User login
Alcohol, Street Drugs Account for One in Eight Toddler Poisonings
BOSTON – Alcohol and illicit drugs account for about one in eight accidental drug poisonings of infants and toddlers in the United States, according to prospective registry data from 31 U.S. toxicology centers.
A review of confirmed poisoning cases from these centers showed that cardiac drugs accounted for 16% of poisonings of children under 2 years of age, followed by psychotropic drugs (15%), and recreational drugs and alcohol (13%), reported Dr. Yaron Finkelstein, a pediatric emergency medicine physician at the University of Toronto.
"Infant and toddler poisonings pose a unique public health concern. They involve among the most helpless and vulnerable populations in our society, partly because of their inability to protect themselves from environmental hazards, or communicate the circumstances of their injury," Dr. Finkelstein said.
Emergency department visits by children aged 5 years and under for poisoning in the United States rose 30% from 2001 to 2008, suggesting that better prevention methods and better data on the extent of the problem are needed, he said at the annual meeting of the Pediatric Academic Societies.
However, the National Poison Data System (NPDS), run by the American Association of Poison Control Centers, relies largely on voluntary information, and reported poisonings are not verified.
"The NPDS system probably underestimates the true magnitude of the problems, since less than 20% of poisoned children who actually present to the emergency department have contacted the regional poison control center," he said.
To get a clearer picture of accidental poisonings in children under 2 years, Dr. Finkelstein and his colleagues reviewed data from the Toxicology Investigators Consortium (ToxIC) Case Registry of the American College of Medical Toxicology (ACMT), a prospective, nationwide toxicology database with 31 U.S. registry sites.
They identified a total of 6,810 poisoning cases from April 2010 through June 2011, 248 (3.6%) of which involved children under age 2 years. The cases were all confirmed by a certified medical toxicologist at bedside.
Of these children, 51% were boys, and 63% were symptomatic at the time of consultation. Slightly more than half of the consultations (54%) occurred when the child was being admitted to the hospital, 42% occurred in the emergency department, and 4% took place in an outpatient setting.
The top seven exposures according to the ToxIC registry were to cardiac drugs , psychotropic agents, street drugs/alcohol, analgesics (9%), cleaning products (6.5%), scorpion stings (4.5%), and toxic alkaloids (3.9%).
In contrast, NPDS data for the same categories implicate, in descending order from most to least frequent, analgesics, cleaning products, psychotropics, alkaloids, cardiac drugs, street drugs, and scorpion stings, Dr. Finkelstein said.
He noted that because the ToxIC registry is a sentinel system based primarily in academic tertiary care centers, it may not be representative of the experience in community or primary care practice settings, but the ToxIC and NPDS registry data complement each other to provide effective real-time surveillance of poisonings in the United States.
The finding that one in eight children presenting with poisoning had been exposed to alcohol or illicit drugs "highlights again the issues of unsafe environment, child neglect, or maltreatment. Additionally, malicious intent should be considered, especially in first-year-of-life exposures," he concluded.
The study was supported by the Toxicology Investigators Consortium. Dr. Finkelstein reported having no relevant financial disclosures.
BOSTON – Alcohol and illicit drugs account for about one in eight accidental drug poisonings of infants and toddlers in the United States, according to prospective registry data from 31 U.S. toxicology centers.
A review of confirmed poisoning cases from these centers showed that cardiac drugs accounted for 16% of poisonings of children under 2 years of age, followed by psychotropic drugs (15%), and recreational drugs and alcohol (13%), reported Dr. Yaron Finkelstein, a pediatric emergency medicine physician at the University of Toronto.
"Infant and toddler poisonings pose a unique public health concern. They involve among the most helpless and vulnerable populations in our society, partly because of their inability to protect themselves from environmental hazards, or communicate the circumstances of their injury," Dr. Finkelstein said.
Emergency department visits by children aged 5 years and under for poisoning in the United States rose 30% from 2001 to 2008, suggesting that better prevention methods and better data on the extent of the problem are needed, he said at the annual meeting of the Pediatric Academic Societies.
However, the National Poison Data System (NPDS), run by the American Association of Poison Control Centers, relies largely on voluntary information, and reported poisonings are not verified.
"The NPDS system probably underestimates the true magnitude of the problems, since less than 20% of poisoned children who actually present to the emergency department have contacted the regional poison control center," he said.
To get a clearer picture of accidental poisonings in children under 2 years, Dr. Finkelstein and his colleagues reviewed data from the Toxicology Investigators Consortium (ToxIC) Case Registry of the American College of Medical Toxicology (ACMT), a prospective, nationwide toxicology database with 31 U.S. registry sites.
They identified a total of 6,810 poisoning cases from April 2010 through June 2011, 248 (3.6%) of which involved children under age 2 years. The cases were all confirmed by a certified medical toxicologist at bedside.
Of these children, 51% were boys, and 63% were symptomatic at the time of consultation. Slightly more than half of the consultations (54%) occurred when the child was being admitted to the hospital, 42% occurred in the emergency department, and 4% took place in an outpatient setting.
The top seven exposures according to the ToxIC registry were to cardiac drugs , psychotropic agents, street drugs/alcohol, analgesics (9%), cleaning products (6.5%), scorpion stings (4.5%), and toxic alkaloids (3.9%).
In contrast, NPDS data for the same categories implicate, in descending order from most to least frequent, analgesics, cleaning products, psychotropics, alkaloids, cardiac drugs, street drugs, and scorpion stings, Dr. Finkelstein said.
He noted that because the ToxIC registry is a sentinel system based primarily in academic tertiary care centers, it may not be representative of the experience in community or primary care practice settings, but the ToxIC and NPDS registry data complement each other to provide effective real-time surveillance of poisonings in the United States.
The finding that one in eight children presenting with poisoning had been exposed to alcohol or illicit drugs "highlights again the issues of unsafe environment, child neglect, or maltreatment. Additionally, malicious intent should be considered, especially in first-year-of-life exposures," he concluded.
The study was supported by the Toxicology Investigators Consortium. Dr. Finkelstein reported having no relevant financial disclosures.
BOSTON – Alcohol and illicit drugs account for about one in eight accidental drug poisonings of infants and toddlers in the United States, according to prospective registry data from 31 U.S. toxicology centers.
A review of confirmed poisoning cases from these centers showed that cardiac drugs accounted for 16% of poisonings of children under 2 years of age, followed by psychotropic drugs (15%), and recreational drugs and alcohol (13%), reported Dr. Yaron Finkelstein, a pediatric emergency medicine physician at the University of Toronto.
"Infant and toddler poisonings pose a unique public health concern. They involve among the most helpless and vulnerable populations in our society, partly because of their inability to protect themselves from environmental hazards, or communicate the circumstances of their injury," Dr. Finkelstein said.
Emergency department visits by children aged 5 years and under for poisoning in the United States rose 30% from 2001 to 2008, suggesting that better prevention methods and better data on the extent of the problem are needed, he said at the annual meeting of the Pediatric Academic Societies.
However, the National Poison Data System (NPDS), run by the American Association of Poison Control Centers, relies largely on voluntary information, and reported poisonings are not verified.
"The NPDS system probably underestimates the true magnitude of the problems, since less than 20% of poisoned children who actually present to the emergency department have contacted the regional poison control center," he said.
To get a clearer picture of accidental poisonings in children under 2 years, Dr. Finkelstein and his colleagues reviewed data from the Toxicology Investigators Consortium (ToxIC) Case Registry of the American College of Medical Toxicology (ACMT), a prospective, nationwide toxicology database with 31 U.S. registry sites.
They identified a total of 6,810 poisoning cases from April 2010 through June 2011, 248 (3.6%) of which involved children under age 2 years. The cases were all confirmed by a certified medical toxicologist at bedside.
Of these children, 51% were boys, and 63% were symptomatic at the time of consultation. Slightly more than half of the consultations (54%) occurred when the child was being admitted to the hospital, 42% occurred in the emergency department, and 4% took place in an outpatient setting.
The top seven exposures according to the ToxIC registry were to cardiac drugs , psychotropic agents, street drugs/alcohol, analgesics (9%), cleaning products (6.5%), scorpion stings (4.5%), and toxic alkaloids (3.9%).
In contrast, NPDS data for the same categories implicate, in descending order from most to least frequent, analgesics, cleaning products, psychotropics, alkaloids, cardiac drugs, street drugs, and scorpion stings, Dr. Finkelstein said.
He noted that because the ToxIC registry is a sentinel system based primarily in academic tertiary care centers, it may not be representative of the experience in community or primary care practice settings, but the ToxIC and NPDS registry data complement each other to provide effective real-time surveillance of poisonings in the United States.
The finding that one in eight children presenting with poisoning had been exposed to alcohol or illicit drugs "highlights again the issues of unsafe environment, child neglect, or maltreatment. Additionally, malicious intent should be considered, especially in first-year-of-life exposures," he concluded.
The study was supported by the Toxicology Investigators Consortium. Dr. Finkelstein reported having no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: Cardiac drugs accounted for 16% of poisonings of children under 2 years of age in the United States, followed by psychotropic drugs (15%), and recreational drugs and alcohol (13%).
Data Source: Findings are based on a prospective registry of data from 31 U.S. toxicology centers.
Disclosures: The study was supported by the Toxicology Investigators Consortium. Dr. Finkelstein reported having no relevant financial disclosures.
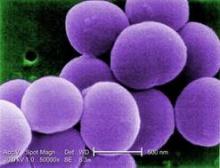
Chlorhexidine-Resistant S. aureus Infections on the Rise
BOSTON – It’s no surprise that antibiotic resistance continues to grow, but now some Staphylococcus aureus are showing off a new trick – resistance to chlorhexidine, the antiseptic relied upon to prevent staph infections.
In a review of isolates from pediatric cancer patients, an increasing number of S. aureus became resistant to the antiseptic, Dr. J. Chase McNeil said at the annual meeting of the Pediatric Academic Societies. The jump from susceptible to resistant occurred around 2006 – 2 years after the Texas Children’s Hospital began using chlorhexidine in the weekly central line dressing changes for its cancer patients, and a year after the facility introduced chlorhexidine mouthwash up to four times each day for patients with acute myeloid leukemia.
"It’s very interesting to see this upward trend [in resistance]," he said in an interview. "Before 2007, we had none, and since then we’ve seen an increase every year."
While the clinical significance of this phenomenon remains unclear, it’s very clear that the bacteria are changing, he added.
Dr. Chase reported a review of a prospectively acquired data set, which includes all children treated at the university’s pediatric oncology facility. He and his coinvestigators looked for infections caused by S. aureus and their related complications. They also assessed the emergence of staph isolates showing the qacA/B gene, which confers a higher minimum inhibitory concentration and minimum bactericidal concentration to chlorhexidine and other quaternary ammonium compound (QAC) antiseptics. The study also examined rates of methicillin resistance.
From 2001 through 2011, 213 S. aureus infections developed in 179 patients. Infections were most commonly associated with acute lymphoblastic leukemia (43%). Other cancers were primary central nervous system malignancies (11%), acute myeloid leukemia (AML), and hematopoietic stem cell transplant (HSCT) patients (16%). Among the infections were bacteremias (40%), skin and soft tissue infections (36%) and surgical site infections (15%).
Most of the infections were methicillin-susceptible S. aureus (147); the remaining infections were methicillin resistant. Most of the methicillin-resistant S. aureus isolates were also the USA300 strain, a particularly resistant strain associated with serious, rapidly progressing infections. The USA300 isolates were responsible for 59% of the skin/soft tissue infections and 25% of the bacteremias.
Overall, 8% of the isolates were also qacA/B positive. These were more likely to be resistant to ciprofloxacin than the qacA/B-negative isolates (50% vs. 15%).
Chlorhexidine-cleansed dressing changes and catheter cleansings began in 2004 in response to a sharp increase in staph infections in AML and HSCT patients, Dr. McNeil said. These infections did drop precipitously in the following years. In 2005, AML patients began using a chlorhexidine mouthwash up to four times each day.
However, in 2006, just as the staph infection rate was improving, qacA/B resistance suddenly appeared. By 2009, 10% of infections were positive for qacA/B, and by 2011, this had risen to about 22%.
"We can’t say if the change in the microbiology of these is caused by anything, or causing anything significant, but there is definitely a temporal association," he said.
Chlorhexidine continues to be relied upon in the oncology ward, he said. By 2011, daily chlorhexidine baths became part of the standard care for neutropenic AML patients.
Among the entire group of patients with infections, 19% (37) developed a total of 58 complications. Bacteremias were associated with most of the complications (70%). A multivariate analysis showed a significant association between complicated bacteremias and AMC patients with a low lymphocyte count.
Thirteen patients with bacteremia also developed pulmonary nodules. All of these were associated with methicillin-susceptible S. aureus isolates. The nodules developed rapidly, appearing a median of 5 days after bacteremia onset. Six patients were biopsied, with S. aureus cultured from five. One nodule was a metastatic tumor. One other patient with nodules died before culture. This patient had an invasive pulmonary fungal infection.
