User login
Quick medication, better communication linked to less violence at inpatient psych unit
SAN FRANCISCO – Physically violent events at an inpatient psychiatric unit in Pennsylvania dropped by 59.8% in the months after it implemented a plan to administer antipsychotic medications to patients more quickly – both in the emergency department and in the unit – and improve handoffs between providers and nurses, researchers reported.
“We were able to significantly reduce violence,” said Michael Chen, MD, Lehigh Valley Health Network psychiatry resident and lead author of an abstract presented at the annual meeting of the American Psychiatric Association. “Furthermore, the interventions were effective in reducing episodes of violence rather than redirecting it. And the overall feeling of safety on the inpatient psychiatric unit improved.”
Violence is common in psychiatric units, although it’s not clear how often it occurs. “The data has shown that patients with a psychotic disorder such as schizophrenia or a mood disorder with psychotic features such as bipolar disorder tend to account for most of the episodes of violence on the unit,” Dr. Chen said in an interview. “This inevitably results in a higher risk for violence on inpatient psychiatric units as a large portion of patients admitted to inpatient psychiatric units have these diagnoses.”
Enlisting the pharmacy department
For the new study, investigators tracked episodes of violence – including verbal attacks – at an Allentown, Penn.–area inpatient psychiatric unit from December 2021 to September 2022. According to Dr. Chen, unit leaders implemented the new plan in May 2022 in the wake of higher levels of violence during the COVID-19 pandemic and the concurrent staff shortages.
Clinic leaders sought to identify potentially aggressive patients in the emergency department and treat them with antipsychotics prior to admission to the psychiatric unit, ensure that the pharmacy provides access to as-needed or standing medications, and develop “standardized huddles to ensure proper handoffs between providers and nurses.”
Medical staff relied on the Dynamic Appraisal of Situational Aggression scale, risk factors, and clinical judgment to determine which patients had the potential to be violent, Dr. Chen said.
As for treatment, first-line antipsychotics are typically given orally, but they can be injected if patients must be treated over their objections, he said. “We would only consider starting standing medications against objections in patients who are involuntarily committed.”
During the 5 months before the intervention was implemented versus the following 5 months, the average monthly number of physically violent events in the psychiatric unit fell from 12.4 to 4.8 (–61.1%, P = .04), and verbal threats dipped from 7.2 to 4 (–44.4%, P = .15). The total average number of violent events per month, including violence against property, fell from an average of 25.4 to 10.2 (–59.8%, P = .03).
The total patient population didn’t vary significantly over time, Dr. Chen said. “Thus, the decrease in violence was not correlated with a decrease in patient load.”
While “there were concerns that there would just be higher episodes of violence in the ED while psychiatry patients awaited placement,” Dr. Chen said, the numbers actually showed reductions in violence in that setting. The average number of physically violent events per month in the ED fell from 49.6 to 39.4 (–20.6%, P = .03). Verbal threats dropped from 38 to 34.6 (–8.9%, P = .5) and overall violent events dipped from 87.6 to 74 (–15.6%, P = .08).
Why did the interventions seem to work? “Standing doses as well as as-needed medications started for psychiatric patients in the emergency department have been crucial to prevent delay of care,” Dr. Chen said. Enlisting the pharmacy department “helped ensure all patients had appropriate as-needed medications to prevent them from decompensating on the units,” he added, and “involvement of nursing and ancillary staff in high-risk rounds allowed the treatment team to rapidly anticipate and address concerns.”
The study authors also reported that nursing staff felt safer. Scores on a perception-of-safety scale – with 1 most unsafe and 7 most safe – improved from 3.3 to 4.2 (+27%, P < .01).
Dr. Chen said there was a “minimal” increase in cost to implement the intervention, although coordination is necessary. “The emergency department and psychiatry department have to work together to initiate treatment in the ED while awaiting beds,” he said. “The treatment team needs to communicate concerns during rounds. The pharmacist and psychiatrist need to work together to ensure that proper as-needed medications are available.”
‘Good clinical practice’
In an interview, psychiatrist Mark J. Russ, MD, of NewYork-Presbyterian/Westchester Behavioral Health and Weill Cornell Medical College, said violent incidents in inpatient psychiatric units are influenced by many factors, such as history of violence, substance use, history of trauma, psychosis/paranoia, and medical problems.
The units themselves can contribute to the risk of violence through power struggles and lack of attention paid to respect and dignity, he said. “Attention to these issues is important in reducing violence,” he noted. “Generalized training for staff in de-escalation techniques and trauma-informed care is imperative. There may be value in developing specialized psychiatric ICUs where staff are meticulously trained in these and other approaches.”
The new study, Dr. Russ said, suggests that “early identification of patients at risk of engaging in violent behavior on the inpatient unit, pharmacologic treatment, and good communication helps reduce violence.” The findings, he added, suggest that “interventions known to constitute good clinical practice are indeed helpful.”
However, he cautioned that “treating all at-risk patients with antipsychotics, regardless of their psychiatric diagnosis, might well be considered chemical restraint, depending on [the] circumstances.”
There was no study funding. The study authors and Dr. Russ have no disclosures.
SAN FRANCISCO – Physically violent events at an inpatient psychiatric unit in Pennsylvania dropped by 59.8% in the months after it implemented a plan to administer antipsychotic medications to patients more quickly – both in the emergency department and in the unit – and improve handoffs between providers and nurses, researchers reported.
“We were able to significantly reduce violence,” said Michael Chen, MD, Lehigh Valley Health Network psychiatry resident and lead author of an abstract presented at the annual meeting of the American Psychiatric Association. “Furthermore, the interventions were effective in reducing episodes of violence rather than redirecting it. And the overall feeling of safety on the inpatient psychiatric unit improved.”
