabetic agents that reduce blood glucose by promoting urinary glucose excretion,” said presenter Mohammad Shafi Kuchay, MD, DM, an endocrinologist at Medanta The Medicity, Gurugram, India. “NAFLD, which also increases the risk of type 2 diabetes, often responds to strategies that improve hyperglycemia.”
Dr. Kuchay and fellow investigators conducted a small, 20-week randomized controlled trial of 42 patients with type 2 diabetes and NAFLD.
Patients in the test group were mostly male and on average 50 years old, with baseline AST, ALT, and gamma-glutamyltransferase scores of 44.6 U/L, 64.3 U/L, and 65.8 U/L, respectively. Those randomized to the control group had similar characteristics.
After adding 10 mg of empagliflozin to their diabetes regimen, liver fat density in test patients decreased from 16.2% to 11.3% (P less than or equal to .0001). The drop stands in sharp contrast to the control group, which decreased from 16.4% to 15.5% (P = .054). Measurement of liver fat density was made by MRI-derived proton density fat fraction (MRI-PDFF). This method has higher sensitivity for detecting changes in liver fat, compared with histology, explained Dr. Kuchay.
When broken down by individual liver fat, 25% of patients in the control group increased in liver fat, 50% had no significant change, and 25% decreased in liver fat, according to Dr. Kuchay.
In comparison, 77% of patients in the empagliflozin group had a decrease in liver fat, 23% had no change, and no patients saw an increase in liver fat.
When comparing levels of hemoglobin A1c between the two groups, both had a similarly significant reduction of around 2%, which Dr. Kuchay attributes to deliberate intervention by investigators.
Further studies will need to be conducted regarding the long-term effects of this treatment; however, using SGLT-2 to reduce liver fat could be a boon to preventing more serious liver diseases, concluded Dr. Kuchay.
“There are studies in which liver fat reduction led to improvement in inflammation and fibrosis,” said Dr. Kuchay in response to a question from the audience. “Because liver fat accumulation is the first inhibitor in the pathogenesis of more severe forms of liver disease, reducing liver fat should help improve patient outcomes.”
Dr. Kuchay reported no relevant financial disclosures.
Source: M. Kuchay et al. ENDO 2018, Abstract OR27-2.
CHICAGO – and improved ALT in patients with nonalcoholic fatty liver disease (NAFLD) and type 2 diabetes mellitus, according to a study presented at the annual meeting of the Endocrine Society.
As insulin resistance is the mechanism for NAFLD development, this new addition to the list of drugs on offer to patients with diabetes could help decrease the chance of developing metabolic syndrome and cardiovascular disease.
“SGLT-2 inhibitors are newer antidiabetic agents that reduce blood glucose by promoting urinary glucose excretion,” said presenter Mohammad Shafi Kuchay, MD, DM, an endocrinologist at Medanta The Medicity, Gurugram, India. “NAFLD, which also increases the risk of type 2 diabetes, often responds to strategies that improve hyperglycemia.”
Dr. Kuchay and fellow investigators conducted a small, 20-week randomized controlled trial of 42 patients with type 2 diabetes and NAFLD.
Patients in the test group were mostly male and on average 50 years old, with baseline AST, ALT, and gamma-glutamyltransferase scores of 44.6 U/L, 64.3 U/L, and 65.8 U/L, respectively. Those randomized to the control group had similar characteristics.
After adding 10 mg of empagliflozin to their diabetes regimen, liver fat density in test patients decreased from 16.2% to 11.3% (P less than or equal to .0001). The drop stands in sharp contrast to the control group, which decreased from 16.4% to 15.5% (P = .054). Measurement of liver fat density was made by MRI-derived proton density fat fraction (MRI-PDFF). This method has higher sensitivity for detecting changes in liver fat, compared with histology, explained Dr. Kuchay.
When broken down by individual liver fat, 25% of patients in the control group increased in liver fat, 50% had no significant change, and 25% decreased in liver fat, according to Dr. Kuchay.