Dr. McNeil said several factors were significantly associated with staph infections and pulmonary nodules, including HSCT, a low lymphocyte count, and low platelets.
"This isn’t surprising because it’s well known that children with malignancies are at a high risk for staph disease because of their immune compromise and a high exposure to empiric antibiotics and antiseptics."
Dr. McNeil said he had no financial declarations.
BOSTON – It’s no surprise that antibiotic resistance continues to grow, but now some Staphylococcus aureus are showing off a new trick – resistance to chlorhexidine, the antiseptic relied upon to prevent staph infections.
In a review of isolates from pediatric cancer patients, an increasing number of S. aureus became resistant to the antiseptic, Dr. J. Chase McNeil said at the annual meeting of the Pediatric Academic Societies. The jump from susceptible to resistant occurred around 2006 – 2 years after the Texas Children’s Hospital began using chlorhexidine in the weekly central line dressing changes for its cancer patients, and a year after the facility introduced chlorhexidine mouthwash up to four times each day for patients with acute myeloid leukemia.
"It’s very interesting to see this upward trend [in resistance]," he said in an interview. "Before 2007, we had none, and since then we’ve seen an increase every year."
While the clinical significance of this phenomenon remains unclear, it’s very clear that the bacteria are changing, he added.
Dr. Chase reported a review of a prospectively acquired data set, which includes all children treated at the university’s pediatric oncology facility. He and his coinvestigators looked for infections caused by S. aureus and their related complications. They also assessed the emergence of staph isolates showing the qacA/B gene, which confers a higher minimum inhibitory concentration and minimum bactericidal concentration to chlorhexidine and other quaternary ammonium compound (QAC) antiseptics. The study also examined rates of methicillin resistance.
From 2001 through 2011, 213 S. aureus infections developed in 179 patients. Infections were most commonly associated with acute lymphoblastic leukemia (43%). Other cancers were primary central nervous system malignancies (11%), acute myeloid leukemia (AML), and hematopoietic stem cell transplant (HSCT) patients (16%). Among the infections were bacteremias (40%), skin and soft tissue infections (36%) and surgical site infections (15%).
Most of the infections were methicillin-susceptible S. aureus (147); the remaining infections were methicillin resistant. Most of the methicillin-resistant S. aureus isolates were also the USA300 strain, a particularly resistant strain associated with serious, rapidly progressing infections. The USA300 isolates were responsible for 59% of the skin/soft tissue infections and 25% of the bacteremias.
Overall, 8% of the isolates were also qacA/B positive. These were more likely to be resistant to ciprofloxacin than the qacA/B-negative isolates (50% vs. 15%).
Chlorhexidine-cleansed dressing changes and catheter cleansings began in 2004 in response to a sharp increase in staph infections in AML and HSCT patients, Dr. McNeil said. These infections did drop precipitously in the following years. In 2005, AML patients began using a chlorhexidine mouthwash up to four times each day.
However, in 2006, just as the staph infection rate was improving, qacA/B resistance suddenly appeared. By 2009, 10% of infections were positive for qacA/B, and by 2011, this had risen to about 22%.
"We can’t say if the change in the microbiology of these is caused by anything, or causing anything significant, but there is definitely a temporal association," he said.
Chlorhexidine continues to be relied upon in the oncology ward, he said. By 2011, daily chlorhexidine baths became part of the standard care for neutropenic AML patients.
Among the entire group of patients with infections, 19% (37) developed a total of 58 complications. Bacteremias were associated with most of the complications (70%). A multivariate analysis showed a significant association between complicated bacteremias and AMC patients with a low lymphocyte count.
Thirteen patients with bacteremia also developed pulmonary nodules. All of these were associated with methicillin-susceptible S. aureus isolates. The nodules developed rapidly, appearing a median of 5 days after bacteremia onset. Six patients were biopsied, with S. aureus cultured from five. One nodule was a metastatic tumor. One other patient with nodules died before culture. This patient had an invasive pulmonary fungal infection.
Dr. McNeil said several factors were significantly associated with staph infections and pulmonary nodules, including HSCT, a low lymphocyte count, and low platelets.
"This isn’t surprising because it’s well known that children with malignancies are at a high risk for staph disease because of their immune compromise and a high exposure to empiric antibiotics and antiseptics."
Dr. McNeil said he had no financial declarations.
BOSTON – It’s no surprise that antibiotic resistance continues to grow, but now some Staphylococcus aureus are showing off a new trick – resistance to chlorhexidine, the antiseptic relied upon to prevent staph infections.
In a review of isolates from pediatric cancer patients, an increasing number of S. aureus became resistant to the antiseptic, Dr. J. Chase McNeil said at the annual meeting of the Pediatric Academic Societies. The jump from susceptible to resistant occurred around 2006 – 2 years after the Texas Children’s Hospital began using chlorhexidine in the weekly central line dressing changes for its cancer patients, and a year after the facility introduced chlorhexidine mouthwash up to four times each day for patients with acute myeloid leukemia.
"It’s very interesting to see this upward trend [in resistance]," he said in an interview. "Before 2007, we had none, and since then we’ve seen an increase every year."
While the clinical significance of this phenomenon remains unclear, it’s very clear that the bacteria are changing, he added.
Dr. Chase reported a review of a prospectively acquired data set, which includes all children treated at the university’s pediatric oncology facility. He and his coinvestigators looked for infections caused by S. aureus and their related complications. They also assessed the emergence of staph isolates showing the qacA/B gene, which confers a higher minimum inhibitory concentration and minimum bactericidal concentration to chlorhexidine and other quaternary ammonium compound (QAC) antiseptics. The study also examined rates of methicillin resistance.
From 2001 through 2011, 213 S. aureus infections developed in 179 patients. Infections were most commonly associated with acute lymphoblastic leukemia (43%). Other cancers were primary central nervous system malignancies (11%), acute myeloid leukemia (AML), and hematopoietic stem cell transplant (HSCT) patients (16%). Among the infections were bacteremias (40%), skin and soft tissue infections (36%) and surgical site infections (15%).
Most of the infections were methicillin-susceptible S. aureus (147); the remaining infections were methicillin resistant. Most of the methicillin-resistant S. aureus isolates were also the USA300 strain, a particularly resistant strain associated with serious, rapidly progressing infections. The USA300 isolates were responsible for 59% of the skin/soft tissue infections and 25% of the bacteremias.
Overall, 8% of the isolates were also qacA/B positive. These were more likely to be resistant to ciprofloxacin than the qacA/B-negative isolates (50% vs. 15%).
Chlorhexidine-cleansed dressing changes and catheter cleansings began in 2004 in response to a sharp increase in staph infections in AML and HSCT patients, Dr. McNeil said. These infections did drop precipitously in the following years. In 2005, AML patients began using a chlorhexidine mouthwash up to four times each day.
However, in 2006, just as the staph infection rate was improving, qacA/B resistance suddenly appeared. By 2009, 10% of infections were positive for qacA/B, and by 2011, this had risen to about 22%.
"We can’t say if the change in the microbiology of these is caused by anything, or causing anything significant, but there is definitely a temporal association," he said.
Chlorhexidine continues to be relied upon in the oncology ward, he said. By 2011, daily chlorhexidine baths became part of the standard care for neutropenic AML patients.
Among the entire group of patients with infections, 19% (37) developed a total of 58 complications. Bacteremias were associated with most of the complications (70%). A multivariate analysis showed a significant association between complicated bacteremias and AMC patients with a low lymphocyte count.
Thirteen patients with bacteremia also developed pulmonary nodules. All of these were associated with methicillin-susceptible S. aureus isolates. The nodules developed rapidly, appearing a median of 5 days after bacteremia onset. Six patients were biopsied, with S. aureus cultured from five. One nodule was a metastatic tumor. One other patient with nodules died before culture. This patient had an invasive pulmonary fungal infection.
Dr. McNeil said several factors were significantly associated with staph infections and pulmonary nodules, including HSCT, a low lymphocyte count, and low platelets.
"This isn’t surprising because it’s well known that children with malignancies are at a high risk for staph disease because of their immune compromise and a high exposure to empiric antibiotics and antiseptics."
Dr. McNeil said he had no financial declarations.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: In a pediatric oncology ward, chlorhexidine-resistant S. aureus–associated infections increased from 0 in 2007 to more than 20% of staph infections in 2011.
Data Source: The data were drawn from an 11-year prospectively acquired series.
Disclosures: Dr. J. Chase McNeil had no financial disclosures.
Neonatal Candidiasis Decreases With Prophylactic Antifungals
BOSTON – Preventive antifungal therapy and changes in broad-spectrum antibiotic use were associated with a significant decrease in the incidence of invasive candidiasis in neonatal intensive care units.
As these changes took place in a large group of neonatal intensive care units, Candida infections dropped from 4 to 1 per 1,000 patients. In the smallest infants – those weighing less than 750 grams – incidence dropped from 83 to 24 per 1,000, Dr. Sofia Aliaga said at the annual meeting of the Pediatric Academic Societies.
Dr. Aliaga, a neonatologist at the University of North Carolina at Chapel Hill, and her colleagues used a large administrative database to determine the incidence of invasive candidiasis over a 14-year period (1997-2010). In addition to disease incidence, they looked at changes in both antifungal prophylaxis and empirical treatment, and the use of broad-spectrum antibiotics in the NICUs.
The database contained information on 709,325 infants seen at 322 units, all of which were managed by a single medical group. There were 2,101 episodes of invasive candidiasis in 2,063 infants.
The researchers divided the cohort into four groups by weight: less than 750 g, 750-999 g, 1,000-1,499 g, and 1,500 g or heavier.
Over the study period, antifungal prophylaxis increased significantly among the smallest babies, from 4 to 119 admissions per 1,000. At the same time, empirical antifungal therapy for these infants also increased, from 4 to 11 admissions per 1,000 overall. The biggest change with empirical therapy occurred in the smallest babies, increasing from 4 to 111 per 1,000.
Finally, the units decreased their use of broad-spectrum antibiotics for all admissions. Use fell from 276 to 48 admissions per 1,000. This change was seen across all weight groups.
The incidence of invasive candidiasis fell from 4 to 1 per 1,000 admissions. The greatest decrease occurred among babies weighing less than 750 g. In this group, the infection fell from 83 to 24 per 1,000.
Overall changes in NICU management also might have influenced the incidence of candidiasis, Dr. Aliaga acknowledged.
"During this time, there was a big push to do quality improvement projects with central line catheters to decrease infection rates ... Babies in the NICU also spend a lot less time on ventilators now than they did 10 years ago, so with less time with an endotracheal tube there are fewer ventilator-associated infections. But I do think the decrease in disease we’re seeing is real, and related to the changes we have made."
Dr. Aliaga said she had no relevant financial disclosures.
BOSTON – Preventive antifungal therapy and changes in broad-spectrum antibiotic use were associated with a significant decrease in the incidence of invasive candidiasis in neonatal intensive care units.
As these changes took place in a large group of neonatal intensive care units, Candida infections dropped from 4 to 1 per 1,000 patients. In the smallest infants – those weighing less than 750 grams – incidence dropped from 83 to 24 per 1,000, Dr. Sofia Aliaga said at the annual meeting of the Pediatric Academic Societies.
Dr. Aliaga, a neonatologist at the University of North Carolina at Chapel Hill, and her colleagues used a large administrative database to determine the incidence of invasive candidiasis over a 14-year period (1997-2010). In addition to disease incidence, they looked at changes in both antifungal prophylaxis and empirical treatment, and the use of broad-spectrum antibiotics in the NICUs.
The database contained information on 709,325 infants seen at 322 units, all of which were managed by a single medical group. There were 2,101 episodes of invasive candidiasis in 2,063 infants.
The researchers divided the cohort into four groups by weight: less than 750 g, 750-999 g, 1,000-1,499 g, and 1,500 g or heavier.
Over the study period, antifungal prophylaxis increased significantly among the smallest babies, from 4 to 119 admissions per 1,000. At the same time, empirical antifungal therapy for these infants also increased, from 4 to 11 admissions per 1,000 overall. The biggest change with empirical therapy occurred in the smallest babies, increasing from 4 to 111 per 1,000.
Finally, the units decreased their use of broad-spectrum antibiotics for all admissions. Use fell from 276 to 48 admissions per 1,000. This change was seen across all weight groups.
The incidence of invasive candidiasis fell from 4 to 1 per 1,000 admissions. The greatest decrease occurred among babies weighing less than 750 g. In this group, the infection fell from 83 to 24 per 1,000.
Overall changes in NICU management also might have influenced the incidence of candidiasis, Dr. Aliaga acknowledged.
"During this time, there was a big push to do quality improvement projects with central line catheters to decrease infection rates ... Babies in the NICU also spend a lot less time on ventilators now than they did 10 years ago, so with less time with an endotracheal tube there are fewer ventilator-associated infections. But I do think the decrease in disease we’re seeing is real, and related to the changes we have made."
Dr. Aliaga said she had no relevant financial disclosures.
