User login
Healthcare Information and Management Systems Society (HIMSS): Annual Conference and Exhibition
VIDEO: Despite privacy concerns, some physicians optimistic about Google Glass
ORLANDO – Google Glass will soon be available to the public, but its future role in medicine is still hazy.
Glass, which is among the growing number of wearable technologies, has several applications to health care settings, experts say. Just last year, a surgeon at Ohio State University’s Wexner Medical Center in Columbus live-streamed an ACL procedure via his Google Glass. And most recently, Rhode Island Hospital’s emergency department began using the device’s video capabilities to consult with off-site specialists.
But Glass is not HIPAA compliant, raising patient privacy concerns and dissuading hospitals from incorporating it into their growing list of mobile technologies. Still, technology enthusiasts are charging ahead, envisioning a future in which Glass could be yet another piece in physicians’ toolkits.
At the annual meeting of the Healthcare Information and Management Systems Society, Dr. Jonathan A. Handler, chief medical information officer for M*Modal, spoke about Glass's potential in medicine.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemsmiller
ORLANDO – Google Glass will soon be available to the public, but its future role in medicine is still hazy.
Glass, which is among the growing number of wearable technologies, has several applications to health care settings, experts say. Just last year, a surgeon at Ohio State University’s Wexner Medical Center in Columbus live-streamed an ACL procedure via his Google Glass. And most recently, Rhode Island Hospital’s emergency department began using the device’s video capabilities to consult with off-site specialists.
But Glass is not HIPAA compliant, raising patient privacy concerns and dissuading hospitals from incorporating it into their growing list of mobile technologies. Still, technology enthusiasts are charging ahead, envisioning a future in which Glass could be yet another piece in physicians’ toolkits.
At the annual meeting of the Healthcare Information and Management Systems Society, Dr. Jonathan A. Handler, chief medical information officer for M*Modal, spoke about Glass's potential in medicine.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemsmiller
ORLANDO – Google Glass will soon be available to the public, but its future role in medicine is still hazy.
Glass, which is among the growing number of wearable technologies, has several applications to health care settings, experts say. Just last year, a surgeon at Ohio State University’s Wexner Medical Center in Columbus live-streamed an ACL procedure via his Google Glass. And most recently, Rhode Island Hospital’s emergency department began using the device’s video capabilities to consult with off-site specialists.
But Glass is not HIPAA compliant, raising patient privacy concerns and dissuading hospitals from incorporating it into their growing list of mobile technologies. Still, technology enthusiasts are charging ahead, envisioning a future in which Glass could be yet another piece in physicians’ toolkits.
At the annual meeting of the Healthcare Information and Management Systems Society, Dr. Jonathan A. Handler, chief medical information officer for M*Modal, spoke about Glass's potential in medicine.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemsmiller
AT HIMSS14
IT survey underlines move to mobile health
ORLANDO – Most health IT executives provided a mobile device to point-of-care clinicians in their organizations, according to the results of the third annual HIMSS Analytics Mobile Survey.
Ranging from computers on wheels to smartphones and tablets, most clinicians used the provided devices primarily to access patient information, clinical practice guidelines, and reference materials, based on the survey results released at the annual meeting of the Healthcare Information Management Systems Society.
"The mobile health market is one of the fastest-growing areas in the health IT space," said David Collins, senior director of mHIMSS, in a statement. "We recognize the growing importance of mobile technologies and its impact to transform the delivery of patient care."
The survey of health IT executives, conducted between December 2013 and January 2014, showed a projected increase in the use of tablet computers while hinting at the demise of the pager.
While 67% of the respondents said they provided pagers to their staff, only 8% said that they’ll add or expand the use of the devices. Laptop computers remained the most common (87%) mobile device provided to clinicians.
Among other findings:
• 36% of respondents said physicians in their organizations used the technology to collect data at bedside.
• Organizations were most likely to leverage mobile technology for pharmacy management, such as medication reminders, preventive support care, continuing of care, and telehealth interventions.
• 35% said that their organization provided apps for their patients for monitoring chronic conditions, physical activity, or nutrition. More than half said they were planning to update or launch new apps next year.
• 22% said that most of their data was integrated into the organization’s electronic medical records.
• 95% said they’ve used at least one security tool to secure data on mobile devices. Passwords were the most widespread form of security.
The complete survey can be viewed here.
On Twitter @naseemsmiller
ORLANDO – Most health IT executives provided a mobile device to point-of-care clinicians in their organizations, according to the results of the third annual HIMSS Analytics Mobile Survey.
Ranging from computers on wheels to smartphones and tablets, most clinicians used the provided devices primarily to access patient information, clinical practice guidelines, and reference materials, based on the survey results released at the annual meeting of the Healthcare Information Management Systems Society.