Violence is common in psychiatric units, although it’s not clear how often it occurs. “The data has shown that patients with a psychotic disorder such as schizophrenia or a mood disorder with psychotic features such as bipolar disorder tend to account for most of the episodes of violence on the unit,” Dr. Chen said in an interview. “This inevitably results in a higher risk for violence on inpatient psychiatric units as a large portion of patients admitted to inpatient psychiatric units have these diagnoses.”
Enlisting the pharmacy department
For the new study, investigators tracked episodes of violence – including verbal attacks – at an Allentown, Penn.–area inpatient psychiatric unit from December 2021 to September 2022. According to Dr. Chen, unit leaders implemented the new plan in May 2022 in the wake of higher levels of violence during the COVID-19 pandemic and the concurrent staff shortages.
Clinic leaders sought to identify potentially aggressive patients in the emergency department and treat them with antipsychotics prior to admission to the psychiatric unit, ensure that the pharmacy provides access to as-needed or standing medications, and develop “standardized huddles to ensure proper handoffs between providers and nurses.”
Medical staff relied on the Dynamic Appraisal of Situational Aggression scale, risk factors, and clinical judgment to determine which patients had the potential to be violent, Dr. Chen said.
As for treatment, first-line antipsychotics are typically given orally, but they can be injected if patients must be treated over their objections, he said. “We would only consider starting standing medications against objections in patients who are involuntarily committed.”
During the 5 months before the intervention was implemented versus the following 5 months, the average monthly number of physically violent events in the psychiatric unit fell from 12.4 to 4.8 (–61.1%, P = .04), and verbal threats dipped from 7.2 to 4 (–44.4%, P = .15). The total average number of violent events per month, including violence against property, fell from an average of 25.4 to 10.2 (–59.8%, P = .03).
The total patient population didn’t vary significantly over time, Dr. Chen said. “Thus, the decrease in violence was not correlated with a decrease in patient load.”
While “there were concerns that there would just be higher episodes of violence in the ED while psychiatry patients awaited placement,” Dr. Chen said, the numbers actually showed reductions in violence in that setting. The average number of physically violent events per month in the ED fell from 49.6 to 39.4 (–20.6%, P = .03). Verbal threats dropped from 38 to 34.6 (–8.9%, P = .5) and overall violent events dipped from 87.6 to 74 (–15.6%, P = .08).
Why did the interventions seem to work? “Standing doses as well as as-needed medications started for psychiatric patients in the emergency department have been crucial to prevent delay of care,” Dr. Chen said. Enlisting the pharmacy department “helped ensure all patients had appropriate as-needed medications to prevent them from decompensating on the units,” he added, and “involvement of nursing and ancillary staff in high-risk rounds allowed the treatment team to rapidly anticipate and address concerns.”
The study authors also reported that nursing staff felt safer. Scores on a perception-of-safety scale – with 1 most unsafe and 7 most safe – improved from 3.3 to 4.2 (+27%, P < .01).
Dr. Chen said there was a “minimal” increase in cost to implement the intervention, although coordination is necessary. “The emergency department and psychiatry department have to work together to initiate treatment in the ED while awaiting beds,” he said. “The treatment team needs to communicate concerns during rounds. The pharmacist and psychiatrist need to work together to ensure that proper as-needed medications are available.”
‘Good clinical practice’
In an interview, psychiatrist Mark J. Russ, MD, of NewYork-Presbyterian/Westchester Behavioral Health and Weill Cornell Medical College, said violent incidents in inpatient psychiatric units are influenced by many factors, such as history of violence, substance use, history of trauma, psychosis/paranoia, and medical problems.
The units themselves can contribute to the risk of violence through power struggles and lack of attention paid to respect and dignity, he said. “Attention to these issues is important in reducing violence,” he noted. “Generalized training for staff in de-escalation techniques and trauma-informed care is imperative. There may be value in developing specialized psychiatric ICUs where staff are meticulously trained in these and other approaches.”
The new study, Dr. Russ said, suggests that “early identification of patients at risk of engaging in violent behavior on the inpatient unit, pharmacologic treatment, and good communication helps reduce violence.” The findings, he added, suggest that “interventions known to constitute good clinical practice are indeed helpful.”
However, he cautioned that “treating all at-risk patients with antipsychotics, regardless of their psychiatric diagnosis, might well be considered chemical restraint, depending on [the] circumstances.”
There was no study funding. The study authors and Dr. Russ have no disclosures.
SAN FRANCISCO – Physically violent events at an inpatient psychiatric unit in Pennsylvania dropped by 59.8% in the months after it implemented a plan to administer antipsychotic medications to patients more quickly – both in the emergency department and in the unit – and improve handoffs between providers and nurses, researchers reported.
“We were able to significantly reduce violence,” said Michael Chen, MD, Lehigh Valley Health Network psychiatry resident and lead author of an abstract presented at the annual meeting of the American Psychiatric Association. “Furthermore, the interventions were effective in reducing episodes of violence rather than redirecting it. And the overall feeling of safety on the inpatient psychiatric unit improved.”
Violence is common in psychiatric units, although it’s not clear how often it occurs. “The data has shown that patients with a psychotic disorder such as schizophrenia or a mood disorder with psychotic features such as bipolar disorder tend to account for most of the episodes of violence on the unit,” Dr. Chen said in an interview. “This inevitably results in a higher risk for violence on inpatient psychiatric units as a large portion of patients admitted to inpatient psychiatric units have these diagnoses.”