BOSTON – Preventive antifungal therapy and changes in broad-spectrum antibiotic use were associated with a significant decrease in the incidence of invasive candidiasis in neonatal intensive care units.
As these changes took place in a large group of neonatal intensive care units, Candida infections dropped from 4 to 1 per 1,000 patients. In the smallest infants – those weighing less than 750 grams – incidence dropped from 83 to 24 per 1,000, Dr. Sofia Aliaga said at the annual meeting of the Pediatric Academic Societies.
Dr. Aliaga, a neonatologist at the University of North Carolina at Chapel Hill, and her colleagues used a large administrative database to determine the incidence of invasive candidiasis over a 14-year period (1997-2010). In addition to disease incidence, they looked at changes in both antifungal prophylaxis and empirical treatment, and the use of broad-spectrum antibiotics in the NICUs.
The database contained information on 709,325 infants seen at 322 units, all of which were managed by a single medical group. There were 2,101 episodes of invasive candidiasis in 2,063 infants.
The researchers divided the cohort into four groups by weight: less than 750 g, 750-999 g, 1,000-1,499 g, and 1,500 g or heavier.
Over the study period, antifungal prophylaxis increased significantly among the smallest babies, from 4 to 119 admissions per 1,000. At the same time, empirical antifungal therapy for these infants also increased, from 4 to 11 admissions per 1,000 overall. The biggest change with empirical therapy occurred in the smallest babies, increasing from 4 to 111 per 1,000.
Finally, the units decreased their use of broad-spectrum antibiotics for all admissions. Use fell from 276 to 48 admissions per 1,000. This change was seen across all weight groups.
The incidence of invasive candidiasis fell from 4 to 1 per 1,000 admissions. The greatest decrease occurred among babies weighing less than 750 g. In this group, the infection fell from 83 to 24 per 1,000.
Overall changes in NICU management also might have influenced the incidence of candidiasis, Dr. Aliaga acknowledged.
"During this time, there was a big push to do quality improvement projects with central line catheters to decrease infection rates ... Babies in the NICU also spend a lot less time on ventilators now than they did 10 years ago, so with less time with an endotracheal tube there are fewer ventilator-associated infections. But I do think the decrease in disease we’re seeing is real, and related to the changes we have made."
Dr. Aliaga said she had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: The incidence of invasive candidiasis dropped by 75% after neonatal units instituted a program of prophylactic antifungal treatment.
Data Source: Dr. Aliaga extracted her data from a large administrative database.
Disclosures: Dr. Aliaga said she had no relevant financial disclosures.
Neonatal Early-Onset Sepsis: Revised Evaluation Guidelines Save Money
BOSTON – Implementation of a revised algorithm for the identification of early-onset sepsis in newborn infants significantly improves resource allocation and decreases overall health care costs, a study has shown.
To gauge the efficiency of the updated algorithm, which is based on the 2010 Centers for Disease Control and Prevention guidelines for the prevention of perinatal group B streptococcal (GBS) disease, Dr. Sagori Mukhopadhyay of Children’s Hospital, Boston, and colleagues conducted a retrospective time-series analysis to compare the frequency of early-onset sepsis (EOS) evaluations during two 5-month time periods – one in 2009, when the 2002 iteration of the guidelines were followed, and one in 2011, when the 2010 guidelines were followed – measuring differences in resource utilization and costs.
"We performed a retrospective economic evaluation to determine the cost difference between periods, using individual patient data, a third-party payer perspective, and a cost-minimization approach," she reported at the annual meeting of the Pediatric Academic Societies.
"We determined the costs associated with the early-onset sepsis evaluation, including laboratory, medication, and physician fees, and time spent in evaluation, specifically nursing costs," Dr. Mukhopadhyay said.
During the periods of study, 6,504 infants were born at or beyond 36 weeks’ gestation, including 662 who were evaluated for EOS. The overall incidence of EOS was 0.62/1,000 infants.
Importantly, "the frequency of evaluation for inadequate intrapartum antibiotic prophylaxis decreased significantly from 33/1,000 in 2009 to 3/1,000 in 2011," she said, with the remaining evaluations during both time periods conducted primarily because of maternal intrapartum fever. The reduction in evaluations for inadequate intrapartum prophylaxis translated into a significant reduction in overall costs associated with EOS evaluation, from $27,883.06 in 2009 to $2,434.64 in 2011. The findings may help hospitals transition to the revised recommendations in terms of anticipated staffing needs and resource allocation, she said.
Although the incidence of perinatal early-onset GBS has decreased since the CDC issued the first iteration of its prevention guidelines in 1996, GBS remained the leading cause of early-onset neonatal sepsis in 2010, prompting the revision of the 2002 guidelines.
Under the revised algorithm, all newborns with signs of sepsis should undergo a full diagnostic evaluation, including a blood culture, a complete blood count with white blood cell differential and platelet count, a chest radiograph in the presence of any abnormal respiratory signs, and a lumbar puncture if the newborn is stable enough to tolerate the procedure and sepsis is suspected. Further, the algorithm provides for the administration of antibiotics active against GBS, including intravenous ampicillin, and other organisms that could cause sepsis, such as Escherichia coli, pending the results of the evaluation.
Additional components of the algorithm include:
• A limited evaluation (consisting of blood culture and CBC) and antibiotic treatment – pending culture results – in well-appearing newborns whose mothers had suspected chorioamnionitis.
• Routine clinical care for well-appearing infants whose mothers had no chorioamnionitis and no indication for GBS prophylaxis.
• A minimum 48 hours of observation but no routine diagnostic testing in well-appearing infants of any gestational age whose mother received adequate intrapartum GBS prophylaxis consisting of at least 4 hours of intravenous penicillin, ampicillin, or cefazolin prior to delivery.
• Observation in well-appearing infants at least 37 weeks’ gestational age whose mothers had an indication for GBS prophylaxis but who received inadequate or no prophylaxis and in whom the duration of membrane rupture prior to delivery was less than 18 hours.
• Limited evaluation as above and a minimum of 48 hours of observation in well-appearing infants less than 37 weeks’ gestation born to mothers with an indication for prophylaxis who received inadequate or no prophylaxis and in whom the duration of membrane rupture prior to delivery was more than 18 hours.
Dr. Mukhopadhyay reported having no relevant financial disclosures.
BOSTON – Implementation of a revised algorithm for the identification of early-onset sepsis in newborn infants significantly improves resource allocation and decreases overall health care costs, a study has shown.
To gauge the efficiency of the updated algorithm, which is based on the 2010 Centers for Disease Control and Prevention guidelines for the prevention of perinatal group B streptococcal (GBS) disease, Dr. Sagori Mukhopadhyay of Children’s Hospital, Boston, and colleagues conducted a retrospective time-series analysis to compare the frequency of early-onset sepsis (EOS) evaluations during two 5-month time periods – one in 2009, when the 2002 iteration of the guidelines were followed, and one in 2011, when the 2010 guidelines were followed – measuring differences in resource utilization and costs.
"We performed a retrospective economic evaluation to determine the cost difference between periods, using individual patient data, a third-party payer perspective, and a cost-minimization approach," she reported at the annual meeting of the Pediatric Academic Societies.
"We determined the costs associated with the early-onset sepsis evaluation, including laboratory, medication, and physician fees, and time spent in evaluation, specifically nursing costs," Dr. Mukhopadhyay said.
During the periods of study, 6,504 infants were born at or beyond 36 weeks’ gestation, including 662 who were evaluated for EOS. The overall incidence of EOS was 0.62/1,000 infants.
Importantly, "the frequency of evaluation for inadequate intrapartum antibiotic prophylaxis decreased significantly from 33/1,000 in 2009 to 3/1,000 in 2011," she said, with the remaining evaluations during both time periods conducted primarily because of maternal intrapartum fever. The reduction in evaluations for inadequate intrapartum prophylaxis translated into a significant reduction in overall costs associated with EOS evaluation, from $27,883.06 in 2009 to $2,434.64 in 2011. The findings may help hospitals transition to the revised recommendations in terms of anticipated staffing needs and resource allocation, she said.
Although the incidence of perinatal early-onset GBS has decreased since the CDC issued the first iteration of its prevention guidelines in 1996, GBS remained the leading cause of early-onset neonatal sepsis in 2010, prompting the revision of the 2002 guidelines.
Under the revised algorithm, all newborns with signs of sepsis should undergo a full diagnostic evaluation, including a blood culture, a complete blood count with white blood cell differential and platelet count, a chest radiograph in the presence of any abnormal respiratory signs, and a lumbar puncture if the newborn is stable enough to tolerate the procedure and sepsis is suspected. Further, the algorithm provides for the administration of antibiotics active against GBS, including intravenous ampicillin, and other organisms that could cause sepsis, such as Escherichia coli, pending the results of the evaluation.
Additional components of the algorithm include:
• A limited evaluation (consisting of blood culture and CBC) and antibiotic treatment – pending culture results – in well-appearing newborns whose mothers had suspected chorioamnionitis.
• Routine clinical care for well-appearing infants whose mothers had no chorioamnionitis and no indication for GBS prophylaxis.
• A minimum 48 hours of observation but no routine diagnostic testing in well-appearing infants of any gestational age whose mother received adequate intrapartum GBS prophylaxis consisting of at least 4 hours of intravenous penicillin, ampicillin, or cefazolin prior to delivery.
• Observation in well-appearing infants at least 37 weeks’ gestational age whose mothers had an indication for GBS prophylaxis but who received inadequate or no prophylaxis and in whom the duration of membrane rupture prior to delivery was less than 18 hours.
• Limited evaluation as above and a minimum of 48 hours of observation in well-appearing infants less than 37 weeks’ gestation born to mothers with an indication for prophylaxis who received inadequate or no prophylaxis and in whom the duration of membrane rupture prior to delivery was more than 18 hours.
Dr. Mukhopadhyay reported having no relevant financial disclosures.
BOSTON – Implementation of a revised algorithm for the identification of early-onset sepsis in newborn infants significantly improves resource allocation and decreases overall health care costs, a study has shown.
To gauge the efficiency of the updated algorithm, which is based on the 2010 Centers for Disease Control and Prevention guidelines for the prevention of perinatal group B streptococcal (GBS) disease, Dr. Sagori Mukhopadhyay of Children’s Hospital, Boston, and colleagues conducted a retrospective time-series analysis to compare the frequency of early-onset sepsis (EOS) evaluations during two 5-month time periods – one in 2009, when the 2002 iteration of the guidelines were followed, and one in 2011, when the 2010 guidelines were followed – measuring differences in resource utilization and costs.
"We performed a retrospective economic evaluation to determine the cost difference between periods, using individual patient data, a third-party payer perspective, and a cost-minimization approach," she reported at the annual meeting of the Pediatric Academic Societies.
"We determined the costs associated with the early-onset sepsis evaluation, including laboratory, medication, and physician fees, and time spent in evaluation, specifically nursing costs," Dr. Mukhopadhyay said.
During the periods of study, 6,504 infants were born at or beyond 36 weeks’ gestation, including 662 who were evaluated for EOS. The overall incidence of EOS was 0.62/1,000 infants.
Importantly, "the frequency of evaluation for inadequate intrapartum antibiotic prophylaxis decreased significantly from 33/1,000 in 2009 to 3/1,000 in 2011," she said, with the remaining evaluations during both time periods conducted primarily because of maternal intrapartum fever. The reduction in evaluations for inadequate intrapartum prophylaxis translated into a significant reduction in overall costs associated with EOS evaluation, from $27,883.06 in 2009 to $2,434.64 in 2011. The findings may help hospitals transition to the revised recommendations in terms of anticipated staffing needs and resource allocation, she said.
Although the incidence of perinatal early-onset GBS has decreased since the CDC issued the first iteration of its prevention guidelines in 1996, GBS remained the leading cause of early-onset neonatal sepsis in 2010, prompting the revision of the 2002 guidelines.
Under the revised algorithm, all newborns with signs of sepsis should undergo a full diagnostic evaluation, including a blood culture, a complete blood count with white blood cell differential and platelet count, a chest radiograph in the presence of any abnormal respiratory signs, and a lumbar puncture if the newborn is stable enough to tolerate the procedure and sepsis is suspected. Further, the algorithm provides for the administration of antibiotics active against GBS, including intravenous ampicillin, and other organisms that could cause sepsis, such as Escherichia coli, pending the results of the evaluation.
Additional components of the algorithm include:
• A limited evaluation (consisting of blood culture and CBC) and antibiotic treatment – pending culture results – in well-appearing newborns whose mothers had suspected chorioamnionitis.
• Routine clinical care for well-appearing infants whose mothers had no chorioamnionitis and no indication for GBS prophylaxis.
• A minimum 48 hours of observation but no routine diagnostic testing in well-appearing infants of any gestational age whose mother received adequate intrapartum GBS prophylaxis consisting of at least 4 hours of intravenous penicillin, ampicillin, or cefazolin prior to delivery.
• Observation in well-appearing infants at least 37 weeks’ gestational age whose mothers had an indication for GBS prophylaxis but who received inadequate or no prophylaxis and in whom the duration of membrane rupture prior to delivery was less than 18 hours.