"The mobile health market is one of the fastest-growing areas in the health IT space," said David Collins, senior director of mHIMSS, in a statement. "We recognize the growing importance of mobile technologies and its impact to transform the delivery of patient care."
The survey of health IT executives, conducted between December 2013 and January 2014, showed a projected increase in the use of tablet computers while hinting at the demise of the pager.
While 67% of the respondents said they provided pagers to their staff, only 8% said that they’ll add or expand the use of the devices. Laptop computers remained the most common (87%) mobile device provided to clinicians.
Among other findings:
• 36% of respondents said physicians in their organizations used the technology to collect data at bedside.
• Organizations were most likely to leverage mobile technology for pharmacy management, such as medication reminders, preventive support care, continuing of care, and telehealth interventions.
• 35% said that their organization provided apps for their patients for monitoring chronic conditions, physical activity, or nutrition. More than half said they were planning to update or launch new apps next year.
• 22% said that most of their data was integrated into the organization’s electronic medical records.
• 95% said they’ve used at least one security tool to secure data on mobile devices. Passwords were the most widespread form of security.
The complete survey can be viewed here.
On Twitter @naseemsmiller
ORLANDO – Most health IT executives provided a mobile device to point-of-care clinicians in their organizations, according to the results of the third annual HIMSS Analytics Mobile Survey.
Ranging from computers on wheels to smartphones and tablets, most clinicians used the provided devices primarily to access patient information, clinical practice guidelines, and reference materials, based on the survey results released at the annual meeting of the Healthcare Information Management Systems Society.
"The mobile health market is one of the fastest-growing areas in the health IT space," said David Collins, senior director of mHIMSS, in a statement. "We recognize the growing importance of mobile technologies and its impact to transform the delivery of patient care."
The survey of health IT executives, conducted between December 2013 and January 2014, showed a projected increase in the use of tablet computers while hinting at the demise of the pager.
While 67% of the respondents said they provided pagers to their staff, only 8% said that they’ll add or expand the use of the devices. Laptop computers remained the most common (87%) mobile device provided to clinicians.
Among other findings:
• 36% of respondents said physicians in their organizations used the technology to collect data at bedside.
• Organizations were most likely to leverage mobile technology for pharmacy management, such as medication reminders, preventive support care, continuing of care, and telehealth interventions.
• 35% said that their organization provided apps for their patients for monitoring chronic conditions, physical activity, or nutrition. More than half said they were planning to update or launch new apps next year.
• 22% said that most of their data was integrated into the organization’s electronic medical records.
• 95% said they’ve used at least one security tool to secure data on mobile devices. Passwords were the most widespread form of security.
The complete survey can be viewed here.
On Twitter @naseemsmiller
AT HIMSS14
Flexibility – but no passes – on meaningful use Stage 2
ORLANDO – The government can be a bit more flexible on physicians meeting Stage 2 of meaningful use of electronic health records, but won’t give blanket permission to slide on deadlines.
That’s according to Marilyn Tavenner, administrator of the Centers for Medicare & Medicaid Services (CMS), who spoke Feb. 27 at the annual meeting of the Healthcare Information and Management Systems Society.
Physicians have been seeking more leeway from CMS on participating in meaningful use this year, in part because they must purchase or upgrade to the 2014 edition of certified EHR (electronic health records) technology, and in part because they must get ready to switch over to the ICD-10 coding set on Oct. 1.
Physicians who participate in meaningful use get incentive payments from Medicare or Medicaid. If they don’t participate this year, they’ll be penalized starting in 2015.
On Feb. 21, 48 physician organizations wrote to the Health and Human Services department, asking for delays in some of the deadlines for meaningful use this year and for more flexibility from the CMS.
Ms. Tavenner said that CMS officials had heard many concerns about moving forward with Stage 2, and "are sensitive to those concerns." She noted that over the past few years, the agency had delayed the start of Stage 1 and Stage 2, and most recently pushed back implementation of Stage 3 to 2017.
"But now is not the time to stop moving forward," she said. Ms. Tavenner said that it was understood that some health care providers and vendors "may legitimately have issues with establishing Stage 2 reporting deadlines."
Because of that, the CMS has "decided to permit flexibility in how hardship exemptions will be granted in the 2014 reporting year," she said.
The agency will look at hardship requests case-by-case, as is required by law. And it is expected to issue further guidance on what qualifies as a hardship very soon.
But Ms. Tavenner said the agency would not give everyone a pass.