In comparison, 77% of patients in the empagliflozin group had a decrease in liver fat, 23% had no change, and no patients saw an increase in liver fat.
When comparing levels of hemoglobin A1c between the two groups, both had a similarly significant reduction of around 2%, which Dr. Kuchay attributes to deliberate intervention by investigators.
Further studies will need to be conducted regarding the long-term effects of this treatment; however, using SGLT-2 to reduce liver fat could be a boon to preventing more serious liver diseases, concluded Dr. Kuchay.
“There are studies in which liver fat reduction led to improvement in inflammation and fibrosis,” said Dr. Kuchay in response to a question from the audience. “Because liver fat accumulation is the first inhibitor in the pathogenesis of more severe forms of liver disease, reducing liver fat should help improve patient outcomes.”
Dr. Kuchay reported no relevant financial disclosures.
Source: M. Kuchay et al. ENDO 2018, Abstract OR27-2.
CHICAGO – and improved ALT in patients with nonalcoholic fatty liver disease (NAFLD) and type 2 diabetes mellitus, according to a study presented at the annual meeting of the Endocrine Society.
As insulin resistance is the mechanism for NAFLD development, this new addition to the list of drugs on offer to patients with diabetes could help decrease the chance of developing metabolic syndrome and cardiovascular disease.
“SGLT-2 inhibitors are newer antidiabetic agents that reduce blood glucose by promoting urinary glucose excretion,” said presenter Mohammad Shafi Kuchay, MD, DM, an endocrinologist at Medanta The Medicity, Gurugram, India. “NAFLD, which also increases the risk of type 2 diabetes, often responds to strategies that improve hyperglycemia.”
Dr. Kuchay and fellow investigators conducted a small, 20-week randomized controlled trial of 42 patients with type 2 diabetes and NAFLD.
Patients in the test group were mostly male and on average 50 years old, with baseline AST, ALT, and gamma-glutamyltransferase scores of 44.6 U/L, 64.3 U/L, and 65.8 U/L, respectively. Those randomized to the control group had similar characteristics.
After adding 10 mg of empagliflozin to their diabetes regimen, liver fat density in test patients decreased from 16.2% to 11.3% (P less than or equal to .0001). The drop stands in sharp contrast to the control group, which decreased from 16.4% to 15.5% (P = .054). Measurement of liver fat density was made by MRI-derived proton density fat fraction (MRI-PDFF). This method has higher sensitivity for detecting changes in liver fat, compared with histology, explained Dr. Kuchay.
When broken down by individual liver fat, 25% of patients in the control group increased in liver fat, 50% had no significant change, and 25% decreased in liver fat, according to Dr. Kuchay.
In comparison, 77% of patients in the empagliflozin group had a decrease in liver fat, 23% had no change, and no patients saw an increase in liver fat.
When comparing levels of hemoglobin A1c between the two groups, both had a similarly significant reduction of around 2%, which Dr. Kuchay attributes to deliberate intervention by investigators.
Further studies will need to be conducted regarding the long-term effects of this treatment; however, using SGLT-2 to reduce liver fat could be a boon to preventing more serious liver diseases, concluded Dr. Kuchay.
“There are studies in which liver fat reduction led to improvement in inflammation and fibrosis,” said Dr. Kuchay in response to a question from the audience. “Because liver fat accumulation is the first inhibitor in the pathogenesis of more severe forms of liver disease, reducing liver fat should help improve patient outcomes.”
Dr. Kuchay reported no relevant financial disclosures.
Source: M. Kuchay et al. ENDO 2018, Abstract OR27-2.
REPORTING FROM ENDO 2018
Key clinical point: Empagliflozin reduced liver fat in patients with NAFLD and type 2 diabetes.