Enlisting the pharmacy department
For the new study, investigators tracked episodes of violence – including verbal attacks – at an Allentown, Penn.–area inpatient psychiatric unit from December 2021 to September 2022. According to Dr. Chen, unit leaders implemented the new plan in May 2022 in the wake of higher levels of violence during the COVID-19 pandemic and the concurrent staff shortages.
Clinic leaders sought to identify potentially aggressive patients in the emergency department and treat them with antipsychotics prior to admission to the psychiatric unit, ensure that the pharmacy provides access to as-needed or standing medications, and develop “standardized huddles to ensure proper handoffs between providers and nurses.”
Medical staff relied on the Dynamic Appraisal of Situational Aggression scale, risk factors, and clinical judgment to determine which patients had the potential to be violent, Dr. Chen said.
As for treatment, first-line antipsychotics are typically given orally, but they can be injected if patients must be treated over their objections, he said. “We would only consider starting standing medications against objections in patients who are involuntarily committed.”
During the 5 months before the intervention was implemented versus the following 5 months, the average monthly number of physically violent events in the psychiatric unit fell from 12.4 to 4.8 (–61.1%, P = .04), and verbal threats dipped from 7.2 to 4 (–44.4%, P = .15). The total average number of violent events per month, including violence against property, fell from an average of 25.4 to 10.2 (–59.8%, P = .03).
The total patient population didn’t vary significantly over time, Dr. Chen said. “Thus, the decrease in violence was not correlated with a decrease in patient load.”
While “there were concerns that there would just be higher episodes of violence in the ED while psychiatry patients awaited placement,” Dr. Chen said, the numbers actually showed reductions in violence in that setting. The average number of physically violent events per month in the ED fell from 49.6 to 39.4 (–20.6%, P = .03). Verbal threats dropped from 38 to 34.6 (–8.9%, P = .5) and overall violent events dipped from 87.6 to 74 (–15.6%, P = .08).
Why did the interventions seem to work? “Standing doses as well as as-needed medications started for psychiatric patients in the emergency department have been crucial to prevent delay of care,” Dr. Chen said. Enlisting the pharmacy department “helped ensure all patients had appropriate as-needed medications to prevent them from decompensating on the units,” he added, and “involvement of nursing and ancillary staff in high-risk rounds allowed the treatment team to rapidly anticipate and address concerns.”
The study authors also reported that nursing staff felt safer. Scores on a perception-of-safety scale – with 1 most unsafe and 7 most safe – improved from 3.3 to 4.2 (+27%, P < .01).
Dr. Chen said there was a “minimal” increase in cost to implement the intervention, although coordination is necessary. “The emergency department and psychiatry department have to work together to initiate treatment in the ED while awaiting beds,” he said. “The treatment team needs to communicate concerns during rounds. The pharmacist and psychiatrist need to work together to ensure that proper as-needed medications are available.”
‘Good clinical practice’
In an interview, psychiatrist Mark J. Russ, MD, of NewYork-Presbyterian/Westchester Behavioral Health and Weill Cornell Medical College, said violent incidents in inpatient psychiatric units are influenced by many factors, such as history of violence, substance use, history of trauma, psychosis/paranoia, and medical problems.
The units themselves can contribute to the risk of violence through power struggles and lack of attention paid to respect and dignity, he said. “Attention to these issues is important in reducing violence,” he noted. “Generalized training for staff in de-escalation techniques and trauma-informed care is imperative. There may be value in developing specialized psychiatric ICUs where staff are meticulously trained in these and other approaches.”
The new study, Dr. Russ said, suggests that “early identification of patients at risk of engaging in violent behavior on the inpatient unit, pharmacologic treatment, and good communication helps reduce violence.” The findings, he added, suggest that “interventions known to constitute good clinical practice are indeed helpful.”
However, he cautioned that “treating all at-risk patients with antipsychotics, regardless of their psychiatric diagnosis, might well be considered chemical restraint, depending on [the] circumstances.”
There was no study funding. The study authors and Dr. Russ have no disclosures.
AT APA 2023
Harmful emotional hit of antidepressants underappreciated
SAN FRANCISCO – , new research shows.
Emotional blunting can be described as feeling emotionally flat and incapable of finding pleasure. The patient may feel less sadness, guilt, or hopelessness, but that may come at the cost of feeling less joy, surprise, and happiness. Some people with SSRI-induced blunting even report caring less about important relationships.
It’s an issue that needs greater attention, study investigator Mujeeb U. Shad, MD, with Valley Health Services and University of Nevada, Las Vegas, said in an interview.
“Patients may come to the clinic and report feeling emotionally and cognitively flat and not be taken seriously by their provider, but they are genuinely reporting something that is happening to them and decreasing their quality of life,” Dr. Shad explained.
The study was presented at the annual meeting of the American Psychiatric Association.
Something ‘missing’
Dr. Shad said that the genesis for the study came from a resident who noticed that many patients receiving SSRIs reported feeling better and not as bothered by the depression, yet, at the same time, they felt something was “missing. Their families would say, ‘You’re better but you’re not the same person.’ ”
To investigate further, the researchers did a “scoping review” of 25 original studies that assessed antidepressant-related emotional blunting. Until now, there hasn’t been a systematic review of this issue, Dr. Shad said.
Ten of the studies looked at the role of SSRIs in emotional blunting, whereas the other 15 looked at serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and second-generation antipsychotic medications.
The results of the review show that emotional blunting is a significant patient-reported concern. It often presents as a subjective complaint of changed personality, feeling a lesser intensity of overall emotions, and the manifestation of not being oneself often attributed to antidepressant use, the researchers found. Emotional blunting was more commonly associated with SSRIs than with the other medications in the studies.
Common clinical strategies to manage antidepressant-induced emotional blunting reported in the literature include dose reduction or switching to a different antidepressant class; however, the literature did not make the distinction between emotional blunting as a primary symptom of depression or an adverse effect of antidepressants.