"I must stress to you that we do expect all eligible Stage 2 providers to fully meet all requirements in 2015," Ms. Tavenner said. "And I urge all of you to do everything you can to meet the Stage 2 requirements this year."
aault@frontlinemedcom.com
On Twitter @aliciaault
ORLANDO – The government can be a bit more flexible on physicians meeting Stage 2 of meaningful use of electronic health records, but won’t give blanket permission to slide on deadlines.
That’s according to Marilyn Tavenner, administrator of the Centers for Medicare & Medicaid Services (CMS), who spoke Feb. 27 at the annual meeting of the Healthcare Information and Management Systems Society.
Physicians have been seeking more leeway from CMS on participating in meaningful use this year, in part because they must purchase or upgrade to the 2014 edition of certified EHR (electronic health records) technology, and in part because they must get ready to switch over to the ICD-10 coding set on Oct. 1.
Physicians who participate in meaningful use get incentive payments from Medicare or Medicaid. If they don’t participate this year, they’ll be penalized starting in 2015.
On Feb. 21, 48 physician organizations wrote to the Health and Human Services department, asking for delays in some of the deadlines for meaningful use this year and for more flexibility from the CMS.
Ms. Tavenner said that CMS officials had heard many concerns about moving forward with Stage 2, and "are sensitive to those concerns." She noted that over the past few years, the agency had delayed the start of Stage 1 and Stage 2, and most recently pushed back implementation of Stage 3 to 2017.
"But now is not the time to stop moving forward," she said. Ms. Tavenner said that it was understood that some health care providers and vendors "may legitimately have issues with establishing Stage 2 reporting deadlines."
Because of that, the CMS has "decided to permit flexibility in how hardship exemptions will be granted in the 2014 reporting year," she said.
The agency will look at hardship requests case-by-case, as is required by law. And it is expected to issue further guidance on what qualifies as a hardship very soon.
But Ms. Tavenner said the agency would not give everyone a pass.
"I must stress to you that we do expect all eligible Stage 2 providers to fully meet all requirements in 2015," Ms. Tavenner said. "And I urge all of you to do everything you can to meet the Stage 2 requirements this year."
aault@frontlinemedcom.com
On Twitter @aliciaault
ORLANDO – The government can be a bit more flexible on physicians meeting Stage 2 of meaningful use of electronic health records, but won’t give blanket permission to slide on deadlines.
That’s according to Marilyn Tavenner, administrator of the Centers for Medicare & Medicaid Services (CMS), who spoke Feb. 27 at the annual meeting of the Healthcare Information and Management Systems Society.
Physicians have been seeking more leeway from CMS on participating in meaningful use this year, in part because they must purchase or upgrade to the 2014 edition of certified EHR (electronic health records) technology, and in part because they must get ready to switch over to the ICD-10 coding set on Oct. 1.
Physicians who participate in meaningful use get incentive payments from Medicare or Medicaid. If they don’t participate this year, they’ll be penalized starting in 2015.
On Feb. 21, 48 physician organizations wrote to the Health and Human Services department, asking for delays in some of the deadlines for meaningful use this year and for more flexibility from the CMS.
Ms. Tavenner said that CMS officials had heard many concerns about moving forward with Stage 2, and "are sensitive to those concerns." She noted that over the past few years, the agency had delayed the start of Stage 1 and Stage 2, and most recently pushed back implementation of Stage 3 to 2017.
"But now is not the time to stop moving forward," she said. Ms. Tavenner said that it was understood that some health care providers and vendors "may legitimately have issues with establishing Stage 2 reporting deadlines."
Because of that, the CMS has "decided to permit flexibility in how hardship exemptions will be granted in the 2014 reporting year," she said.
The agency will look at hardship requests case-by-case, as is required by law. And it is expected to issue further guidance on what qualifies as a hardship very soon.
But Ms. Tavenner said the agency would not give everyone a pass.
"I must stress to you that we do expect all eligible Stage 2 providers to fully meet all requirements in 2015," Ms. Tavenner said. "And I urge all of you to do everything you can to meet the Stage 2 requirements this year."
aault@frontlinemedcom.com
On Twitter @aliciaault
AT HIMSS14
CMS launches ICD-10 website for small physician practices
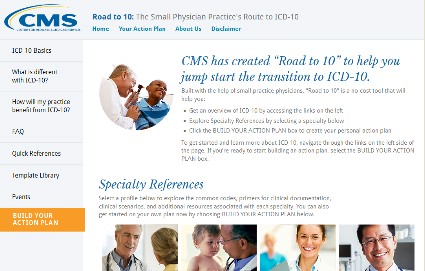
ORLANDO – A new resource is available for small practices as they prepare to switch to the ICD-10 coding system.
Officials from the Centers for Medicare & Medicaid Services (CMS) launched a new website – Road to ICD-10 – to provide a central source of basic information as well as a place to start transitioning to the new code set, which becomes mandatory on Oct. 1.