Major finding: MRI-PDFF in test patients decreased from 16.2% to 11.3% (P less than or equal to .0001), compared with control patients, who saw a decrease from 19.4% to 15.5% (P = .057)
Data source: Prospective, randomized, controlled trial of 60 patients with type 2 diabetes and NAFLD.
Disclosures: Dr. Kuchay reported no relevant financial disclosures.
Source: Kuchay M et al. ENDO 2018, Abstract OR27-2.
VIDEO: Researchers closing in on the elusive ‘male pill’
CHICAGO –
It blocks gonadotropin signaling and testosterone production in the testes. When capsules ranging in dose from 100 mg to 400 mg were given once daily to 100 men in a randomized, placebo controlled trial, the drop in testosterone was more than sufficient to block sperm production. Testosterone levels jumped back up to normal after the end of the 28-day trial, all without inducing liver toxicity or other serious problems.
“We are very excited [about] the results. It’s a big step forward in the development of the male pill. Our last great advance in male contraception was over 300 years ago with the development of the condom,” said senior investigator Stephanie Page, MD, PhD, head of the division of metabolism, endocrinology, and nutrition at the University of Washington, Seattle.
Some men reported a drop in libido that resolved by the end of the study. There was also mild weight gain and small reductions in HDL cholesterol. A few tweaks to the formulation or dosing might fix those problems. “Overall, we were very encouraged about the safety profile,” Dr. Page said.
She explained the work, its promise, and the next steps in a video interview at the Endocrine Society’s annual meeting. The National Institutes of Health is funding development. Dr. Page didn’t have any relevant disclosures.
SOURCE: Page S et al. ENDO 2018, Abstract OR15-2.
CHICAGO –
It blocks gonadotropin signaling and testosterone production in the testes. When capsules ranging in dose from 100 mg to 400 mg were given once daily to 100 men in a randomized, placebo controlled trial, the drop in testosterone was more than sufficient to block sperm production. Testosterone levels jumped back up to normal after the end of the 28-day trial, all without inducing liver toxicity or other serious problems.
“We are very excited [about] the results. It’s a big step forward in the development of the male pill. Our last great advance in male contraception was over 300 years ago with the development of the condom,” said senior investigator Stephanie Page, MD, PhD, head of the division of metabolism, endocrinology, and nutrition at the University of Washington, Seattle.
Some men reported a drop in libido that resolved by the end of the study. There was also mild weight gain and small reductions in HDL cholesterol. A few tweaks to the formulation or dosing might fix those problems. “Overall, we were very encouraged about the safety profile,” Dr. Page said.
She explained the work, its promise, and the next steps in a video interview at the Endocrine Society’s annual meeting. The National Institutes of Health is funding development. Dr. Page didn’t have any relevant disclosures.
SOURCE: Page S et al. ENDO 2018, Abstract OR15-2.
CHICAGO –
It blocks gonadotropin signaling and testosterone production in the testes. When capsules ranging in dose from 100 mg to 400 mg were given once daily to 100 men in a randomized, placebo controlled trial, the drop in testosterone was more than sufficient to block sperm production. Testosterone levels jumped back up to normal after the end of the 28-day trial, all without inducing liver toxicity or other serious problems.
“We are very excited [about] the results. It’s a big step forward in the development of the male pill. Our last great advance in male contraception was over 300 years ago with the development of the condom,” said senior investigator Stephanie Page, MD, PhD, head of the division of metabolism, endocrinology, and nutrition at the University of Washington, Seattle.
Some men reported a drop in libido that resolved by the end of the study. There was also mild weight gain and small reductions in HDL cholesterol. A few tweaks to the formulation or dosing might fix those problems. “Overall, we were very encouraged about the safety profile,” Dr. Page said.
She explained the work, its promise, and the next steps in a video interview at the Endocrine Society’s annual meeting. The National Institutes of Health is funding development. Dr. Page didn’t have any relevant disclosures.
SOURCE: Page S et al. ENDO 2018, Abstract OR15-2.