Dr. Shad said that there is a need to develop valid and reliable measures to assess emotional blunting related to antidepressants.
He noted that optimal patient care should include pre- and posttreatment assessment of emotional blunting. One useful tool is the Oxford Questionnaire on the Emotional Side-Effects of Antidepressants.
Can’t get to the top
Jacob Cross, MD, who wasn’t involved in the study, said that he has seen the impact of antidepressant-related emotional blunting first-hand.
“I’ve had multiple patients report emotional blunting on antidepressant therapy,” Dr. Cross, with the department of psychiatry, Rush Medical College, Chicago, said.
“These patients feel like their emotions are not as high and not as low; so they experience directional improvement, but they’re still not feeling like they can get that top peak emotion. It’s kind of similar to anhedonia. They’re just feeling like a little cut off, like they’re climbing a cliff and just can’t get to that top,” Dr. Cross said.
For a patient with emotional blunting, Dr. Cross said he might “switch to an antidepressant that’s more stimulating like an SNRI from an SSRI. You could also lower the dose and see if that helps, but I usually change the drug class.”
The study had no specific funding. Dr. Shad and Dr. Cross have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – , new research shows.
Emotional blunting can be described as feeling emotionally flat and incapable of finding pleasure. The patient may feel less sadness, guilt, or hopelessness, but that may come at the cost of feeling less joy, surprise, and happiness. Some people with SSRI-induced blunting even report caring less about important relationships.
It’s an issue that needs greater attention, study investigator Mujeeb U. Shad, MD, with Valley Health Services and University of Nevada, Las Vegas, said in an interview.
“Patients may come to the clinic and report feeling emotionally and cognitively flat and not be taken seriously by their provider, but they are genuinely reporting something that is happening to them and decreasing their quality of life,” Dr. Shad explained.
The study was presented at the annual meeting of the American Psychiatric Association.
Something ‘missing’
Dr. Shad said that the genesis for the study came from a resident who noticed that many patients receiving SSRIs reported feeling better and not as bothered by the depression, yet, at the same time, they felt something was “missing. Their families would say, ‘You’re better but you’re not the same person.’ ”
To investigate further, the researchers did a “scoping review” of 25 original studies that assessed antidepressant-related emotional blunting. Until now, there hasn’t been a systematic review of this issue, Dr. Shad said.
Ten of the studies looked at the role of SSRIs in emotional blunting, whereas the other 15 looked at serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and second-generation antipsychotic medications.
The results of the review show that emotional blunting is a significant patient-reported concern. It often presents as a subjective complaint of changed personality, feeling a lesser intensity of overall emotions, and the manifestation of not being oneself often attributed to antidepressant use, the researchers found. Emotional blunting was more commonly associated with SSRIs than with the other medications in the studies.
Common clinical strategies to manage antidepressant-induced emotional blunting reported in the literature include dose reduction or switching to a different antidepressant class; however, the literature did not make the distinction between emotional blunting as a primary symptom of depression or an adverse effect of antidepressants.
Dr. Shad said that there is a need to develop valid and reliable measures to assess emotional blunting related to antidepressants.
He noted that optimal patient care should include pre- and posttreatment assessment of emotional blunting. One useful tool is the Oxford Questionnaire on the Emotional Side-Effects of Antidepressants.
Can’t get to the top
Jacob Cross, MD, who wasn’t involved in the study, said that he has seen the impact of antidepressant-related emotional blunting first-hand.
“I’ve had multiple patients report emotional blunting on antidepressant therapy,” Dr. Cross, with the department of psychiatry, Rush Medical College, Chicago, said.
“These patients feel like their emotions are not as high and not as low; so they experience directional improvement, but they’re still not feeling like they can get that top peak emotion. It’s kind of similar to anhedonia. They’re just feeling like a little cut off, like they’re climbing a cliff and just can’t get to that top,” Dr. Cross said.
For a patient with emotional blunting, Dr. Cross said he might “switch to an antidepressant that’s more stimulating like an SNRI from an SSRI. You could also lower the dose and see if that helps, but I usually change the drug class.”
The study had no specific funding. Dr. Shad and Dr. Cross have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – , new research shows.
Emotional blunting can be described as feeling emotionally flat and incapable of finding pleasure. The patient may feel less sadness, guilt, or hopelessness, but that may come at the cost of feeling less joy, surprise, and happiness. Some people with SSRI-induced blunting even report caring less about important relationships.
It’s an issue that needs greater attention, study investigator Mujeeb U. Shad, MD, with Valley Health Services and University of Nevada, Las Vegas, said in an interview.
“Patients may come to the clinic and report feeling emotionally and cognitively flat and not be taken seriously by their provider, but they are genuinely reporting something that is happening to them and decreasing their quality of life,” Dr. Shad explained.
The study was presented at the annual meeting of the American Psychiatric Association.
Something ‘missing’
Dr. Shad said that the genesis for the study came from a resident who noticed that many patients receiving SSRIs reported feeling better and not as bothered by the depression, yet, at the same time, they felt something was “missing. Their families would say, ‘You’re better but you’re not the same person.’ ”
To investigate further, the researchers did a “scoping review” of 25 original studies that assessed antidepressant-related emotional blunting. Until now, there hasn’t been a systematic review of this issue, Dr. Shad said.
Ten of the studies looked at the role of SSRIs in emotional blunting, whereas the other 15 looked at serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and second-generation antipsychotic medications.