• Limited evaluation as above and a minimum of 48 hours of observation in well-appearing infants less than 37 weeks’ gestation born to mothers with an indication for prophylaxis who received inadequate or no prophylaxis and in whom the duration of membrane rupture prior to delivery was more than 18 hours.
Dr. Mukhopadhyay reported having no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: The frequency of newborn evaluation for inadequate intrapartum antibiotic prophylaxis at an academic medical center decreased significantly from 33/1,000 births during a 5-month period in 2009 under 2002 CDC guidelines to 3/1,000 during a 5-month period in 2011 under revised 2010 CDC guidelines. The overall costs associated with early-onset sepsis evaluations decreased from $27,883.06 in 2009 to $2,434.64 in 2011.
Data Source: A retrospective economic analysis of two 5-month periods to measure differences in resource utilization and costs associated with the transition to the 2010 guidelines.
Disclosures: Dr. Mukhopadhyay reported having no relevant financial disclosures.
Abused Children Treated in ED at Risk of Return
BOSTON – Children treated in the emergency department for abuse or neglect are at increased risk for further maltreatment, even after medical or social service intervention, a study has shown.
Among nearly 44,000 pediatric emergency department (ED) visits with at least one ICD-9 code for maltreatment, 3% of the children returned one or more times and were again identified as victims of maltreatment, reported Michael C. Monuteaux, Sc.D., of Harvard Medical School, Boston.
Children who were admitted to a patient floor or to an intensive care unit on their initial visit were twice as likely as those who were treated and released to be readmitted on subsequent ED visits. Children under 5 years of age were the most vulnerable, the authors found.
"Even when maltreatment is identified in the ED, children are at risk for further victimization resulting in future ED care," Dr. Monuteaux said at the annual meeting of the Pediatric Academic Societies.
Coinvestigator Dr. Daniel M. Lindberg, an emergency physician at Brigham and Women’s Hospital in Boston, said in an interview that the Child Protective Services workers have "a tremendously difficult" job made even more difficult by increasing caseloads and proposed reductions in funding.
"If that happens, [there will be] fewer investigators or case workers who can do the kind of checking in to make sure that safety plans are being followed or dangerous people are kept away from kids at risk. My hope is that any intervention to support Child Protective Services workers, and decrease caseloads, will help decrease rates of recurrent abuse," he said.
Dr. Monuteaux and Dr. Lindberg took a retrospective look at data from an administrative database on children under 18 treated in the emergency departments of 41 U.S. hospitals in 2005-2010.
They identified 43,824 ED visits by 42,354 children with one or more ICD-9 principal or secondary diagnoses of physical or sexual abuse, or other/unspecified maltreatment, and used medical record numbers to track patients over time.
In all, 1,286 maltreated children (3.0%) returned for another ED visit and received a second diagnosis of maltreatment. The median age of the children was 3 years (range, 1-8 years), 63% were girls, and 60% were white. The majority of the children (90%) had two ED visits, 8% had three visits, and 2% were seen in the ED four or more times.
One-fourth of the returning patients were seen again in the emergency department within 21 days, half within 150 days, and two-thirds within 1 year.
Abuse and neglect was the primary diagnosis in 38%, sexual abuse in 18%, physical abuse in 17%, and other maltreatment or injury in 27%.
Overall, 20% were admitted to the hospital at the initial visit, 3% were admitted to an ICU, and 6% underwent surgery for their injuries.
Of 253 children admitted at the initial visit, 42% were also admitted on their second visit. In comparison, of the 1,033 children not admitted at their first ED visit, 7% were admitted on the second visit. The odds ratio (OR) for being admitted a second time after a first admission was 2.1 (95% confidence interval [CI], 1.6-2.8).
Similarly, of 78 children with an initial ICU stay, 17% went back to the ICU at the second ED visit, compared with 2% of those who were not put in intensive care at their first ED visit (OR, 2.2; 95% CI, 1.4-3.6).
In a multivariate analysis controlled for demographic and clinical factors, the only significant predictor of repeat ED visits was age younger than 5 years (OR, 1.47; 95% CI, 1.22-1.78).
Dr. Monuteaux noted that the study might underestimate the actual number of repeat abuse cases because of its reliance on ICD-9 codes and because some of the children may have had ED visits for abuse or neglect before the start of the study. It is also possible that the code for physical abuse reflects long-term complications from prior abuse and not a new episode. Additionally, the data were drawn from academic pediatric hospitals and may not reflect the experience of community and general hospitals.
"Despite the dedicated work of ED and child protection workers, children diagnosed with maltreatment in the ED are at risk for additional victimization and subsequent emergency care for maltreatment, which leads us to suggest that improvements in the child protection apparatus should be considered," Dr. Monuteaux concluded.
The study was internally funded. The authors reported having no relevant financial relationships.
Michael C. Monuteaux, Sc.D., intensive care unit, Children under 5 years of age, maltreatment identified in the ED, Pediatric Academic Societies, Dr. Daniel M. Lindberg, Child Protective Services,
BOSTON – Children treated in the emergency department for abuse or neglect are at increased risk for further maltreatment, even after medical or social service intervention, a study has shown.
Among nearly 44,000 pediatric emergency department (ED) visits with at least one ICD-9 code for maltreatment, 3% of the children returned one or more times and were again identified as victims of maltreatment, reported Michael C. Monuteaux, Sc.D., of Harvard Medical School, Boston.
Children who were admitted to a patient floor or to an intensive care unit on their initial visit were twice as likely as those who were treated and released to be readmitted on subsequent ED visits. Children under 5 years of age were the most vulnerable, the authors found.
"Even when maltreatment is identified in the ED, children are at risk for further victimization resulting in future ED care," Dr. Monuteaux said at the annual meeting of the Pediatric Academic Societies.
Coinvestigator Dr. Daniel M. Lindberg, an emergency physician at Brigham and Women’s Hospital in Boston, said in an interview that the Child Protective Services workers have "a tremendously difficult" job made even more difficult by increasing caseloads and proposed reductions in funding.
"If that happens, [there will be] fewer investigators or case workers who can do the kind of checking in to make sure that safety plans are being followed or dangerous people are kept away from kids at risk. My hope is that any intervention to support Child Protective Services workers, and decrease caseloads, will help decrease rates of recurrent abuse," he said.
Dr. Monuteaux and Dr. Lindberg took a retrospective look at data from an administrative database on children under 18 treated in the emergency departments of 41 U.S. hospitals in 2005-2010.
They identified 43,824 ED visits by 42,354 children with one or more ICD-9 principal or secondary diagnoses of physical or sexual abuse, or other/unspecified maltreatment, and used medical record numbers to track patients over time.
In all, 1,286 maltreated children (3.0%) returned for another ED visit and received a second diagnosis of maltreatment. The median age of the children was 3 years (range, 1-8 years), 63% were girls, and 60% were white. The majority of the children (90%) had two ED visits, 8% had three visits, and 2% were seen in the ED four or more times.
One-fourth of the returning patients were seen again in the emergency department within 21 days, half within 150 days, and two-thirds within 1 year.
Abuse and neglect was the primary diagnosis in 38%, sexual abuse in 18%, physical abuse in 17%, and other maltreatment or injury in 27%.
Overall, 20% were admitted to the hospital at the initial visit, 3% were admitted to an ICU, and 6% underwent surgery for their injuries.
Of 253 children admitted at the initial visit, 42% were also admitted on their second visit. In comparison, of the 1,033 children not admitted at their first ED visit, 7% were admitted on the second visit. The odds ratio (OR) for being admitted a second time after a first admission was 2.1 (95% confidence interval [CI], 1.6-2.8).
Similarly, of 78 children with an initial ICU stay, 17% went back to the ICU at the second ED visit, compared with 2% of those who were not put in intensive care at their first ED visit (OR, 2.2; 95% CI, 1.4-3.6).
In a multivariate analysis controlled for demographic and clinical factors, the only significant predictor of repeat ED visits was age younger than 5 years (OR, 1.47; 95% CI, 1.22-1.78).
Dr. Monuteaux noted that the study might underestimate the actual number of repeat abuse cases because of its reliance on ICD-9 codes and because some of the children may have had ED visits for abuse or neglect before the start of the study. It is also possible that the code for physical abuse reflects long-term complications from prior abuse and not a new episode. Additionally, the data were drawn from academic pediatric hospitals and may not reflect the experience of community and general hospitals.
"Despite the dedicated work of ED and child protection workers, children diagnosed with maltreatment in the ED are at risk for additional victimization and subsequent emergency care for maltreatment, which leads us to suggest that improvements in the child protection apparatus should be considered," Dr. Monuteaux concluded.
The study was internally funded. The authors reported having no relevant financial relationships.
BOSTON – Children treated in the emergency department for abuse or neglect are at increased risk for further maltreatment, even after medical or social service intervention, a study has shown.
Among nearly 44,000 pediatric emergency department (ED) visits with at least one ICD-9 code for maltreatment, 3% of the children returned one or more times and were again identified as victims of maltreatment, reported Michael C. Monuteaux, Sc.D., of Harvard Medical School, Boston.
Children who were admitted to a patient floor or to an intensive care unit on their initial visit were twice as likely as those who were treated and released to be readmitted on subsequent ED visits. Children under 5 years of age were the most vulnerable, the authors found.
"Even when maltreatment is identified in the ED, children are at risk for further victimization resulting in future ED care," Dr. Monuteaux said at the annual meeting of the Pediatric Academic Societies.
Coinvestigator Dr. Daniel M. Lindberg, an emergency physician at Brigham and Women’s Hospital in Boston, said in an interview that the Child Protective Services workers have "a tremendously difficult" job made even more difficult by increasing caseloads and proposed reductions in funding.
"If that happens, [there will be] fewer investigators or case workers who can do the kind of checking in to make sure that safety plans are being followed or dangerous people are kept away from kids at risk. My hope is that any intervention to support Child Protective Services workers, and decrease caseloads, will help decrease rates of recurrent abuse," he said.
Dr. Monuteaux and Dr. Lindberg took a retrospective look at data from an administrative database on children under 18 treated in the emergency departments of 41 U.S. hospitals in 2005-2010.
They identified 43,824 ED visits by 42,354 children with one or more ICD-9 principal or secondary diagnoses of physical or sexual abuse, or other/unspecified maltreatment, and used medical record numbers to track patients over time.
In all, 1,286 maltreated children (3.0%) returned for another ED visit and received a second diagnosis of maltreatment. The median age of the children was 3 years (range, 1-8 years), 63% were girls, and 60% were white. The majority of the children (90%) had two ED visits, 8% had three visits, and 2% were seen in the ED four or more times.
One-fourth of the returning patients were seen again in the emergency department within 21 days, half within 150 days, and two-thirds within 1 year.
Abuse and neglect was the primary diagnosis in 38%, sexual abuse in 18%, physical abuse in 17%, and other maltreatment or injury in 27%.
Overall, 20% were admitted to the hospital at the initial visit, 3% were admitted to an ICU, and 6% underwent surgery for their injuries.
Of 253 children admitted at the initial visit, 42% were also admitted on their second visit. In comparison, of the 1,033 children not admitted at their first ED visit, 7% were admitted on the second visit. The odds ratio (OR) for being admitted a second time after a first admission was 2.1 (95% confidence interval [CI], 1.6-2.8).
Similarly, of 78 children with an initial ICU stay, 17% went back to the ICU at the second ED visit, compared with 2% of those who were not put in intensive care at their first ED visit (OR, 2.2; 95% CI, 1.4-3.6).
In a multivariate analysis controlled for demographic and clinical factors, the only significant predictor of repeat ED visits was age younger than 5 years (OR, 1.47; 95% CI, 1.22-1.78).
Dr. Monuteaux noted that the study might underestimate the actual number of repeat abuse cases because of its reliance on ICD-9 codes and because some of the children may have had ED visits for abuse or neglect before the start of the study. It is also possible that the code for physical abuse reflects long-term complications from prior abuse and not a new episode. Additionally, the data were drawn from academic pediatric hospitals and may not reflect the experience of community and general hospitals.
"Despite the dedicated work of ED and child protection workers, children diagnosed with maltreatment in the ED are at risk for additional victimization and subsequent emergency care for maltreatment, which leads us to suggest that improvements in the child protection apparatus should be considered," Dr. Monuteaux concluded.
The study was internally funded. The authors reported having no relevant financial relationships.
Michael C. Monuteaux, Sc.D., intensive care unit, Children under 5 years of age, maltreatment identified in the ED, Pediatric Academic Societies, Dr. Daniel M. Lindberg, Child Protective Services,
Michael C. Monuteaux, Sc.D., intensive care unit, Children under 5 years of age, maltreatment identified in the ED, Pediatric Academic Societies, Dr. Daniel M. Lindberg, Child Protective Services,
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: In all, 3% of abused or neglected children treated in the emergency department will return with a second diagnosis of maltreatment, often within a year of the first visit.
Data Source: The retrospective study drew on data from pediatric divisions of 41 U.S. academic medical centers.