REPORTING FROM ENDO 2018
VIDEO: Stem cells may reverse premature menopause, restore fertility
CHICAGO –
Neither of the women had menstruated for about 5 years; both were in premature menopause and wanted desperately to start a family. Estrogen levels began increasing soon after treatment, and night sweats and other symptoms of menopause almost disappeared. After a year, the treated ovary was almost the size of a normal premenopausal ovary. There weren’t any complications or side effects, and both women are now pursuing pregnancy.
The results are “very exciting, very encouraging,” said senior investigator Ayman Al-Hendy, MD, PhD, a gynecology professor at the University of Illinois at Chicago.
“The eggs are there, but they are not active.” Something about the stem cells seems “to activate these eggs to become fertilizable,” he said.
Far more work is planned on the project, and there’s no shortage of volunteers; premature menopause is a devastating diagnosis to young women hoping to start families.
Dr. Al-Hendy explained the procedure and the next steps in a video interview at the Endocrine Society annual meeting.
The work is supported by MD Stem Cells and the National Institutes of Health. Dr. Al-Hendy didn’t have any relevant disclosures.
SOURCE: Al-Hendy A et al. ENDO 2018, Abstract OR33-6.
CHICAGO –
Neither of the women had menstruated for about 5 years; both were in premature menopause and wanted desperately to start a family. Estrogen levels began increasing soon after treatment, and night sweats and other symptoms of menopause almost disappeared. After a year, the treated ovary was almost the size of a normal premenopausal ovary. There weren’t any complications or side effects, and both women are now pursuing pregnancy.
The results are “very exciting, very encouraging,” said senior investigator Ayman Al-Hendy, MD, PhD, a gynecology professor at the University of Illinois at Chicago.
“The eggs are there, but they are not active.” Something about the stem cells seems “to activate these eggs to become fertilizable,” he said.
Far more work is planned on the project, and there’s no shortage of volunteers; premature menopause is a devastating diagnosis to young women hoping to start families.
Dr. Al-Hendy explained the procedure and the next steps in a video interview at the Endocrine Society annual meeting.
The work is supported by MD Stem Cells and the National Institutes of Health. Dr. Al-Hendy didn’t have any relevant disclosures.
SOURCE: Al-Hendy A et al. ENDO 2018, Abstract OR33-6.
CHICAGO –
Neither of the women had menstruated for about 5 years; both were in premature menopause and wanted desperately to start a family. Estrogen levels began increasing soon after treatment, and night sweats and other symptoms of menopause almost disappeared. After a year, the treated ovary was almost the size of a normal premenopausal ovary. There weren’t any complications or side effects, and both women are now pursuing pregnancy.
The results are “very exciting, very encouraging,” said senior investigator Ayman Al-Hendy, MD, PhD, a gynecology professor at the University of Illinois at Chicago.
“The eggs are there, but they are not active.” Something about the stem cells seems “to activate these eggs to become fertilizable,” he said.
Far more work is planned on the project, and there’s no shortage of volunteers; premature menopause is a devastating diagnosis to young women hoping to start families.
Dr. Al-Hendy explained the procedure and the next steps in a video interview at the Endocrine Society annual meeting.
The work is supported by MD Stem Cells and the National Institutes of Health. Dr. Al-Hendy didn’t have any relevant disclosures.
SOURCE: Al-Hendy A et al. ENDO 2018, Abstract OR33-6.
REPORTING FROM ENDO 2018
VIDEO: Fezolinetant drops testosterone levels in PCOS
CHICAGO – currently in development. The proof-of-concept phase 2 trial, which saw no concerning safety signals for the medication, fezolinetant, sets the stage for a larger, and perhaps longer, study to learn more about the neurokinin 3 receptor antagonist’s efficacy against PCOS.