The results of the review show that emotional blunting is a significant patient-reported concern. It often presents as a subjective complaint of changed personality, feeling a lesser intensity of overall emotions, and the manifestation of not being oneself often attributed to antidepressant use, the researchers found. Emotional blunting was more commonly associated with SSRIs than with the other medications in the studies.
Common clinical strategies to manage antidepressant-induced emotional blunting reported in the literature include dose reduction or switching to a different antidepressant class; however, the literature did not make the distinction between emotional blunting as a primary symptom of depression or an adverse effect of antidepressants.
Dr. Shad said that there is a need to develop valid and reliable measures to assess emotional blunting related to antidepressants.
He noted that optimal patient care should include pre- and posttreatment assessment of emotional blunting. One useful tool is the Oxford Questionnaire on the Emotional Side-Effects of Antidepressants.
Can’t get to the top
Jacob Cross, MD, who wasn’t involved in the study, said that he has seen the impact of antidepressant-related emotional blunting first-hand.
“I’ve had multiple patients report emotional blunting on antidepressant therapy,” Dr. Cross, with the department of psychiatry, Rush Medical College, Chicago, said.
“These patients feel like their emotions are not as high and not as low; so they experience directional improvement, but they’re still not feeling like they can get that top peak emotion. It’s kind of similar to anhedonia. They’re just feeling like a little cut off, like they’re climbing a cliff and just can’t get to that top,” Dr. Cross said.
For a patient with emotional blunting, Dr. Cross said he might “switch to an antidepressant that’s more stimulating like an SNRI from an SSRI. You could also lower the dose and see if that helps, but I usually change the drug class.”
The study had no specific funding. Dr. Shad and Dr. Cross have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
AT APA 2023
Eating disorder apps fall short when it comes to privacy
SAN FRANCISCO –
Federal laws require those handling sensitive health information to have policies and security safeguards in place to protect such information, whether it’s stored on paper or electronically.
“As it stands right now, there’s not enough evidence to support using these apps as an adjunct to clinical care,” study author Theodora O’Leary, a 4th-year medical student at Tufts University, Boston, said in an interview. “We need more research on the efficacy of these apps because right now not enough of them meet HIPAA [standards] and don’t have privacy and security measures.”
The findings were presented at the annual meeting of the American Psychiatric Association.
Eating disorders (EDs) are a common mental health condition affecting almost 1 in 10 Americans over their lifetime. Yet only about a third of patients with an eating disorder receive adequate treatment.
The pandemic saw a rise in eating disorders and in the use of mental health apps “to kind of fill the gap because people couldn’t be seen in person,” said Ms. O’Leary.
Inexpensive and accessible
Smartphone apps have a lot of advantages for patients with an ED. For one thing, they’re relatively inexpensive and accessible; most Americans already own one or more devices on which these apps can be used.
They’re also a feasible means of delivering psychological interventions, which are often recommended for EDs. Among these interventions, cognitive-behavioral therapy (CBT) has the largest evidence base for this condition.
Also, as many individuals with an ED may be reluctant to seek treatment because of stigma and shame, the anonymity afforded by an app could increase access to the help they seek.
But Ms. O’Leary warned the Food and Drug Administration does not regulate these apps, and people are sharing their personal health information on them.
The researchers conducted a review of commercially available eating disorder apps by searching the Apple and Google play stores using key phrases such as “eating disorder,” “anorexia,” and “binge eating disorder.”
They found 16 relevant apps that they added to the publicly available apps already in a database at Tufts, for a total of about 36 that were evaluated in the study (the number fluctuates as apps are deleted.)
They then reviewed the apps using the 105 questions based on the APA’s app evaluation model, which covers categories such as efficacy, privacy, accessibility, and clinical applicability. And they used filters to group apps by characteristics such as function, cost, and features.