The site provides fact sheets, training videos, sample codes, and a variety of other resources. It also provides training modules that are specific to certain specialties.
Importantly, it gives physicians a template for building an action plan, said Denesecia Green, director of the Administrative Simplification Group at the CMS Office of eHealth Standards and Services.
So far, templates have been tailored for internal medicine, family practice, pediatrics, cardiology, obstetrics/gynecology, and orthopedics. The site also offers a more general path for other specialties.
According to Ms. Green, the action plan gives physicians a pictorial road map and lists the steps that might help pinpoint where diagnosis codes are used in the practice, how to identify the transition team, how to prepare a budget for the transition to ICD-10, and how to arrange for training.
The site was developed by physicians and came out of a series of listening sessions the agency held with a variety of physicians, said Dr. Ricardo Martinez, a member of the CMS’s small physician practice team, and an emergency physician.
"Physicians are concerned that everything is happening to them, rather than with them or for them," Dr. Martinez said.
However, many in the listening sessions said that they did see some potential benefits with ICD-10. In the end, Dr. Martinez said, physicians had a big question: "If there is a better world ahead, how do you get there?"
The Road to ICD-10 website is designed to help doctors make the journey, Dr. Martinez said.
The site was announced Feb. 26 at the annual meeting of the Healthcare Information and Management Systems Society (HIMSS).
On Twitter @aliciaault
ORLANDO – A new resource is available for small practices as they prepare to switch to the ICD-10 coding system.
Officials from the Centers for Medicare & Medicaid Services (CMS) launched a new website – Road to ICD-10 – to provide a central source of basic information as well as a place to start transitioning to the new code set, which becomes mandatory on Oct. 1.
The site provides fact sheets, training videos, sample codes, and a variety of other resources. It also provides training modules that are specific to certain specialties.
Importantly, it gives physicians a template for building an action plan, said Denesecia Green, director of the Administrative Simplification Group at the CMS Office of eHealth Standards and Services.
So far, templates have been tailored for internal medicine, family practice, pediatrics, cardiology, obstetrics/gynecology, and orthopedics. The site also offers a more general path for other specialties.
According to Ms. Green, the action plan gives physicians a pictorial road map and lists the steps that might help pinpoint where diagnosis codes are used in the practice, how to identify the transition team, how to prepare a budget for the transition to ICD-10, and how to arrange for training.
The site was developed by physicians and came out of a series of listening sessions the agency held with a variety of physicians, said Dr. Ricardo Martinez, a member of the CMS’s small physician practice team, and an emergency physician.
"Physicians are concerned that everything is happening to them, rather than with them or for them," Dr. Martinez said.
However, many in the listening sessions said that they did see some potential benefits with ICD-10. In the end, Dr. Martinez said, physicians had a big question: "If there is a better world ahead, how do you get there?"
The Road to ICD-10 website is designed to help doctors make the journey, Dr. Martinez said.
The site was announced Feb. 26 at the annual meeting of the Healthcare Information and Management Systems Society (HIMSS).
On Twitter @aliciaault
ORLANDO – A new resource is available for small practices as they prepare to switch to the ICD-10 coding system.
Officials from the Centers for Medicare & Medicaid Services (CMS) launched a new website – Road to ICD-10 – to provide a central source of basic information as well as a place to start transitioning to the new code set, which becomes mandatory on Oct. 1.
The site provides fact sheets, training videos, sample codes, and a variety of other resources. It also provides training modules that are specific to certain specialties.
Importantly, it gives physicians a template for building an action plan, said Denesecia Green, director of the Administrative Simplification Group at the CMS Office of eHealth Standards and Services.
So far, templates have been tailored for internal medicine, family practice, pediatrics, cardiology, obstetrics/gynecology, and orthopedics. The site also offers a more general path for other specialties.
According to Ms. Green, the action plan gives physicians a pictorial road map and lists the steps that might help pinpoint where diagnosis codes are used in the practice, how to identify the transition team, how to prepare a budget for the transition to ICD-10, and how to arrange for training.
The site was developed by physicians and came out of a series of listening sessions the agency held with a variety of physicians, said Dr. Ricardo Martinez, a member of the CMS’s small physician practice team, and an emergency physician.
"Physicians are concerned that everything is happening to them, rather than with them or for them," Dr. Martinez said.
However, many in the listening sessions said that they did see some potential benefits with ICD-10. In the end, Dr. Martinez said, physicians had a big question: "If there is a better world ahead, how do you get there?"
The Road to ICD-10 website is designed to help doctors make the journey, Dr. Martinez said.