“The primary outcome for this phase 2 trial was to see if we could lower testosterone levels in these PCOS patients,” said Graeme Fraser, PhD, chief scientific officer for Ogeda, discussing the poster he and his colleagues presented at the annual meeting of the Endocrine Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Testosterone levels decreased: Measured at about 3 hours postdose, which is the approximate pharmacokinetic Cmax [maximum serum concentration], there was … a more than 30% decrease in testosterone levels,” said Dr. Fraser. By week 12, he said, “there was a very consistent decrease of 30% of testosterone levels. So that was quite good; we successfully hit the primary outcome.”
At 12 weeks, the higher dose of fezolinetant decreased testosterone by 0.64 nmol/L, compared with the 0.04 nmol/L seen with placebo (P less than .01).
Fezolinetant downregulates the activity of candy neurons in the hypothalamus, said Dr. Fraser in an interview. In turn, gonadotropin-releasing hormone (GNRH) pulse frequency is reduced, lowering luteinizing hormone (LH) levels. Since LH drives testosterone levels, this drops as well – a beneficial effect in PCOS, with its cardinal symptom of hyperandrogenism.
The double-blind, placebo-controlled study was conducted in Western Europe; 73 participants were randomized into three groups: 27 to a placebo group, 23 to a treatment group given 60 mg of fezolinetant once daily, and 23 to a treatment group given 180 mg of fezolinetant once daily. All groups received treatment for 12 weeks.
A total of 26 patients on placebo, 21 on 60-mg fezolinetant, and 17 on 180-mg fezolinetant completed the study. Patients who completed the study were included in the safety analysis, while all who took the study medication were included in the intent-to-treat analysis for primary and secondary outcome measures.
All participants had PCOS with hyperandrogenism, mean age was about 31 years, and about three quarters of enrollees were white, though local regulations restricted the collection of race and ethnicity data in some cases. One secondary outcome measure of the study was how fezolinetant affected the LH:FSH (follicle-stimulating hormone) ratio. “Patients with PCOS tend to have a very high GNRH [gonadotropin-releasing hormone] pulse frequency, which leads to a very high LH:FSH ratio,” said Dr. Fraser.
At baseline, the LH:FSH ratio was about 3. “With treatment, that ratio normalized to about 1, which is where it is in healthy women,” he said. The decrease in LH:FSH ratio occurred in a dose-dependent fashion and was statistically significant (P less than .001 for 180 mg fezolinetant versus placebo).
Dr. Fraser and his collaborators also tracked anti-müllerian hormone (AMH) levels, ovarian volume, and number of follicles. Although the investigators saw trends toward reduction in AMH levels and toward smaller ovarian volumes, these trends weren’t significant. “It was somewhat ambitious, I guess, to consider we’d hit these endpoints within 12 weeks,” he said. There were no serious drug-related adverse events.
“Most importantly, I would say, we did not get an increase in menses frequency, and, of course, that’s an important marker for fertility,” said Dr. Fraser. “There’s a debate in PCOS about whether this disease is driven by a malfunction in the brain or a malfunction in the ovaries. I guess on face value, perhaps this problem is in the ovaries.”
With the trends toward lower AMH and ovarian volumes, the research team is left wondering what would happen if the duration of therapy were extended. “Perhaps, the system would have been reset, and the frequency would have been restored. … So one thought that we have is to prolong the study in future trials and see if that could lead to an increase in fertility in PCOS,” said Dr. Fraser.
Fezolinetant is also being studied for menopause-related hot flashes in the United States and Europe.
Dr. Fraser is an employee of Ogeda, which sponsored the trial. Ogeda is a wholly owned subsidiary of Astelas.
SOURCE: Fraser G et al. ENDO 2018, Abstract SAT-305-LB.
CHICAGO – currently in development. The proof-of-concept phase 2 trial, which saw no concerning safety signals for the medication, fezolinetant, sets the stage for a larger, and perhaps longer, study to learn more about the neurokinin 3 receptor antagonist’s efficacy against PCOS.