The vast majority were self-help apps, which include things like journaling, meditation, and information on CBT. Others were reference apps that provide related definitions and sometimes include surveys to determine, for example, if the user has an eating disorder.
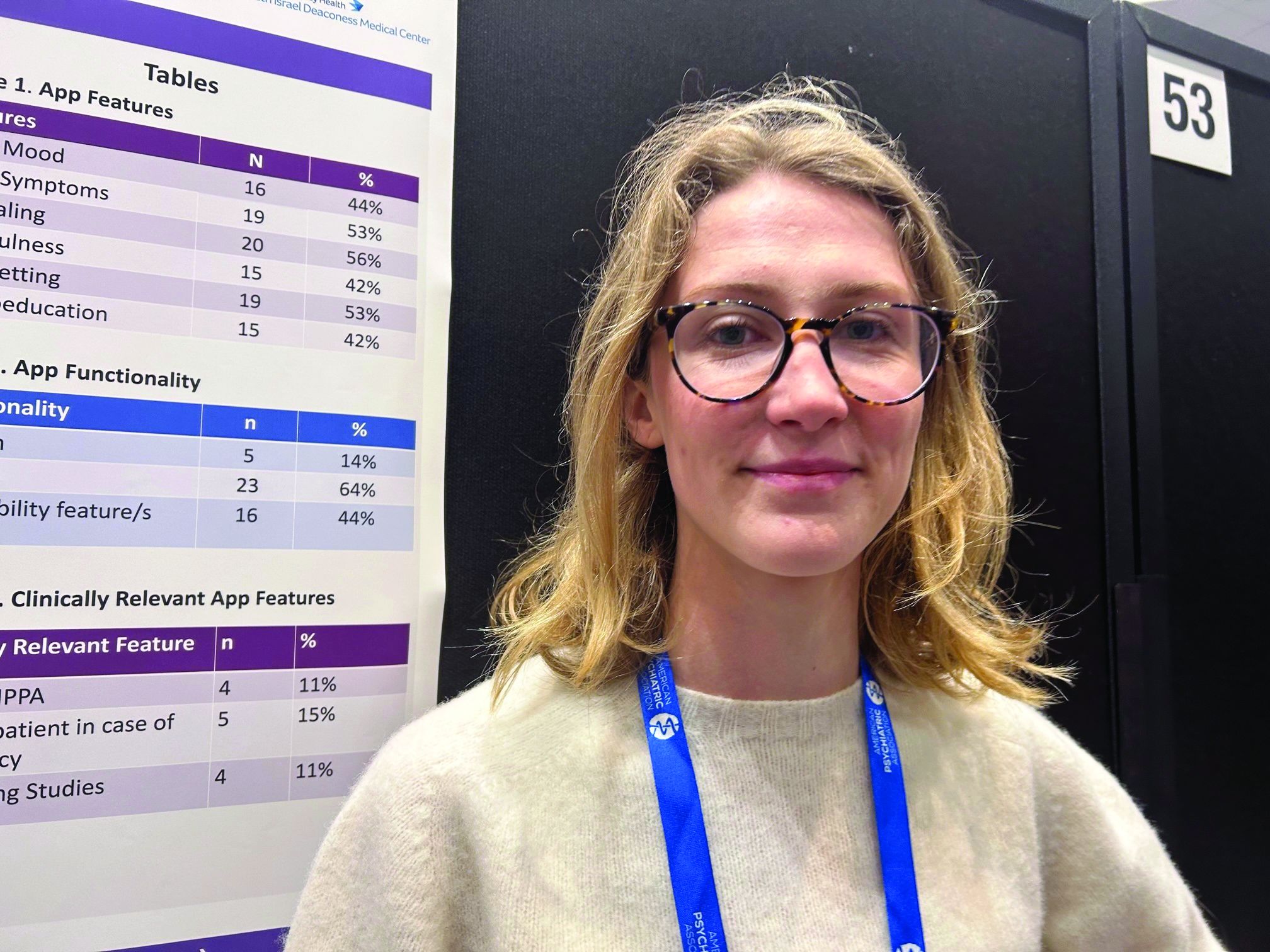
About 44% of the apps track mood, and 53% track symptoms. Some 56% include journaling, 42% mindfulness, 53% goal setting, and 42% psychoeducation.
Hybrid care
Only 5% of apps allow for “hybrid” care. This, explained Ms. O’Leary, is when clinicians use their own app to access patients’ apps, allowing them to track food restrictions and therapies, and make comments.
“The hybrid is viewed as the best form of app”, she said. “It’s almost like an adjunct to clinical care.”
Hybrid apps also tend to have patient safety features, she added. And these apps meet HIPAA standards, which only 11% of the apps in the study did.
Only 15% of apps advised patients to take steps in case of an emergency, and 11% had supporting studies. And where there was supporting research, much of it was funded by the app creators, said Ms. O’Leary.
For example, an app provided by Noom (the weight loss program that promises to help change habits and mindsets around food) “has a bunch of feasibility studies but they’re all funded by Noom”, which can introduce bias, she explained.
None of the apps were created by an accredited health care institution, she noted. “And I think only one app out of all the eating disorder apps we looked at was from a nonprofit.”
About 17% of the apps offer help with a “coach” or “expert”. However, these apps often fail to disclose the definition of a coach or state they’re not a replacement for medical care.
Coaching apps more expensive
Additionally, these coaching apps are often some of the most expensive, said Ms. O’Leary.
Daniel E. Gih, MD, associate professor at the University of Nebraska Medical Center, Omaha, helped start an eating disorders program at the University of Michigan and continues to treat patients with eating disorders. He said the increase in the use of eating disorder apps isn’t surprising as the incidence of these disorders increased in the wake of pandemic restrictions, especially among young people.
“Patients are likely doing more research on their medical conditions and trying to crowdsource information or self-treat,” Dr. Gih said.
It’s unclear whether “shame or just the general lack of specialized eating disorder professionals,” including physicians, is driving some of the interest in these apps, he added.
Dr. Gih stressed eating disorder apps should not only include screening for suicidality, but also explicitly tell patients to seek immediate attention if they show certain signs – for example, fainting, chest pain, or blood in emesis.
“The apps may be giving patients false hope or delaying medical care,” he said. “Apps are likely not sufficient enough to replace a multidisciplinary team with experience and expertise in eating disorders.”
Ms. O’Leary and Dr. Gih report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO –
Federal laws require those handling sensitive health information to have policies and security safeguards in place to protect such information, whether it’s stored on paper or electronically.
“As it stands right now, there’s not enough evidence to support using these apps as an adjunct to clinical care,” study author Theodora O’Leary, a 4th-year medical student at Tufts University, Boston, said in an interview. “We need more research on the efficacy of these apps because right now not enough of them meet HIPAA [standards] and don’t have privacy and security measures.”
The findings were presented at the annual meeting of the American Psychiatric Association.
Eating disorders (EDs) are a common mental health condition affecting almost 1 in 10 Americans over their lifetime. Yet only about a third of patients with an eating disorder receive adequate treatment.
The pandemic saw a rise in eating disorders and in the use of mental health apps “to kind of fill the gap because people couldn’t be seen in person,” said Ms. O’Leary.
Inexpensive and accessible
Smartphone apps have a lot of advantages for patients with an ED. For one thing, they’re relatively inexpensive and accessible; most Americans already own one or more devices on which these apps can be used.
They’re also a feasible means of delivering psychological interventions, which are often recommended for EDs. Among these interventions, cognitive-behavioral therapy (CBT) has the largest evidence base for this condition.
Also, as many individuals with an ED may be reluctant to seek treatment because of stigma and shame, the anonymity afforded by an app could increase access to the help they seek.