Disclosures: The study was internally funded. The authors reported having no relevant financial relationships.
Consider Narrow Fluconazole Strategy if Candida Incidence Is Low
BOSTON – A narrow, targeted approach to fluconazole prophylaxis prevents most cases of neonatal candidiasis among extremely low-birth-weight infants in centers with a low incidence of the fungal infection, a study has shown.
Because of the high rates of mortality and neurodevelopmental impairment associated with candidiasis infection in at-risk infants, the Infectious Diseases Society of America recommends that centers with a high incidence of the infection consider routine fluconazole prophylaxis for extremely low-birth-weight neonates (less than 1,000 g at birth). The recommendation does not extend to low-incidence centers, however, because of the unknown risks for neurologic and cognitive disorders after fluconazole exposure in premature infants, said Dr. Karen M. Puopolo, a neonatologist at Brigham and Women’s Hospital in Boston.
To assess the theoretical efficacy of fluconazole prophylaxis in extremely low-birth-weight (ELBW) infants in a low-incidence center, Dr. Puopolo and her colleagues reviewed the clinical details of blood culture–proven neonatal Candida infections that occurred in a single tertiary care neonatal intensive care unit (NICU) from January 2003 to October 2010.
Using demographic data and antibiotic exposure information gleaned from medical and administrative records of nearly 1,400 ELBW infants, "we developed four different possible criteria for fluconazole prophylaxis, including fluconazole prophylaxis for all babies born with a birth weight less than 1,000 g, all babies born with a birth weight less than 1,000 g who also received 7 or more days of antibiotics, all babies born with a birth weight less than 750 g, and all babies born with a birth weight less than 750 g who also received 7 or more days of antibiotics," she explained at the annual meeting of the Pediatric Academic Societies.
For the number needed to treat (NNT) calculations, the investigators assumed that fluconazole prophylaxis would be 100% effective, and for the antibiotic exposure calculation, which was based on a review of antibiotic use in the NICU, they assumed that 50% of the infants with a birth weight less than 1,000 g and 80% with a birth weight less than 750 g would be treated with antibiotics for 7 or more days, Dr. Puopolo said.
During the period of study, 1,381 ELBW infants were exposed to fluconazole prophylaxis, including 878 weighing less than 1,000 g at birth, of which 293 had a minimum of 7 days of antibiotic therapy, and 393 weighing less than 750 g at birth, of which 179 had a minimum of 7 days of antibiotic therapy, Dr. Puopolo said. "Twenty cases of neonatal candidiasis were identified, with 18 [3%] occurring in ELBW infants surviving beyond 72 hours of life," she said. The mean birth weight of the infected infants was 702 g, and the mean gestational age and age at infection were 24.5 weeks and 21.4 weeks.
With respect to the number needed to treat analysis, the narrowest targeted approach – routine fluconazole prophylaxis in neonates weighing less than 750 g who had been exposed to a minimum of 7 days of antibiotic therapy – was the most efficient. In this subgroup, according to Dr. Puopolo, "we would need to treat 13 infants to prevent one fungal infection." The NNT in the 750-g, 1000-g with 7 or more days of antibiotic exposure, and 1,000-g groups were 15, 19, and 33, respectively.
If this approach were applied to the number of babies in each of the four prophylaxis categories, all 18 infections would have been targeted in the most liberal exposure group, while 567 of the babies would have been unnecessarily exposed to the antifungal drug. In the increasingly narrower exposure groups, 16, 15, and 14 of the infections would have been targeted. Although 2, 3, and 4 of the infections, respectively, would have been missed in these groups, far fewer babies would have been unnecessarily exposed to fluconazole, said Dr. Puopolo.
National guidelines do not recommend fluconazole prophylaxis in centers with a lower-than-average incidence of neonatal invasive Candida infections in the NICU, but "our findings suggest that individual NICUs should consider different approaches to fluconazole prophylaxis based on their incidence of candidiasis," Dr. Puopolo said. "A narrow targeted approach can prevent most cases of neonatal candidiasis with the lowest number needed to treat."
Dr. Puopolo said she had no relevant financial disclosures.
BOSTON – A narrow, targeted approach to fluconazole prophylaxis prevents most cases of neonatal candidiasis among extremely low-birth-weight infants in centers with a low incidence of the fungal infection, a study has shown.
Because of the high rates of mortality and neurodevelopmental impairment associated with candidiasis infection in at-risk infants, the Infectious Diseases Society of America recommends that centers with a high incidence of the infection consider routine fluconazole prophylaxis for extremely low-birth-weight neonates (less than 1,000 g at birth). The recommendation does not extend to low-incidence centers, however, because of the unknown risks for neurologic and cognitive disorders after fluconazole exposure in premature infants, said Dr. Karen M. Puopolo, a neonatologist at Brigham and Women’s Hospital in Boston.
To assess the theoretical efficacy of fluconazole prophylaxis in extremely low-birth-weight (ELBW) infants in a low-incidence center, Dr. Puopolo and her colleagues reviewed the clinical details of blood culture–proven neonatal Candida infections that occurred in a single tertiary care neonatal intensive care unit (NICU) from January 2003 to October 2010.
Using demographic data and antibiotic exposure information gleaned from medical and administrative records of nearly 1,400 ELBW infants, "we developed four different possible criteria for fluconazole prophylaxis, including fluconazole prophylaxis for all babies born with a birth weight less than 1,000 g, all babies born with a birth weight less than 1,000 g who also received 7 or more days of antibiotics, all babies born with a birth weight less than 750 g, and all babies born with a birth weight less than 750 g who also received 7 or more days of antibiotics," she explained at the annual meeting of the Pediatric Academic Societies.
For the number needed to treat (NNT) calculations, the investigators assumed that fluconazole prophylaxis would be 100% effective, and for the antibiotic exposure calculation, which was based on a review of antibiotic use in the NICU, they assumed that 50% of the infants with a birth weight less than 1,000 g and 80% with a birth weight less than 750 g would be treated with antibiotics for 7 or more days, Dr. Puopolo said.
During the period of study, 1,381 ELBW infants were exposed to fluconazole prophylaxis, including 878 weighing less than 1,000 g at birth, of which 293 had a minimum of 7 days of antibiotic therapy, and 393 weighing less than 750 g at birth, of which 179 had a minimum of 7 days of antibiotic therapy, Dr. Puopolo said. "Twenty cases of neonatal candidiasis were identified, with 18 [3%] occurring in ELBW infants surviving beyond 72 hours of life," she said. The mean birth weight of the infected infants was 702 g, and the mean gestational age and age at infection were 24.5 weeks and 21.4 weeks.
With respect to the number needed to treat analysis, the narrowest targeted approach – routine fluconazole prophylaxis in neonates weighing less than 750 g who had been exposed to a minimum of 7 days of antibiotic therapy – was the most efficient. In this subgroup, according to Dr. Puopolo, "we would need to treat 13 infants to prevent one fungal infection." The NNT in the 750-g, 1000-g with 7 or more days of antibiotic exposure, and 1,000-g groups were 15, 19, and 33, respectively.
If this approach were applied to the number of babies in each of the four prophylaxis categories, all 18 infections would have been targeted in the most liberal exposure group, while 567 of the babies would have been unnecessarily exposed to the antifungal drug. In the increasingly narrower exposure groups, 16, 15, and 14 of the infections would have been targeted. Although 2, 3, and 4 of the infections, respectively, would have been missed in these groups, far fewer babies would have been unnecessarily exposed to fluconazole, said Dr. Puopolo.
National guidelines do not recommend fluconazole prophylaxis in centers with a lower-than-average incidence of neonatal invasive Candida infections in the NICU, but "our findings suggest that individual NICUs should consider different approaches to fluconazole prophylaxis based on their incidence of candidiasis," Dr. Puopolo said. "A narrow targeted approach can prevent most cases of neonatal candidiasis with the lowest number needed to treat."
Dr. Puopolo said she had no relevant financial disclosures.
BOSTON – A narrow, targeted approach to fluconazole prophylaxis prevents most cases of neonatal candidiasis among extremely low-birth-weight infants in centers with a low incidence of the fungal infection, a study has shown.
Because of the high rates of mortality and neurodevelopmental impairment associated with candidiasis infection in at-risk infants, the Infectious Diseases Society of America recommends that centers with a high incidence of the infection consider routine fluconazole prophylaxis for extremely low-birth-weight neonates (less than 1,000 g at birth). The recommendation does not extend to low-incidence centers, however, because of the unknown risks for neurologic and cognitive disorders after fluconazole exposure in premature infants, said Dr. Karen M. Puopolo, a neonatologist at Brigham and Women’s Hospital in Boston.
To assess the theoretical efficacy of fluconazole prophylaxis in extremely low-birth-weight (ELBW) infants in a low-incidence center, Dr. Puopolo and her colleagues reviewed the clinical details of blood culture–proven neonatal Candida infections that occurred in a single tertiary care neonatal intensive care unit (NICU) from January 2003 to October 2010.
Using demographic data and antibiotic exposure information gleaned from medical and administrative records of nearly 1,400 ELBW infants, "we developed four different possible criteria for fluconazole prophylaxis, including fluconazole prophylaxis for all babies born with a birth weight less than 1,000 g, all babies born with a birth weight less than 1,000 g who also received 7 or more days of antibiotics, all babies born with a birth weight less than 750 g, and all babies born with a birth weight less than 750 g who also received 7 or more days of antibiotics," she explained at the annual meeting of the Pediatric Academic Societies.
For the number needed to treat (NNT) calculations, the investigators assumed that fluconazole prophylaxis would be 100% effective, and for the antibiotic exposure calculation, which was based on a review of antibiotic use in the NICU, they assumed that 50% of the infants with a birth weight less than 1,000 g and 80% with a birth weight less than 750 g would be treated with antibiotics for 7 or more days, Dr. Puopolo said.
During the period of study, 1,381 ELBW infants were exposed to fluconazole prophylaxis, including 878 weighing less than 1,000 g at birth, of which 293 had a minimum of 7 days of antibiotic therapy, and 393 weighing less than 750 g at birth, of which 179 had a minimum of 7 days of antibiotic therapy, Dr. Puopolo said. "Twenty cases of neonatal candidiasis were identified, with 18 [3%] occurring in ELBW infants surviving beyond 72 hours of life," she said. The mean birth weight of the infected infants was 702 g, and the mean gestational age and age at infection were 24.5 weeks and 21.4 weeks.
With respect to the number needed to treat analysis, the narrowest targeted approach – routine fluconazole prophylaxis in neonates weighing less than 750 g who had been exposed to a minimum of 7 days of antibiotic therapy – was the most efficient. In this subgroup, according to Dr. Puopolo, "we would need to treat 13 infants to prevent one fungal infection." The NNT in the 750-g, 1000-g with 7 or more days of antibiotic exposure, and 1,000-g groups were 15, 19, and 33, respectively.
If this approach were applied to the number of babies in each of the four prophylaxis categories, all 18 infections would have been targeted in the most liberal exposure group, while 567 of the babies would have been unnecessarily exposed to the antifungal drug. In the increasingly narrower exposure groups, 16, 15, and 14 of the infections would have been targeted. Although 2, 3, and 4 of the infections, respectively, would have been missed in these groups, far fewer babies would have been unnecessarily exposed to fluconazole, said Dr. Puopolo.
National guidelines do not recommend fluconazole prophylaxis in centers with a lower-than-average incidence of neonatal invasive Candida infections in the NICU, but "our findings suggest that individual NICUs should consider different approaches to fluconazole prophylaxis based on their incidence of candidiasis," Dr. Puopolo said. "A narrow targeted approach can prevent most cases of neonatal candidiasis with the lowest number needed to treat."
Dr. Puopolo said she had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: In 179 premature neonates weighing 750 g who received at least 7 days of antibiotic therapy, fluconazole prophylaxis would have targeted 14 of 18 invasive Candida infections, based on the findings of a theoretical efficacy evaluation showing the number of prophylaxis exposures needed to prevent 1 such infection in this patient group was 13. In contrast, the number needed to treat in a broader group of all neonates weighing 1,000 g at birth was 33.
Data Source: The medical and administrative records of nearly 1,400 ELBW babies in a single tertiary care NICU were reviewed to determine the theoretical efficacy of various fluconazole prophylaxis practices.
Disclosures: Dr. Puopolo said she had no relevant financial disclosures.
Prenatal Screen Predicts Maternal Risk of Traumatic Death
BOSTON – A screening tool designed to identify medical and psychosocial risk factors associated with poor pregnancy outcomes also seems to predict maternal traumatic pregnancy–associated death, according to Dr. Nancy S. Hardt.
The Florida Healthy Start Prenatal Risk Screen has been validated for the identification of women who are at risk for preterm delivery or for delivering a low-birth-weight infant. Even low levels of risk on the screening test, which has been offered to all pregnant women in Florida at their first prenatal visit as per state legislative statute since 1991, appear to be associated with an increased likelihood of traumatic maternal death, Dr. Hardt said at the annual meeting of the Pediatric Academic Societies.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death," she said. "It doesn’t take a whole lot of practice change to address some of the factors that might be putting the moms at risk, such as dispelling the myth that pregnant women shouldn’t wear seatbelts, asking patients if they feel safe in their homes, and stressing the dangers of substance use and abuse, including prescription drug use."