The site was announced Feb. 26 at the annual meeting of the Healthcare Information and Management Systems Society (HIMSS).
On Twitter @aliciaault
AT HIMSS14
Stage 2 of meaningful use: Expect tougher objectives, pre-payment audits
ORLANDO – Expect a more rigorous process of certification for Stage 2 of meaningful use and be prepared for audits that will withhold incentive payments until all issues are resolved, federal officials advised.
This year is the first that physicians can work to meet the requirements for Stage 2 of meaningful use. Stage 1 was about data capture, but Stage 2 is about sharing information across care settings and between patients and providers, Robert Anthony, deputy director of the Health IT Initiatives Group at the Centers for Medicare and Medicaid Services’ Office of E-Health Standards and Services, said at the annual meeting of the Healthcare Information and Management Systems Society.
Among the core requirements for Stage 2 are establishing a patient portal and ensuring and using secure messaging between patients and providers. Physicians must be able to link to imaging results, report to a registry, and record electronic progress notes.
Mr. Anthony said that CMS purposely set what he called a "low bar" for patient engagement in Stage 2. To demonstrate meaningful use, 5% of patients must use the practice’s patient portal and 5% must participate in secure messaging beyond appointment booking, he said.
Even so, meeting that target might not be easy. Mr. Anthony said that he had heard from some physicians that they are sitting down with patients at the end of a visit and walking them through use of the portal or the messaging process. Those encounters, he added, can be counted toward the target.
Requirements for documenting care transitions are stricter as well, Mr. Anthony said.
"In Stage 1, ‘transitions of care’ was a menu objective, and virtually none of you selected transitions of care," he said. "We know why everybody didn’t select it – because it’s a difficult objective to achieve."
Care transitions, though, are "the Holy Grail" for showing that systems and clinicians can talk to each other, so the measure was moved into the core objectives for stage 2, he said.
Under Stage 1, physicians could send a summary of care to the next provider by any method, as long as it arrived, said Mr. Anthony. Under Stage 2, summaries must be electronically transmitted 10% or more of the time. At least some have to be sent to clinicians using a different electronic health record system.
Finally, CMS will be performing more audits under Stage 2. The agency must be accountable for the $21 billion spent on incentive payments so far, he said. In stage 1, the audits for Medicare were primarily post payment. Now, payments will be withheld until the audits are resolved. Some 5%-10% of physicians will be subject to an audit. They will be chosen at random or through risk profiling.
And, "no, we’re not going to talk about what raises a red flag, because that’s the point of an oversight program," he added.
So far, documentation has been the primary deficiency found through the audit process, Mr. Anthony said.
"I am shocked by the number of people who do not retain any documentation related to their attestation figures," he said. Physicians need to document the numerators and denominators they use for attestation and then keep that documentation for 6 years.
There are no consultants or companies that have any special knowledge about how to avoid audits or resolve an audit more quickly. They also don’t know anything special about the appeals process. "The process is the same for everybody and is transparent and public for everybody," he said.
"Anybody who is telling you separately that they have some kind of inside line to CMS is drumming up business and nothing more," Mr. Anthony said.
He also said that there is no secret process to getting an appeal. The agency spells out what it is looking for in the appeals documentation available on the CMS ICD-10 website. There’s also a sample audit letter from the CMS contractor, Figliozzi and Co.
On Twitter @aliciaault
ORLANDO – Expect a more rigorous process of certification for Stage 2 of meaningful use and be prepared for audits that will withhold incentive payments until all issues are resolved, federal officials advised.
This year is the first that physicians can work to meet the requirements for Stage 2 of meaningful use. Stage 1 was about data capture, but Stage 2 is about sharing information across care settings and between patients and providers, Robert Anthony, deputy director of the Health IT Initiatives Group at the Centers for Medicare and Medicaid Services’ Office of E-Health Standards and Services, said at the annual meeting of the Healthcare Information and Management Systems Society.
Among the core requirements for Stage 2 are establishing a patient portal and ensuring and using secure messaging between patients and providers. Physicians must be able to link to imaging results, report to a registry, and record electronic progress notes.
Mr. Anthony said that CMS purposely set what he called a "low bar" for patient engagement in Stage 2. To demonstrate meaningful use, 5% of patients must use the practice’s patient portal and 5% must participate in secure messaging beyond appointment booking, he said.
Even so, meeting that target might not be easy. Mr. Anthony said that he had heard from some physicians that they are sitting down with patients at the end of a visit and walking them through use of the portal or the messaging process. Those encounters, he added, can be counted toward the target.
Requirements for documenting care transitions are stricter as well, Mr. Anthony said.
"In Stage 1, ‘transitions of care’ was a menu objective, and virtually none of you selected transitions of care," he said. "We know why everybody didn’t select it – because it’s a difficult objective to achieve."