“The primary outcome for this phase 2 trial was to see if we could lower testosterone levels in these PCOS patients,” said Graeme Fraser, PhD, chief scientific officer for Ogeda, discussing the poster he and his colleagues presented at the annual meeting of the Endocrine Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Testosterone levels decreased: Measured at about 3 hours postdose, which is the approximate pharmacokinetic Cmax [maximum serum concentration], there was … a more than 30% decrease in testosterone levels,” said Dr. Fraser. By week 12, he said, “there was a very consistent decrease of 30% of testosterone levels. So that was quite good; we successfully hit the primary outcome.”
At 12 weeks, the higher dose of fezolinetant decreased testosterone by 0.64 nmol/L, compared with the 0.04 nmol/L seen with placebo (P less than .01).
Fezolinetant downregulates the activity of candy neurons in the hypothalamus, said Dr. Fraser in an interview. In turn, gonadotropin-releasing hormone (GNRH) pulse frequency is reduced, lowering luteinizing hormone (LH) levels. Since LH drives testosterone levels, this drops as well – a beneficial effect in PCOS, with its cardinal symptom of hyperandrogenism.
The double-blind, placebo-controlled study was conducted in Western Europe; 73 participants were randomized into three groups: 27 to a placebo group, 23 to a treatment group given 60 mg of fezolinetant once daily, and 23 to a treatment group given 180 mg of fezolinetant once daily. All groups received treatment for 12 weeks.
A total of 26 patients on placebo, 21 on 60-mg fezolinetant, and 17 on 180-mg fezolinetant completed the study. Patients who completed the study were included in the safety analysis, while all who took the study medication were included in the intent-to-treat analysis for primary and secondary outcome measures.
All participants had PCOS with hyperandrogenism, mean age was about 31 years, and about three quarters of enrollees were white, though local regulations restricted the collection of race and ethnicity data in some cases. One secondary outcome measure of the study was how fezolinetant affected the LH:FSH (follicle-stimulating hormone) ratio. “Patients with PCOS tend to have a very high GNRH [gonadotropin-releasing hormone] pulse frequency, which leads to a very high LH:FSH ratio,” said Dr. Fraser.
At baseline, the LH:FSH ratio was about 3. “With treatment, that ratio normalized to about 1, which is where it is in healthy women,” he said. The decrease in LH:FSH ratio occurred in a dose-dependent fashion and was statistically significant (P less than .001 for 180 mg fezolinetant versus placebo).
Dr. Fraser and his collaborators also tracked anti-müllerian hormone (AMH) levels, ovarian volume, and number of follicles. Although the investigators saw trends toward reduction in AMH levels and toward smaller ovarian volumes, these trends weren’t significant. “It was somewhat ambitious, I guess, to consider we’d hit these endpoints within 12 weeks,” he said. There were no serious drug-related adverse events.
“Most importantly, I would say, we did not get an increase in menses frequency, and, of course, that’s an important marker for fertility,” said Dr. Fraser. “There’s a debate in PCOS about whether this disease is driven by a malfunction in the brain or a malfunction in the ovaries. I guess on face value, perhaps this problem is in the ovaries.”
With the trends toward lower AMH and ovarian volumes, the research team is left wondering what would happen if the duration of therapy were extended. “Perhaps, the system would have been reset, and the frequency would have been restored. … So one thought that we have is to prolong the study in future trials and see if that could lead to an increase in fertility in PCOS,” said Dr. Fraser.
Fezolinetant is also being studied for menopause-related hot flashes in the United States and Europe.
Dr. Fraser is an employee of Ogeda, which sponsored the trial. Ogeda is a wholly owned subsidiary of Astelas.
SOURCE: Fraser G et al. ENDO 2018, Abstract SAT-305-LB.
CHICAGO – currently in development. The proof-of-concept phase 2 trial, which saw no concerning safety signals for the medication, fezolinetant, sets the stage for a larger, and perhaps longer, study to learn more about the neurokinin 3 receptor antagonist’s efficacy against PCOS.