Dr. Hardt and her colleagues reviewed 600,000 Healthy Start screens from 1999 to 2005, as well as linked data for the concurrent period from Florida’s Enhanced Maternal Mortality Reporting Database. Of the women who died during the period of study, 144 experienced traumatic deaths. These included accidents, homicides, suicides, and drug overdoses, she said, noting that the top four causes of maternal deaths were trauma related.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death."
Specifically, the causes of death that had the greatest maternal mortality ratios were transport accidents (13.3), homicide (5.5), accidental poisoning (3.3), and suicide (2.9).
"We have to go through quite a few categories of traumatic deaths before we get to the obstetric-related deaths," such as hypertension disorders (2.7), hemorrhage (2.2), thrombotic embolism (2.2), and infection (2.0), observed Dr. Hardt, professor of pathology and ob.gyn. at the University of Florida in Gainesville.
To evaluate the predictive value of the Healthy Start screen for identifying risk of traumatic death, the investigators used the same screening threshold as that used for identifying women at risk for poor pregnancy outcomes, Dr. Hardt said. "A score of 4 or higher on the [15-item] weighted measure, which includes demographic as well as environmental and social factors, indicates a positive screen for risk of preterm or low-birth-weight delivery and triggers referral to Healthy Start services," Dr. Hardt explained. "We hypothesized that the risk factors for these infant problems would be the same as for maternal death, and as such the screening instruments would work for identifying at-risk moms."
An analysis of the data showed that as a woman’s risk score increased, the probability of traumatic death also increased. In fact, "a woman with a risk score of 4 had nearly 12 times the risk of traumatic death compared to a women with a risk score of zero, and a woman with a risk score of 9 had 52 times the risk of traumatic death compared to one who scored zero," Dr. Hardt said. "What we observed is that with each increase in score of 1, the relative risk of death increased 1.5 to 2 times."
What this means, in terms of a prediction tool, "is that for every 100,000 women with a score of 4, expect nearly 48 traumatic maternal deaths, and for every one with a score of 9, expect 215 traumatic deaths," according to Dr. Hardt.
Many of the specific risk determinants associated with poor pregnancy outcomes are likely the same as those that are predictive of maternal traumatic death, including mental health, substance use, domestic violence, education, and employment/family income status, Dr. Hardt said.
Dr. Hardt said she had no relevant financial disclosures.
BOSTON – A screening tool designed to identify medical and psychosocial risk factors associated with poor pregnancy outcomes also seems to predict maternal traumatic pregnancy–associated death, according to Dr. Nancy S. Hardt.
The Florida Healthy Start Prenatal Risk Screen has been validated for the identification of women who are at risk for preterm delivery or for delivering a low-birth-weight infant. Even low levels of risk on the screening test, which has been offered to all pregnant women in Florida at their first prenatal visit as per state legislative statute since 1991, appear to be associated with an increased likelihood of traumatic maternal death, Dr. Hardt said at the annual meeting of the Pediatric Academic Societies.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death," she said. "It doesn’t take a whole lot of practice change to address some of the factors that might be putting the moms at risk, such as dispelling the myth that pregnant women shouldn’t wear seatbelts, asking patients if they feel safe in their homes, and stressing the dangers of substance use and abuse, including prescription drug use."
Dr. Hardt and her colleagues reviewed 600,000 Healthy Start screens from 1999 to 2005, as well as linked data for the concurrent period from Florida’s Enhanced Maternal Mortality Reporting Database. Of the women who died during the period of study, 144 experienced traumatic deaths. These included accidents, homicides, suicides, and drug overdoses, she said, noting that the top four causes of maternal deaths were trauma related.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death."
Specifically, the causes of death that had the greatest maternal mortality ratios were transport accidents (13.3), homicide (5.5), accidental poisoning (3.3), and suicide (2.9).
"We have to go through quite a few categories of traumatic deaths before we get to the obstetric-related deaths," such as hypertension disorders (2.7), hemorrhage (2.2), thrombotic embolism (2.2), and infection (2.0), observed Dr. Hardt, professor of pathology and ob.gyn. at the University of Florida in Gainesville.
To evaluate the predictive value of the Healthy Start screen for identifying risk of traumatic death, the investigators used the same screening threshold as that used for identifying women at risk for poor pregnancy outcomes, Dr. Hardt said. "A score of 4 or higher on the [15-item] weighted measure, which includes demographic as well as environmental and social factors, indicates a positive screen for risk of preterm or low-birth-weight delivery and triggers referral to Healthy Start services," Dr. Hardt explained. "We hypothesized that the risk factors for these infant problems would be the same as for maternal death, and as such the screening instruments would work for identifying at-risk moms."
An analysis of the data showed that as a woman’s risk score increased, the probability of traumatic death also increased. In fact, "a woman with a risk score of 4 had nearly 12 times the risk of traumatic death compared to a women with a risk score of zero, and a woman with a risk score of 9 had 52 times the risk of traumatic death compared to one who scored zero," Dr. Hardt said. "What we observed is that with each increase in score of 1, the relative risk of death increased 1.5 to 2 times."
What this means, in terms of a prediction tool, "is that for every 100,000 women with a score of 4, expect nearly 48 traumatic maternal deaths, and for every one with a score of 9, expect 215 traumatic deaths," according to Dr. Hardt.
Many of the specific risk determinants associated with poor pregnancy outcomes are likely the same as those that are predictive of maternal traumatic death, including mental health, substance use, domestic violence, education, and employment/family income status, Dr. Hardt said.
Dr. Hardt said she had no relevant financial disclosures.
BOSTON – A screening tool designed to identify medical and psychosocial risk factors associated with poor pregnancy outcomes also seems to predict maternal traumatic pregnancy–associated death, according to Dr. Nancy S. Hardt.
The Florida Healthy Start Prenatal Risk Screen has been validated for the identification of women who are at risk for preterm delivery or for delivering a low-birth-weight infant. Even low levels of risk on the screening test, which has been offered to all pregnant women in Florida at their first prenatal visit as per state legislative statute since 1991, appear to be associated with an increased likelihood of traumatic maternal death, Dr. Hardt said at the annual meeting of the Pediatric Academic Societies.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death," she said. "It doesn’t take a whole lot of practice change to address some of the factors that might be putting the moms at risk, such as dispelling the myth that pregnant women shouldn’t wear seatbelts, asking patients if they feel safe in their homes, and stressing the dangers of substance use and abuse, including prescription drug use."
Dr. Hardt and her colleagues reviewed 600,000 Healthy Start screens from 1999 to 2005, as well as linked data for the concurrent period from Florida’s Enhanced Maternal Mortality Reporting Database. Of the women who died during the period of study, 144 experienced traumatic deaths. These included accidents, homicides, suicides, and drug overdoses, she said, noting that the top four causes of maternal deaths were trauma related.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death."
Specifically, the causes of death that had the greatest maternal mortality ratios were transport accidents (13.3), homicide (5.5), accidental poisoning (3.3), and suicide (2.9).
"We have to go through quite a few categories of traumatic deaths before we get to the obstetric-related deaths," such as hypertension disorders (2.7), hemorrhage (2.2), thrombotic embolism (2.2), and infection (2.0), observed Dr. Hardt, professor of pathology and ob.gyn. at the University of Florida in Gainesville.
To evaluate the predictive value of the Healthy Start screen for identifying risk of traumatic death, the investigators used the same screening threshold as that used for identifying women at risk for poor pregnancy outcomes, Dr. Hardt said. "A score of 4 or higher on the [15-item] weighted measure, which includes demographic as well as environmental and social factors, indicates a positive screen for risk of preterm or low-birth-weight delivery and triggers referral to Healthy Start services," Dr. Hardt explained. "We hypothesized that the risk factors for these infant problems would be the same as for maternal death, and as such the screening instruments would work for identifying at-risk moms."
An analysis of the data showed that as a woman’s risk score increased, the probability of traumatic death also increased. In fact, "a woman with a risk score of 4 had nearly 12 times the risk of traumatic death compared to a women with a risk score of zero, and a woman with a risk score of 9 had 52 times the risk of traumatic death compared to one who scored zero," Dr. Hardt said. "What we observed is that with each increase in score of 1, the relative risk of death increased 1.5 to 2 times."
What this means, in terms of a prediction tool, "is that for every 100,000 women with a score of 4, expect nearly 48 traumatic maternal deaths, and for every one with a score of 9, expect 215 traumatic deaths," according to Dr. Hardt.
Many of the specific risk determinants associated with poor pregnancy outcomes are likely the same as those that are predictive of maternal traumatic death, including mental health, substance use, domestic violence, education, and employment/family income status, Dr. Hardt said.
Dr. Hardt said she had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Following Concussions, Give Kids' Brains a Rest
BOSTON – Children who present to a primary care practice following a head or facial injury must be carefully evaluated for signs and symptoms of concussion, and those with concussion should be advised to give their brains a break, recommended a pediatric injury specialist at the annual meeting of the Pediatric Academic Societies.
Cognitive rest involves limiting "cognitive activity to a level that does not elicit symptoms." For children, this means forgoing computers, video games, texting/social media, reading for school and/or homework, and avoiding noisy or busy environments.
"The primary focus of pediatric concussion management should be return to cognitive activities and then return to the playing field," Dr. Kristy B. Arbogast said.
A review of records from a large pediatric primary care network showed that 25% of patients with concussion symptoms did not have concussion mentioned in the medical assessment or diagnosis, and nearly half of children in a random sample presented for reevaluation of concussion or persistent concussion symptoms, said Dr. Arbogast, an emergency physician and director of the Pediatric Injury Prevention Program at Children’s Hospital of Philadelphia.
"So-called ‘mild’ traumatic brain injuries are often far from mild. They lead to poor neurological outcomes that can adversely affect a child’s quality of life," she said.
Children with concussion make an estimated 144,000 emergency department visits annually in the United States. As children’s participation in year-round sports has increased, their risk of mild traumatic brain injury (TBI) has also increased, Dr. Arbogast noted.
Concussions among professional athletes receive considerable attention in the popular press, where the stories center on physical recovery and returning to the game. But for school kids, who are at significant risk for learning disabilities, memory problems, and emotional or behavioral changes after a TBI, the focus should be on physical and cognitive rest, she said.
Dr. Arbogast and her colleagues reviewed the concussion management and return-to-school practices of pediatric primary care providers by reviewing records from their hospital’s primary care network.
They looked for data on children aged 5-18 years with any presentation of mild TBI based on ICD-9 codes for skull fracture, concussion, intracranial injury, head injury (unspecified), or facial fracture. The children received initial or continuing care during the study period of July 2010 through June 2011.
The researchers included children who presented with one or more injury characteristics such as amnesia, loss of consciousness, cognitive symptoms (decline in school performance, report of being "in a fog"), emotional symptoms, and physical symptoms or exam findings including eye-tracking problems, headache, nausea/vomiting, poor balance, sleep disturbances, slow reaction times, or visual disturbance. Children with moderate or severe head trauma were excluded from the study.
The investigators randomly selected a sample of 193 patients who met all of the criteria. In all, 51% had a sports-related injury, 8% had previously had a concussion, and 6% had sustained a loss of consciousness.
There was no mention of concussion in the medical assessment or diagnosis of 25% of the sample. Of 94 children who presented for reevaluation of concussion, 33% reported a decline in school performance, 13% said they felt like they were "in a fog," 12% reported vision problems, 12% reported fatigue, and 11% had concentration problems (some reported more than one symptom).
When the authors looked at the written instructions primary care providers gave to the patients, they found that while 54% received return-to-play instructions, only 34% received return-to-school instructions, suggesting that in many cases the practitioners may have failed to recognize the importance of cognitive rest, Dr. Arbogast said. The remaining 12% of patients did not have written instructions documented.
She recommended that clinicians caring for children with suspected concussion ask about all symptoms individually in a systematic fashion, and prescribe a return-to-school protocol with a stepwise approach. The protocol includes a return to the previous step if an action elicits the return of symptoms, sending a standardized letter to notify the child’s school of the plan, and training the child’s parent or guardian to oversee the child’s progression from one step to the next.
The study was funded by the Children’s Hospital of Philadelphia and the University of Pennsylvania, also in Philadelphia. Dr. Arbogast and coinvestigators reported having no conflicts of interest to disclose.
BOSTON – Children who present to a primary care practice following a head or facial injury must be carefully evaluated for signs and symptoms of concussion, and those with concussion should be advised to give their brains a break, recommended a pediatric injury specialist at the annual meeting of the Pediatric Academic Societies.
Cognitive rest involves limiting "cognitive activity to a level that does not elicit symptoms." For children, this means forgoing computers, video games, texting/social media, reading for school and/or homework, and avoiding noisy or busy environments.