Care transitions, though, are "the Holy Grail" for showing that systems and clinicians can talk to each other, so the measure was moved into the core objectives for stage 2, he said.
Under Stage 1, physicians could send a summary of care to the next provider by any method, as long as it arrived, said Mr. Anthony. Under Stage 2, summaries must be electronically transmitted 10% or more of the time. At least some have to be sent to clinicians using a different electronic health record system.
Finally, CMS will be performing more audits under Stage 2. The agency must be accountable for the $21 billion spent on incentive payments so far, he said. In stage 1, the audits for Medicare were primarily post payment. Now, payments will be withheld until the audits are resolved. Some 5%-10% of physicians will be subject to an audit. They will be chosen at random or through risk profiling.
And, "no, we’re not going to talk about what raises a red flag, because that’s the point of an oversight program," he added.
So far, documentation has been the primary deficiency found through the audit process, Mr. Anthony said.
"I am shocked by the number of people who do not retain any documentation related to their attestation figures," he said. Physicians need to document the numerators and denominators they use for attestation and then keep that documentation for 6 years.
There are no consultants or companies that have any special knowledge about how to avoid audits or resolve an audit more quickly. They also don’t know anything special about the appeals process. "The process is the same for everybody and is transparent and public for everybody," he said.
"Anybody who is telling you separately that they have some kind of inside line to CMS is drumming up business and nothing more," Mr. Anthony said.
He also said that there is no secret process to getting an appeal. The agency spells out what it is looking for in the appeals documentation available on the CMS ICD-10 website. There’s also a sample audit letter from the CMS contractor, Figliozzi and Co.
On Twitter @aliciaault
ORLANDO – Expect a more rigorous process of certification for Stage 2 of meaningful use and be prepared for audits that will withhold incentive payments until all issues are resolved, federal officials advised.
This year is the first that physicians can work to meet the requirements for Stage 2 of meaningful use. Stage 1 was about data capture, but Stage 2 is about sharing information across care settings and between patients and providers, Robert Anthony, deputy director of the Health IT Initiatives Group at the Centers for Medicare and Medicaid Services’ Office of E-Health Standards and Services, said at the annual meeting of the Healthcare Information and Management Systems Society.
Among the core requirements for Stage 2 are establishing a patient portal and ensuring and using secure messaging between patients and providers. Physicians must be able to link to imaging results, report to a registry, and record electronic progress notes.
Mr. Anthony said that CMS purposely set what he called a "low bar" for patient engagement in Stage 2. To demonstrate meaningful use, 5% of patients must use the practice’s patient portal and 5% must participate in secure messaging beyond appointment booking, he said.
Even so, meeting that target might not be easy. Mr. Anthony said that he had heard from some physicians that they are sitting down with patients at the end of a visit and walking them through use of the portal or the messaging process. Those encounters, he added, can be counted toward the target.
Requirements for documenting care transitions are stricter as well, Mr. Anthony said.
"In Stage 1, ‘transitions of care’ was a menu objective, and virtually none of you selected transitions of care," he said. "We know why everybody didn’t select it – because it’s a difficult objective to achieve."
Care transitions, though, are "the Holy Grail" for showing that systems and clinicians can talk to each other, so the measure was moved into the core objectives for stage 2, he said.
Under Stage 1, physicians could send a summary of care to the next provider by any method, as long as it arrived, said Mr. Anthony. Under Stage 2, summaries must be electronically transmitted 10% or more of the time. At least some have to be sent to clinicians using a different electronic health record system.
Finally, CMS will be performing more audits under Stage 2. The agency must be accountable for the $21 billion spent on incentive payments so far, he said. In stage 1, the audits for Medicare were primarily post payment. Now, payments will be withheld until the audits are resolved. Some 5%-10% of physicians will be subject to an audit. They will be chosen at random or through risk profiling.
And, "no, we’re not going to talk about what raises a red flag, because that’s the point of an oversight program," he added.
So far, documentation has been the primary deficiency found through the audit process, Mr. Anthony said.
"I am shocked by the number of people who do not retain any documentation related to their attestation figures," he said. Physicians need to document the numerators and denominators they use for attestation and then keep that documentation for 6 years.
There are no consultants or companies that have any special knowledge about how to avoid audits or resolve an audit more quickly. They also don’t know anything special about the appeals process. "The process is the same for everybody and is transparent and public for everybody," he said.
"Anybody who is telling you separately that they have some kind of inside line to CMS is drumming up business and nothing more," Mr. Anthony said.
He also said that there is no secret process to getting an appeal. The agency spells out what it is looking for in the appeals documentation available on the CMS ICD-10 website. There’s also a sample audit letter from the CMS contractor, Figliozzi and Co.