“The primary outcome for this phase 2 trial was to see if we could lower testosterone levels in these PCOS patients,” said Graeme Fraser, PhD, chief scientific officer for Ogeda, discussing the poster he and his colleagues presented at the annual meeting of the Endocrine Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Testosterone levels decreased: Measured at about 3 hours postdose, which is the approximate pharmacokinetic Cmax [maximum serum concentration], there was … a more than 30% decrease in testosterone levels,” said Dr. Fraser. By week 12, he said, “there was a very consistent decrease of 30% of testosterone levels. So that was quite good; we successfully hit the primary outcome.”
At 12 weeks, the higher dose of fezolinetant decreased testosterone by 0.64 nmol/L, compared with the 0.04 nmol/L seen with placebo (P less than .01).
Fezolinetant downregulates the activity of candy neurons in the hypothalamus, said Dr. Fraser in an interview. In turn, gonadotropin-releasing hormone (GNRH) pulse frequency is reduced, lowering luteinizing hormone (LH) levels. Since LH drives testosterone levels, this drops as well – a beneficial effect in PCOS, with its cardinal symptom of hyperandrogenism.
The double-blind, placebo-controlled study was conducted in Western Europe; 73 participants were randomized into three groups: 27 to a placebo group, 23 to a treatment group given 60 mg of fezolinetant once daily, and 23 to a treatment group given 180 mg of fezolinetant once daily. All groups received treatment for 12 weeks.
A total of 26 patients on placebo, 21 on 60-mg fezolinetant, and 17 on 180-mg fezolinetant completed the study. Patients who completed the study were included in the safety analysis, while all who took the study medication were included in the intent-to-treat analysis for primary and secondary outcome measures.
All participants had PCOS with hyperandrogenism, mean age was about 31 years, and about three quarters of enrollees were white, though local regulations restricted the collection of race and ethnicity data in some cases. One secondary outcome measure of the study was how fezolinetant affected the LH:FSH (follicle-stimulating hormone) ratio. “Patients with PCOS tend to have a very high GNRH [gonadotropin-releasing hormone] pulse frequency, which leads to a very high LH:FSH ratio,” said Dr. Fraser.
At baseline, the LH:FSH ratio was about 3. “With treatment, that ratio normalized to about 1, which is where it is in healthy women,” he said. The decrease in LH:FSH ratio occurred in a dose-dependent fashion and was statistically significant (P less than .001 for 180 mg fezolinetant versus placebo).
Dr. Fraser and his collaborators also tracked anti-müllerian hormone (AMH) levels, ovarian volume, and number of follicles. Although the investigators saw trends toward reduction in AMH levels and toward smaller ovarian volumes, these trends weren’t significant. “It was somewhat ambitious, I guess, to consider we’d hit these endpoints within 12 weeks,” he said. There were no serious drug-related adverse events.
“Most importantly, I would say, we did not get an increase in menses frequency, and, of course, that’s an important marker for fertility,” said Dr. Fraser. “There’s a debate in PCOS about whether this disease is driven by a malfunction in the brain or a malfunction in the ovaries. I guess on face value, perhaps this problem is in the ovaries.”
With the trends toward lower AMH and ovarian volumes, the research team is left wondering what would happen if the duration of therapy were extended. “Perhaps, the system would have been reset, and the frequency would have been restored. … So one thought that we have is to prolong the study in future trials and see if that could lead to an increase in fertility in PCOS,” said Dr. Fraser.
Fezolinetant is also being studied for menopause-related hot flashes in the United States and Europe.
Dr. Fraser is an employee of Ogeda, which sponsored the trial. Ogeda is a wholly owned subsidiary of Astelas.
SOURCE: Fraser G et al. ENDO 2018, Abstract SAT-305-LB.
REPORTING FROM ENDO 2018