"The primary focus of pediatric concussion management should be return to cognitive activities and then return to the playing field," Dr. Kristy B. Arbogast said.
A review of records from a large pediatric primary care network showed that 25% of patients with concussion symptoms did not have concussion mentioned in the medical assessment or diagnosis, and nearly half of children in a random sample presented for reevaluation of concussion or persistent concussion symptoms, said Dr. Arbogast, an emergency physician and director of the Pediatric Injury Prevention Program at Children’s Hospital of Philadelphia.
"So-called ‘mild’ traumatic brain injuries are often far from mild. They lead to poor neurological outcomes that can adversely affect a child’s quality of life," she said.
Children with concussion make an estimated 144,000 emergency department visits annually in the United States. As children’s participation in year-round sports has increased, their risk of mild traumatic brain injury (TBI) has also increased, Dr. Arbogast noted.
Concussions among professional athletes receive considerable attention in the popular press, where the stories center on physical recovery and returning to the game. But for school kids, who are at significant risk for learning disabilities, memory problems, and emotional or behavioral changes after a TBI, the focus should be on physical and cognitive rest, she said.
Dr. Arbogast and her colleagues reviewed the concussion management and return-to-school practices of pediatric primary care providers by reviewing records from their hospital’s primary care network.
They looked for data on children aged 5-18 years with any presentation of mild TBI based on ICD-9 codes for skull fracture, concussion, intracranial injury, head injury (unspecified), or facial fracture. The children received initial or continuing care during the study period of July 2010 through June 2011.
The researchers included children who presented with one or more injury characteristics such as amnesia, loss of consciousness, cognitive symptoms (decline in school performance, report of being "in a fog"), emotional symptoms, and physical symptoms or exam findings including eye-tracking problems, headache, nausea/vomiting, poor balance, sleep disturbances, slow reaction times, or visual disturbance. Children with moderate or severe head trauma were excluded from the study.
The investigators randomly selected a sample of 193 patients who met all of the criteria. In all, 51% had a sports-related injury, 8% had previously had a concussion, and 6% had sustained a loss of consciousness.
There was no mention of concussion in the medical assessment or diagnosis of 25% of the sample. Of 94 children who presented for reevaluation of concussion, 33% reported a decline in school performance, 13% said they felt like they were "in a fog," 12% reported vision problems, 12% reported fatigue, and 11% had concentration problems (some reported more than one symptom).
When the authors looked at the written instructions primary care providers gave to the patients, they found that while 54% received return-to-play instructions, only 34% received return-to-school instructions, suggesting that in many cases the practitioners may have failed to recognize the importance of cognitive rest, Dr. Arbogast said. The remaining 12% of patients did not have written instructions documented.
She recommended that clinicians caring for children with suspected concussion ask about all symptoms individually in a systematic fashion, and prescribe a return-to-school protocol with a stepwise approach. The protocol includes a return to the previous step if an action elicits the return of symptoms, sending a standardized letter to notify the child’s school of the plan, and training the child’s parent or guardian to oversee the child’s progression from one step to the next.
The study was funded by the Children’s Hospital of Philadelphia and the University of Pennsylvania, also in Philadelphia. Dr. Arbogast and coinvestigators reported having no conflicts of interest to disclose.
BOSTON – Children who present to a primary care practice following a head or facial injury must be carefully evaluated for signs and symptoms of concussion, and those with concussion should be advised to give their brains a break, recommended a pediatric injury specialist at the annual meeting of the Pediatric Academic Societies.
Cognitive rest involves limiting "cognitive activity to a level that does not elicit symptoms." For children, this means forgoing computers, video games, texting/social media, reading for school and/or homework, and avoiding noisy or busy environments.
"The primary focus of pediatric concussion management should be return to cognitive activities and then return to the playing field," Dr. Kristy B. Arbogast said.
A review of records from a large pediatric primary care network showed that 25% of patients with concussion symptoms did not have concussion mentioned in the medical assessment or diagnosis, and nearly half of children in a random sample presented for reevaluation of concussion or persistent concussion symptoms, said Dr. Arbogast, an emergency physician and director of the Pediatric Injury Prevention Program at Children’s Hospital of Philadelphia.
"So-called ‘mild’ traumatic brain injuries are often far from mild. They lead to poor neurological outcomes that can adversely affect a child’s quality of life," she said.
Children with concussion make an estimated 144,000 emergency department visits annually in the United States. As children’s participation in year-round sports has increased, their risk of mild traumatic brain injury (TBI) has also increased, Dr. Arbogast noted.
Concussions among professional athletes receive considerable attention in the popular press, where the stories center on physical recovery and returning to the game. But for school kids, who are at significant risk for learning disabilities, memory problems, and emotional or behavioral changes after a TBI, the focus should be on physical and cognitive rest, she said.
Dr. Arbogast and her colleagues reviewed the concussion management and return-to-school practices of pediatric primary care providers by reviewing records from their hospital’s primary care network.
They looked for data on children aged 5-18 years with any presentation of mild TBI based on ICD-9 codes for skull fracture, concussion, intracranial injury, head injury (unspecified), or facial fracture. The children received initial or continuing care during the study period of July 2010 through June 2011.
The researchers included children who presented with one or more injury characteristics such as amnesia, loss of consciousness, cognitive symptoms (decline in school performance, report of being "in a fog"), emotional symptoms, and physical symptoms or exam findings including eye-tracking problems, headache, nausea/vomiting, poor balance, sleep disturbances, slow reaction times, or visual disturbance. Children with moderate or severe head trauma were excluded from the study.
The investigators randomly selected a sample of 193 patients who met all of the criteria. In all, 51% had a sports-related injury, 8% had previously had a concussion, and 6% had sustained a loss of consciousness.
There was no mention of concussion in the medical assessment or diagnosis of 25% of the sample. Of 94 children who presented for reevaluation of concussion, 33% reported a decline in school performance, 13% said they felt like they were "in a fog," 12% reported vision problems, 12% reported fatigue, and 11% had concentration problems (some reported more than one symptom).
When the authors looked at the written instructions primary care providers gave to the patients, they found that while 54% received return-to-play instructions, only 34% received return-to-school instructions, suggesting that in many cases the practitioners may have failed to recognize the importance of cognitive rest, Dr. Arbogast said. The remaining 12% of patients did not have written instructions documented.
She recommended that clinicians caring for children with suspected concussion ask about all symptoms individually in a systematic fashion, and prescribe a return-to-school protocol with a stepwise approach. The protocol includes a return to the previous step if an action elicits the return of symptoms, sending a standardized letter to notify the child’s school of the plan, and training the child’s parent or guardian to oversee the child’s progression from one step to the next.
The study was funded by the Children’s Hospital of Philadelphia and the University of Pennsylvania, also in Philadelphia. Dr. Arbogast and coinvestigators reported having no conflicts of interest to disclose.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: About 25% of children who presented to a primary care practice with concussion symptoms did not have concussion mentioned in the medical assessment or diagnosis.
Data Source: The data were taken from a random sample of records from a pediatric primary care provider network.
Disclosures: The study was funded by the Children’s Hospital of Philadelphia and the University of Pennsylvania. Dr. Arbogast and coinvestigators reported having no conflicts of interest to disclose.
PCR Bests Culture at Identifying Congenital CMV Infections
BOSTON – A real-time saliva-based polymerase chain reaction assay identifies more newborns with congenital cytomegalovirus infections than a standard rapid-culture assay, investigators reported.
"A PCR [polymerase chain reaction]-based assay would be a better newborn screen as the sample is convenient and noninvasive to collect, and we have already shown that elimination of the DNA extraction step does not interfere with the sensitivity or the specificity of the assay," said Dr. Swetha Pinninti, a pediatric infectious disease fellow at the University of Alabama at Birmingham.
The PCR assay lends itself to high throughput methods, is less expensive than culturing, and could help clinicians identify an additional 400-1,200 infants with congenital cytomegalovirus (CMV) annually, Dr. Pinninti said at the annual meeting of the Pediatric Academic Societies.
Congenital CMV is the leading cause of nongenetic sensorineural hearing loss, but may go undetected, because approximately 90% of infected children have no clinical findings at birth. From 10%-15% of children who are infected but asymptomatic, and 60% of those who are symptomatic will develop hearing loss. In about one-third of cases, the development of sensorineural hearing loss has a delayed onset, Dr. Pinninti said.
Although detection of virus from culture of urine or saliva samples is the current gold standard, the investigators previously showed that PCR of saliva is comparable to culture-based methods (N. Engl. J. Med. 2011;364:2111-8).
In the current study, they tested whether saliva PCR could be a better screening tool for congenital CMV infection than rapid culture (RC)-based techniques.
To do so, they looked at two cohorts of infants. The first, screened from June 2008 through December 2009, included newborns who had saliva samples collected by swab and tested with both PCR and RC.
Due to a change of protocol, a second cohort of infants screened from January 2010 through November 2011 had saliva PCR testing, with RC performed on all samples that tested positive by PCR.
Infants who were positive for CMV by either screening were re-evaluated for confirmation, with testing of saliva and urine samples collected at enrollment. Infants confirmed to have congenital CMV infections were enrolled in follow-up to monitor their hearing outcomes.
Of the 35,334 infants screened in the first cohort, 161 tested positive for CMV and were enrolled for confirmation. Of this group, 152 had confirmed CMV, and 9 were confirmed to be CMV-negative.
Of the 152 confirmed CMV-positive, 147 were positive by both screening methods, 4 were PCR-positive but RC-negative, and 1 was PCR-negative but RC-positive,
In the second cohort, 37,250 infants were screened with PCR, and 123 were enrolled for confirmation. Of this group, 114 were confirmed to be CMV-positive, and 9 were confirmed to be CMV-negative. Of those confirmed positive, 105 were positive on both screening methods, and 9 were PCR-positive but RC-negative.
Of the 14 PCR/RC discordant samples, PCR detected CMV copies in varying amounts in 13, whereas RC detected cells in only 1 of the 14 (4 cells per slide).
Dr. Pinninti acknowledged a few study limitations, including the fact that infants with initially negative screens were not enrolled, and that samples were transported to a central lab, which could have degraded the quality of the cultured samples.
"This is really exciting," commented Dr. Morven S. Edwards, professor of pediatrics at Baylor College of Medicine, Houston, who comoderated the session in which the study was presented, but was not involved in the research.
The study was supported by the National Institute on Deafness and Other Communication Disorders. Dr. Pinninti and Dr. Edwards reported having no conflicts of interest.
BOSTON – A real-time saliva-based polymerase chain reaction assay identifies more newborns with congenital cytomegalovirus infections than a standard rapid-culture assay, investigators reported.
"A PCR [polymerase chain reaction]-based assay would be a better newborn screen as the sample is convenient and noninvasive to collect, and we have already shown that elimination of the DNA extraction step does not interfere with the sensitivity or the specificity of the assay," said Dr. Swetha Pinninti, a pediatric infectious disease fellow at the University of Alabama at Birmingham.
The PCR assay lends itself to high throughput methods, is less expensive than culturing, and could help clinicians identify an additional 400-1,200 infants with congenital cytomegalovirus (CMV) annually, Dr. Pinninti said at the annual meeting of the Pediatric Academic Societies.
Congenital CMV is the leading cause of nongenetic sensorineural hearing loss, but may go undetected, because approximately 90% of infected children have no clinical findings at birth. From 10%-15% of children who are infected but asymptomatic, and 60% of those who are symptomatic will develop hearing loss. In about one-third of cases, the development of sensorineural hearing loss has a delayed onset, Dr. Pinninti said.
Although detection of virus from culture of urine or saliva samples is the current gold standard, the investigators previously showed that PCR of saliva is comparable to culture-based methods (N. Engl. J. Med. 2011;364:2111-8).
In the current study, they tested whether saliva PCR could be a better screening tool for congenital CMV infection than rapid culture (RC)-based techniques.
To do so, they looked at two cohorts of infants. The first, screened from June 2008 through December 2009, included newborns who had saliva samples collected by swab and tested with both PCR and RC.
Due to a change of protocol, a second cohort of infants screened from January 2010 through November 2011 had saliva PCR testing, with RC performed on all samples that tested positive by PCR.
Infants who were positive for CMV by either screening were re-evaluated for confirmation, with testing of saliva and urine samples collected at enrollment. Infants confirmed to have congenital CMV infections were enrolled in follow-up to monitor their hearing outcomes.
Of the 35,334 infants screened in the first cohort, 161 tested positive for CMV and were enrolled for confirmation. Of this group, 152 had confirmed CMV, and 9 were confirmed to be CMV-negative.
Of the 152 confirmed CMV-positive, 147 were positive by both screening methods, 4 were PCR-positive but RC-negative, and 1 was PCR-negative but RC-positive,
In the second cohort, 37,250 infants were screened with PCR, and 123 were enrolled for confirmation. Of this group, 114 were confirmed to be CMV-positive, and 9 were confirmed to be CMV-negative. Of those confirmed positive, 105 were positive on both screening methods, and 9 were PCR-positive but RC-negative.