But Ms. O’Leary warned the Food and Drug Administration does not regulate these apps, and people are sharing their personal health information on them.
The researchers conducted a review of commercially available eating disorder apps by searching the Apple and Google play stores using key phrases such as “eating disorder,” “anorexia,” and “binge eating disorder.”
They found 16 relevant apps that they added to the publicly available apps already in a database at Tufts, for a total of about 36 that were evaluated in the study (the number fluctuates as apps are deleted.)
They then reviewed the apps using the 105 questions based on the APA’s app evaluation model, which covers categories such as efficacy, privacy, accessibility, and clinical applicability. And they used filters to group apps by characteristics such as function, cost, and features.
The vast majority were self-help apps, which include things like journaling, meditation, and information on CBT. Others were reference apps that provide related definitions and sometimes include surveys to determine, for example, if the user has an eating disorder.
About 44% of the apps track mood, and 53% track symptoms. Some 56% include journaling, 42% mindfulness, 53% goal setting, and 42% psychoeducation.
Hybrid care
Only 5% of apps allow for “hybrid” care. This, explained Ms. O’Leary, is when clinicians use their own app to access patients’ apps, allowing them to track food restrictions and therapies, and make comments.
“The hybrid is viewed as the best form of app”, she said. “It’s almost like an adjunct to clinical care.”
Hybrid apps also tend to have patient safety features, she added. And these apps meet HIPAA standards, which only 11% of the apps in the study did.
Only 15% of apps advised patients to take steps in case of an emergency, and 11% had supporting studies. And where there was supporting research, much of it was funded by the app creators, said Ms. O’Leary.
For example, an app provided by Noom (the weight loss program that promises to help change habits and mindsets around food) “has a bunch of feasibility studies but they’re all funded by Noom”, which can introduce bias, she explained.
None of the apps were created by an accredited health care institution, she noted. “And I think only one app out of all the eating disorder apps we looked at was from a nonprofit.”
About 17% of the apps offer help with a “coach” or “expert”. However, these apps often fail to disclose the definition of a coach or state they’re not a replacement for medical care.
Coaching apps more expensive
Additionally, these coaching apps are often some of the most expensive, said Ms. O’Leary.
Daniel E. Gih, MD, associate professor at the University of Nebraska Medical Center, Omaha, helped start an eating disorders program at the University of Michigan and continues to treat patients with eating disorders. He said the increase in the use of eating disorder apps isn’t surprising as the incidence of these disorders increased in the wake of pandemic restrictions, especially among young people.
“Patients are likely doing more research on their medical conditions and trying to crowdsource information or self-treat,” Dr. Gih said.
It’s unclear whether “shame or just the general lack of specialized eating disorder professionals,” including physicians, is driving some of the interest in these apps, he added.
Dr. Gih stressed eating disorder apps should not only include screening for suicidality, but also explicitly tell patients to seek immediate attention if they show certain signs – for example, fainting, chest pain, or blood in emesis.
“The apps may be giving patients false hope or delaying medical care,” he said. “Apps are likely not sufficient enough to replace a multidisciplinary team with experience and expertise in eating disorders.”
Ms. O’Leary and Dr. Gih report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO –
Federal laws require those handling sensitive health information to have policies and security safeguards in place to protect such information, whether it’s stored on paper or electronically.
“As it stands right now, there’s not enough evidence to support using these apps as an adjunct to clinical care,” study author Theodora O’Leary, a 4th-year medical student at Tufts University, Boston, said in an interview. “We need more research on the efficacy of these apps because right now not enough of them meet HIPAA [standards] and don’t have privacy and security measures.”
The findings were presented at the annual meeting of the American Psychiatric Association.
Eating disorders (EDs) are a common mental health condition affecting almost 1 in 10 Americans over their lifetime. Yet only about a third of patients with an eating disorder receive adequate treatment.
The pandemic saw a rise in eating disorders and in the use of mental health apps “to kind of fill the gap because people couldn’t be seen in person,” said Ms. O’Leary.
Inexpensive and accessible
Smartphone apps have a lot of advantages for patients with an ED. For one thing, they’re relatively inexpensive and accessible; most Americans already own one or more devices on which these apps can be used.
They’re also a feasible means of delivering psychological interventions, which are often recommended for EDs. Among these interventions, cognitive-behavioral therapy (CBT) has the largest evidence base for this condition.
Also, as many individuals with an ED may be reluctant to seek treatment because of stigma and shame, the anonymity afforded by an app could increase access to the help they seek.
But Ms. O’Leary warned the Food and Drug Administration does not regulate these apps, and people are sharing their personal health information on them.
The researchers conducted a review of commercially available eating disorder apps by searching the Apple and Google play stores using key phrases such as “eating disorder,” “anorexia,” and “binge eating disorder.”
They found 16 relevant apps that they added to the publicly available apps already in a database at Tufts, for a total of about 36 that were evaluated in the study (the number fluctuates as apps are deleted.)
They then reviewed the apps using the 105 questions based on the APA’s app evaluation model, which covers categories such as efficacy, privacy, accessibility, and clinical applicability. And they used filters to group apps by characteristics such as function, cost, and features.
The vast majority were self-help apps, which include things like journaling, meditation, and information on CBT. Others were reference apps that provide related definitions and sometimes include surveys to determine, for example, if the user has an eating disorder.
About 44% of the apps track mood, and 53% track symptoms. Some 56% include journaling, 42% mindfulness, 53% goal setting, and 42% psychoeducation.
Hybrid care
Only 5% of apps allow for “hybrid” care. This, explained Ms. O’Leary, is when clinicians use their own app to access patients’ apps, allowing them to track food restrictions and therapies, and make comments.