On Twitter @aliciaault
AT HIMSS14
Doctors seek to delay 2014 meaningful use deadlines
ORLANDO – Several dozen physician organizations are imploring the Department of Health and Human Services to slow down implementation of the meaningful use program for electronic health records, saying that the pace is overwhelming doctors’ ability to keep up.
The request comes as more than 35,500 attendees gather for the annual meeting of the Healthcare Information and Management Systems Society to learn more about government and private efforts to digitize the U.S. health care system.
In a letter to HHS Secretary Kathleen Sebelius, the physician groups said that doctors are struggling to make the investments needed to meet the federal targets. The groups want the government to give physicians through 2015 to transition to new EHR software and to meet stage 1 and 2 meaningful use requirements. They are also seeking more flexibility in how physicians meet those requirements.
Under the meaningful use program, eligible providers – physicians, nurse practitioners, and physician assistants who meet specific criteria – can receive incentive payments from Medicare and Medicaid. In 2014, the Medicare payment can be up to $23,520.
Centers for Medicare & Medicaid Services (CMS) officials at the HIMSS meeting said that 267,029 eligible providers have received Medicare incentive payments and 142,801 have received Medicaid payments since the program began in 2011, amounting to some $21 billion in payouts.
Providers will be penalized in 2015 if they do not sign up to be a meaningful user by March 31, said Elizabeth Holland, director of the HIT initiatives group at the CMS Office of E-Health Standards and Services. That date was recently extended by a month. Doctors who have never participated in the meaningful use program have until Oct. 1 to sign up to avoid penalties next year, and many physicians may be eligible for hardship exemptions that give them even more time to sign up, Ms. Holland said.
The physician groups still want more leeway. A big sticking point: Currently, eligible professionals have to adopt the 2014 Edition of Certified Electronic Health Record Technology (CEHRT) and also meet more stringent meaningful use standards by the end of the year. Most providers are still working with the last edition – the 2011 CEHRT. The Office of the National Coordinator for Health Information Technology (ONC) created the CEHRT program to guide providers to EHRs that contain all the elements necessary to achieve meaningful use. The 2014 edition supports stage 2 of meaningful use, which started this year.
"With only a fraction of 2011 Edition products currently certified to 2014 Edition standards, it is clear the pace and scope of change have outstripped the ability of vendors to support providers," according to the letter from the physician groups. If doctors can’t easily move on to the 2014 edition, they might "either abandon the possibility of meeting meaningful use criteria in 2014 or be forced to implement a system much more rapidly than would otherwise be the case."
While physicians worry about the 2014 edition, the ONC on Feb. 21 proposed to move forward again, spelling out standards for the 2015 edition of the CEHRT.
The ONC said that compliance with the 2015 edition would be voluntary – providers would not have to upgrade to be able to get incentive payments.
"This provides the opportunity for developers and health care providers to move to the 2015 Edition on their own terms and at their own pace," Dr. Karen DeSalvo, national coordinator for health IT, said in a statement.
The rule on the 2015 edition will be published in the Federal Register on Feb. 26, and the ONC will take comments at www.regulations.gov until April 28. The final rule will be published this summer.
On Twitter @aliciaault
ORLANDO – Several dozen physician organizations are imploring the Department of Health and Human Services to slow down implementation of the meaningful use program for electronic health records, saying that the pace is overwhelming doctors’ ability to keep up.
The request comes as more than 35,500 attendees gather for the annual meeting of the Healthcare Information and Management Systems Society to learn more about government and private efforts to digitize the U.S. health care system.
In a letter to HHS Secretary Kathleen Sebelius, the physician groups said that doctors are struggling to make the investments needed to meet the federal targets. The groups want the government to give physicians through 2015 to transition to new EHR software and to meet stage 1 and 2 meaningful use requirements. They are also seeking more flexibility in how physicians meet those requirements.
Under the meaningful use program, eligible providers – physicians, nurse practitioners, and physician assistants who meet specific criteria – can receive incentive payments from Medicare and Medicaid. In 2014, the Medicare payment can be up to $23,520.
Centers for Medicare & Medicaid Services (CMS) officials at the HIMSS meeting said that 267,029 eligible providers have received Medicare incentive payments and 142,801 have received Medicaid payments since the program began in 2011, amounting to some $21 billion in payouts.
Providers will be penalized in 2015 if they do not sign up to be a meaningful user by March 31, said Elizabeth Holland, director of the HIT initiatives group at the CMS Office of E-Health Standards and Services. That date was recently extended by a month. Doctors who have never participated in the meaningful use program have until Oct. 1 to sign up to avoid penalties next year, and many physicians may be eligible for hardship exemptions that give them even more time to sign up, Ms. Holland said.