Of the 14 PCR/RC discordant samples, PCR detected CMV copies in varying amounts in 13, whereas RC detected cells in only 1 of the 14 (4 cells per slide).
Dr. Pinninti acknowledged a few study limitations, including the fact that infants with initially negative screens were not enrolled, and that samples were transported to a central lab, which could have degraded the quality of the cultured samples.
"This is really exciting," commented Dr. Morven S. Edwards, professor of pediatrics at Baylor College of Medicine, Houston, who comoderated the session in which the study was presented, but was not involved in the research.
The study was supported by the National Institute on Deafness and Other Communication Disorders. Dr. Pinninti and Dr. Edwards reported having no conflicts of interest.
BOSTON – A real-time saliva-based polymerase chain reaction assay identifies more newborns with congenital cytomegalovirus infections than a standard rapid-culture assay, investigators reported.
"A PCR [polymerase chain reaction]-based assay would be a better newborn screen as the sample is convenient and noninvasive to collect, and we have already shown that elimination of the DNA extraction step does not interfere with the sensitivity or the specificity of the assay," said Dr. Swetha Pinninti, a pediatric infectious disease fellow at the University of Alabama at Birmingham.
The PCR assay lends itself to high throughput methods, is less expensive than culturing, and could help clinicians identify an additional 400-1,200 infants with congenital cytomegalovirus (CMV) annually, Dr. Pinninti said at the annual meeting of the Pediatric Academic Societies.
Congenital CMV is the leading cause of nongenetic sensorineural hearing loss, but may go undetected, because approximately 90% of infected children have no clinical findings at birth. From 10%-15% of children who are infected but asymptomatic, and 60% of those who are symptomatic will develop hearing loss. In about one-third of cases, the development of sensorineural hearing loss has a delayed onset, Dr. Pinninti said.
Although detection of virus from culture of urine or saliva samples is the current gold standard, the investigators previously showed that PCR of saliva is comparable to culture-based methods (N. Engl. J. Med. 2011;364:2111-8).
In the current study, they tested whether saliva PCR could be a better screening tool for congenital CMV infection than rapid culture (RC)-based techniques.
To do so, they looked at two cohorts of infants. The first, screened from June 2008 through December 2009, included newborns who had saliva samples collected by swab and tested with both PCR and RC.
Due to a change of protocol, a second cohort of infants screened from January 2010 through November 2011 had saliva PCR testing, with RC performed on all samples that tested positive by PCR.
Infants who were positive for CMV by either screening were re-evaluated for confirmation, with testing of saliva and urine samples collected at enrollment. Infants confirmed to have congenital CMV infections were enrolled in follow-up to monitor their hearing outcomes.
Of the 35,334 infants screened in the first cohort, 161 tested positive for CMV and were enrolled for confirmation. Of this group, 152 had confirmed CMV, and 9 were confirmed to be CMV-negative.
Of the 152 confirmed CMV-positive, 147 were positive by both screening methods, 4 were PCR-positive but RC-negative, and 1 was PCR-negative but RC-positive,
In the second cohort, 37,250 infants were screened with PCR, and 123 were enrolled for confirmation. Of this group, 114 were confirmed to be CMV-positive, and 9 were confirmed to be CMV-negative. Of those confirmed positive, 105 were positive on both screening methods, and 9 were PCR-positive but RC-negative.
Of the 14 PCR/RC discordant samples, PCR detected CMV copies in varying amounts in 13, whereas RC detected cells in only 1 of the 14 (4 cells per slide).
Dr. Pinninti acknowledged a few study limitations, including the fact that infants with initially negative screens were not enrolled, and that samples were transported to a central lab, which could have degraded the quality of the cultured samples.
"This is really exciting," commented Dr. Morven S. Edwards, professor of pediatrics at Baylor College of Medicine, Houston, who comoderated the session in which the study was presented, but was not involved in the research.
The study was supported by the National Institute on Deafness and Other Communication Disorders. Dr. Pinninti and Dr. Edwards reported having no conflicts of interest.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: Of 123 infants enrolled for confirmation, 114 were confirmed to be CMV-positive, and 9 were confirmed to be CMV-negative. Of those confirmed positive, 105 were positive on both screening methods, and 9 were PCR-positive but RC-negative.
Data Source: This was a prospective multicenter study.
Disclosures: The study was supported by the National Institute on Deafness and Other Communication Disorders. Dr. Pinninti and Dr. Edwards reported having no conflicts of interest.
Gloves Not Enough for Infection Control in Preterm Newborns
BOSTON – Supplementing appropriate hand hygiene with nonsterile gloving can help keep late-onset infections at bay in preterm infants.
In a randomized, controlled trial reported at the annual meeting of the Pediatric Academic Societies, preterm infants in the neonatal intensive care unit of an academic hospital whose caregivers were directed to don nonsterile gloves after standard hand washing and prior to contact with the infants or with their central or peripheral lines were significantly less likely to develop bloodstream infections after 72 hours than those cared for by individuals who practiced appropriate hand hygiene only.
Specifically, the rate of gram-positive bloodstream infections among the 60 newborns randomized to gloved treatment was approximately 40% less than in the 60 newborns randomized to hand hygiene-only care, according to lead investigator David A. Kaufman of the University of Virginia in Charlottesville.
Further, "gloving after hand hygiene with all patient line contact was associated with a 60% decrease in central line associated blood stream infections and a 50% decrease in UTIs [urinary tract infections]," he said.
In previous studies, gloving plus hand hygiene has reduced the transmission of methicillin-resistant Staphylococcus aureus (MRSA) and other infections, "but we haven’t seen many randomized controlled trials in the NICU," said Dr. Kaufman. Such investigations are especially warranted in light of evidence that microorganisms often persist despite appropriate hand hygiene practices as well as the increased risk of infection and consequent morbidity and mortality among preterm infants weighing less than 1,000 g at birth.
For the current study, preterm newborns who weighed less than 1,000 g at birth or who were born at or before 28 weeks’ gestation were randomized to the gloving plus hand hygiene or hand hygiene-only group within 7 days after birth and continuing for 4 weeks or until intravenous access was no longer necessary, Dr. Kaufman said. Hand hygiene was defined as using alcohol hand rub or washing hands with antimicrobial soap. Outcome measures included the incidence of one or more episodes of blood stream infection, urinary tract infection, meningitis, and/or necrotizing enterocolitis after 72 hours.
The baseline characteristics of both groups of infants were similar, Dr. Kaufman reported, noting that gestational age and body weight of infants in the gloved group were 25.7 weeks and 790 g, respectively, compared with 25.9 weeks and 803 g in the hand hygiene-only group. While the rates for one or more episode of blood stream infection, UTI, meningitis, and necrotizing enterocolitis were similar between the groups, the odds ratio for gram-positive bloodstream infections in the gloving group was 0.42, and the odds ratio of possible central line-associated blood stream infection – defined as one or more positive culture and a central line in place – was 0.31 in the gloving group, he said.
The findings suggest that gloving is a simple, effective approach for preventing invasive infections in high-risk infants with lines in place, said Dr. Kaufmann. The resulting reduction in infection rates could improve outcomes while reducing hospital stays and overall health care costs in this population.
Dr. Kaufmann said he had no relevant financial conflicts to disclose.
BOSTON – Supplementing appropriate hand hygiene with nonsterile gloving can help keep late-onset infections at bay in preterm infants.
In a randomized, controlled trial reported at the annual meeting of the Pediatric Academic Societies, preterm infants in the neonatal intensive care unit of an academic hospital whose caregivers were directed to don nonsterile gloves after standard hand washing and prior to contact with the infants or with their central or peripheral lines were significantly less likely to develop bloodstream infections after 72 hours than those cared for by individuals who practiced appropriate hand hygiene only.
Specifically, the rate of gram-positive bloodstream infections among the 60 newborns randomized to gloved treatment was approximately 40% less than in the 60 newborns randomized to hand hygiene-only care, according to lead investigator David A. Kaufman of the University of Virginia in Charlottesville.
Further, "gloving after hand hygiene with all patient line contact was associated with a 60% decrease in central line associated blood stream infections and a 50% decrease in UTIs [urinary tract infections]," he said.
In previous studies, gloving plus hand hygiene has reduced the transmission of methicillin-resistant Staphylococcus aureus (MRSA) and other infections, "but we haven’t seen many randomized controlled trials in the NICU," said Dr. Kaufman. Such investigations are especially warranted in light of evidence that microorganisms often persist despite appropriate hand hygiene practices as well as the increased risk of infection and consequent morbidity and mortality among preterm infants weighing less than 1,000 g at birth.
For the current study, preterm newborns who weighed less than 1,000 g at birth or who were born at or before 28 weeks’ gestation were randomized to the gloving plus hand hygiene or hand hygiene-only group within 7 days after birth and continuing for 4 weeks or until intravenous access was no longer necessary, Dr. Kaufman said. Hand hygiene was defined as using alcohol hand rub or washing hands with antimicrobial soap. Outcome measures included the incidence of one or more episodes of blood stream infection, urinary tract infection, meningitis, and/or necrotizing enterocolitis after 72 hours.
The baseline characteristics of both groups of infants were similar, Dr. Kaufman reported, noting that gestational age and body weight of infants in the gloved group were 25.7 weeks and 790 g, respectively, compared with 25.9 weeks and 803 g in the hand hygiene-only group. While the rates for one or more episode of blood stream infection, UTI, meningitis, and necrotizing enterocolitis were similar between the groups, the odds ratio for gram-positive bloodstream infections in the gloving group was 0.42, and the odds ratio of possible central line-associated blood stream infection – defined as one or more positive culture and a central line in place – was 0.31 in the gloving group, he said.
The findings suggest that gloving is a simple, effective approach for preventing invasive infections in high-risk infants with lines in place, said Dr. Kaufmann. The resulting reduction in infection rates could improve outcomes while reducing hospital stays and overall health care costs in this population.
Dr. Kaufmann said he had no relevant financial conflicts to disclose.
BOSTON – Supplementing appropriate hand hygiene with nonsterile gloving can help keep late-onset infections at bay in preterm infants.
In a randomized, controlled trial reported at the annual meeting of the Pediatric Academic Societies, preterm infants in the neonatal intensive care unit of an academic hospital whose caregivers were directed to don nonsterile gloves after standard hand washing and prior to contact with the infants or with their central or peripheral lines were significantly less likely to develop bloodstream infections after 72 hours than those cared for by individuals who practiced appropriate hand hygiene only.
Specifically, the rate of gram-positive bloodstream infections among the 60 newborns randomized to gloved treatment was approximately 40% less than in the 60 newborns randomized to hand hygiene-only care, according to lead investigator David A. Kaufman of the University of Virginia in Charlottesville.
Further, "gloving after hand hygiene with all patient line contact was associated with a 60% decrease in central line associated blood stream infections and a 50% decrease in UTIs [urinary tract infections]," he said.
In previous studies, gloving plus hand hygiene has reduced the transmission of methicillin-resistant Staphylococcus aureus (MRSA) and other infections, "but we haven’t seen many randomized controlled trials in the NICU," said Dr. Kaufman. Such investigations are especially warranted in light of evidence that microorganisms often persist despite appropriate hand hygiene practices as well as the increased risk of infection and consequent morbidity and mortality among preterm infants weighing less than 1,000 g at birth.
For the current study, preterm newborns who weighed less than 1,000 g at birth or who were born at or before 28 weeks’ gestation were randomized to the gloving plus hand hygiene or hand hygiene-only group within 7 days after birth and continuing for 4 weeks or until intravenous access was no longer necessary, Dr. Kaufman said. Hand hygiene was defined as using alcohol hand rub or washing hands with antimicrobial soap. Outcome measures included the incidence of one or more episodes of blood stream infection, urinary tract infection, meningitis, and/or necrotizing enterocolitis after 72 hours.
The baseline characteristics of both groups of infants were similar, Dr. Kaufman reported, noting that gestational age and body weight of infants in the gloved group were 25.7 weeks and 790 g, respectively, compared with 25.9 weeks and 803 g in the hand hygiene-only group. While the rates for one or more episode of blood stream infection, UTI, meningitis, and necrotizing enterocolitis were similar between the groups, the odds ratio for gram-positive bloodstream infections in the gloving group was 0.42, and the odds ratio of possible central line-associated blood stream infection – defined as one or more positive culture and a central line in place – was 0.31 in the gloving group, he said.
The findings suggest that gloving is a simple, effective approach for preventing invasive infections in high-risk infants with lines in place, said Dr. Kaufmann. The resulting reduction in infection rates could improve outcomes while reducing hospital stays and overall health care costs in this population.
Dr. Kaufmann said he had no relevant financial conflicts to disclose.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: Gram-positive bloodstream infections were more than 40% lower in preterm infants whose NICU caregivers donned nonsterile gloves after hand hygiene relative to appropriate hand hygiene alone prior to patient and peripheral and central line contact.
Data Source: This was a randomized controlled trial of 120 preterm infants.
Disclosures: Dr. Kaufmann said he had no relevant financial conflicts to disclose.