The physician groups still want more leeway. A big sticking point: Currently, eligible professionals have to adopt the 2014 Edition of Certified Electronic Health Record Technology (CEHRT) and also meet more stringent meaningful use standards by the end of the year. Most providers are still working with the last edition – the 2011 CEHRT. The Office of the National Coordinator for Health Information Technology (ONC) created the CEHRT program to guide providers to EHRs that contain all the elements necessary to achieve meaningful use. The 2014 edition supports stage 2 of meaningful use, which started this year.
"With only a fraction of 2011 Edition products currently certified to 2014 Edition standards, it is clear the pace and scope of change have outstripped the ability of vendors to support providers," according to the letter from the physician groups. If doctors can’t easily move on to the 2014 edition, they might "either abandon the possibility of meeting meaningful use criteria in 2014 or be forced to implement a system much more rapidly than would otherwise be the case."
While physicians worry about the 2014 edition, the ONC on Feb. 21 proposed to move forward again, spelling out standards for the 2015 edition of the CEHRT.
The ONC said that compliance with the 2015 edition would be voluntary – providers would not have to upgrade to be able to get incentive payments.
"This provides the opportunity for developers and health care providers to move to the 2015 Edition on their own terms and at their own pace," Dr. Karen DeSalvo, national coordinator for health IT, said in a statement.
The rule on the 2015 edition will be published in the Federal Register on Feb. 26, and the ONC will take comments at www.regulations.gov until April 28. The final rule will be published this summer.
On Twitter @aliciaault
ORLANDO – Several dozen physician organizations are imploring the Department of Health and Human Services to slow down implementation of the meaningful use program for electronic health records, saying that the pace is overwhelming doctors’ ability to keep up.
The request comes as more than 35,500 attendees gather for the annual meeting of the Healthcare Information and Management Systems Society to learn more about government and private efforts to digitize the U.S. health care system.
In a letter to HHS Secretary Kathleen Sebelius, the physician groups said that doctors are struggling to make the investments needed to meet the federal targets. The groups want the government to give physicians through 2015 to transition to new EHR software and to meet stage 1 and 2 meaningful use requirements. They are also seeking more flexibility in how physicians meet those requirements.
Under the meaningful use program, eligible providers – physicians, nurse practitioners, and physician assistants who meet specific criteria – can receive incentive payments from Medicare and Medicaid. In 2014, the Medicare payment can be up to $23,520.
Centers for Medicare & Medicaid Services (CMS) officials at the HIMSS meeting said that 267,029 eligible providers have received Medicare incentive payments and 142,801 have received Medicaid payments since the program began in 2011, amounting to some $21 billion in payouts.
Providers will be penalized in 2015 if they do not sign up to be a meaningful user by March 31, said Elizabeth Holland, director of the HIT initiatives group at the CMS Office of E-Health Standards and Services. That date was recently extended by a month. Doctors who have never participated in the meaningful use program have until Oct. 1 to sign up to avoid penalties next year, and many physicians may be eligible for hardship exemptions that give them even more time to sign up, Ms. Holland said.
The physician groups still want more leeway. A big sticking point: Currently, eligible professionals have to adopt the 2014 Edition of Certified Electronic Health Record Technology (CEHRT) and also meet more stringent meaningful use standards by the end of the year. Most providers are still working with the last edition – the 2011 CEHRT. The Office of the National Coordinator for Health Information Technology (ONC) created the CEHRT program to guide providers to EHRs that contain all the elements necessary to achieve meaningful use. The 2014 edition supports stage 2 of meaningful use, which started this year.
"With only a fraction of 2011 Edition products currently certified to 2014 Edition standards, it is clear the pace and scope of change have outstripped the ability of vendors to support providers," according to the letter from the physician groups. If doctors can’t easily move on to the 2014 edition, they might "either abandon the possibility of meeting meaningful use criteria in 2014 or be forced to implement a system much more rapidly than would otherwise be the case."
While physicians worry about the 2014 edition, the ONC on Feb. 21 proposed to move forward again, spelling out standards for the 2015 edition of the CEHRT.
The ONC said that compliance with the 2015 edition would be voluntary – providers would not have to upgrade to be able to get incentive payments.
"This provides the opportunity for developers and health care providers to move to the 2015 Edition on their own terms and at their own pace," Dr. Karen DeSalvo, national coordinator for health IT, said in a statement.
The rule on the 2015 edition will be published in the Federal Register on Feb. 26, and the ONC will take comments at www.regulations.gov until April 28. The final rule will be published this summer.
On Twitter @aliciaault
AT HIMSS14