“The hybrid is viewed as the best form of app”, she said. “It’s almost like an adjunct to clinical care.”
Hybrid apps also tend to have patient safety features, she added. And these apps meet HIPAA standards, which only 11% of the apps in the study did.
Only 15% of apps advised patients to take steps in case of an emergency, and 11% had supporting studies. And where there was supporting research, much of it was funded by the app creators, said Ms. O’Leary.
For example, an app provided by Noom (the weight loss program that promises to help change habits and mindsets around food) “has a bunch of feasibility studies but they’re all funded by Noom”, which can introduce bias, she explained.
None of the apps were created by an accredited health care institution, she noted. “And I think only one app out of all the eating disorder apps we looked at was from a nonprofit.”
About 17% of the apps offer help with a “coach” or “expert”. However, these apps often fail to disclose the definition of a coach or state they’re not a replacement for medical care.
Coaching apps more expensive
Additionally, these coaching apps are often some of the most expensive, said Ms. O’Leary.
Daniel E. Gih, MD, associate professor at the University of Nebraska Medical Center, Omaha, helped start an eating disorders program at the University of Michigan and continues to treat patients with eating disorders. He said the increase in the use of eating disorder apps isn’t surprising as the incidence of these disorders increased in the wake of pandemic restrictions, especially among young people.
“Patients are likely doing more research on their medical conditions and trying to crowdsource information or self-treat,” Dr. Gih said.
It’s unclear whether “shame or just the general lack of specialized eating disorder professionals,” including physicians, is driving some of the interest in these apps, he added.
Dr. Gih stressed eating disorder apps should not only include screening for suicidality, but also explicitly tell patients to seek immediate attention if they show certain signs – for example, fainting, chest pain, or blood in emesis.
“The apps may be giving patients false hope or delaying medical care,” he said. “Apps are likely not sufficient enough to replace a multidisciplinary team with experience and expertise in eating disorders.”
Ms. O’Leary and Dr. Gih report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT APA 2023
Docs can help combat TikTok misinformation on rare psychiatric disorder
SAN FRANCISCO – , new research shows.
These findings, say investigators, underscore the need for mental health professionals to help counter the spread of false information by creating accurate content and posting it on the popular social media platform.
“Health care professionals need to make engaging content to post on social media platforms like YouTube and especially TikTok, to reach wider audiences and combat misinformation about DID,” study investigator Isreal Bladimir Munoz, a fourth-year medical student at University of Texas, Galveston, said in an interview.
The findings were presented at the annual meeting of the American Psychiatric Association.
Popularized by the media
A rare condition affecting less than 1% of the general population, DID involves two or more distinct personality states, along with changes in behavior and memory gaps.
The condition has been popularized in books and the media. Movies such as “Split,” “Psycho,” and “Fight Club” all feature characters with DID.
“These bring awareness about the condition, but also often sensationalize or stigmatize it and reinforce stereotypes,” said Mr. Munoz.
In recent years, social media has become an integral part of everyday life. An estimated 4.2 billion people actively frequent sites such as YouTube, TikTok, Twitter, and Meta.
Although social media allows for instant communication and the opportunity for self-expression, there are mounting concerns about the spread of misinformation and its potential impact on mental health and privacy, said Mr. Munoz.
To evaluate the quality and accuracy of information about DID on social media, investigators analyzed 60 YouTube and 97 TikTok videos on the condition.
To evaluate the reliability and the intent and reliability of videos, researchers used the modified DISCERN instrument and the Global Quality Scale, a five-point rating system.
Using these tools, the researchers determined whether the selected videos were useful, misleading, or neither. Mr. Munoz said videos were classified as useful if they contained accurate information about the condition and its pathogenesis, treatment, and management.
Researchers determined that for YouTube videos, 51.7% were useful, 6.6% were misleading, and 34.7% were neither. About 43.3% of these videos involved interviews, 21.7% were educational, 15% involved personal stories, 8.3% were films/TV programs, 5% were comedy skits, and 3.3% were another content type.
The highest quality YouTube videos were from educational organizations and health care professionals. The least accurate videos came from independent users and film/TV sources.
As for TikTok videos on DID, only 5.2% were useful, 10.3% were misleading, and 41.7% were neither.
The main sources for TikTok videos were independent organizations, whereas podcasts and film/TV were the least common sources.
The findings, said Mr. Munoz, underscore the need for medical professionals to develop high-quality content about DID and post it on TikTok to counter misinformation on social media.
Call to action
In a comment, Howard Y. Liu, MD, a child and adolescent psychiatrist and chair of the department of psychiatry, University of Nebraska, Omaha, described the study as “compelling.”
When it comes to public health messages, it’s important to know what social media people are using. Today’s parents are on Twitter and Facebook, whereas their children are more likely to be checking out YouTube and TikTok, said Dr. Liu, chair of the APA’s Council on Communications.
“TikTok is critical because that’s where all the youth eyeballs are,” he said.
The medical profession needs to engage with the platform to reach this next-generation audience and help stop the spread of misinformation about DID, said Dr. Liu. He noted that the APA is looking into undertaking such an initiative.
The study investigators report no relevant disclosures. Dr. Liu reports no relevant disclosures.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – , new research shows.
These findings, say investigators, underscore the need for mental health professionals to help counter the spread of false information by creating accurate content and posting it on the popular social media platform.
“Health care professionals need to make engaging content to post on social media platforms like YouTube and especially TikTok, to reach wider audiences and combat misinformation about DID,” study investigator Isreal Bladimir Munoz, a fourth-year medical student at University of Texas, Galveston, said in an interview.
The findings were presented at the annual meeting of the American Psychiatric Association.
Popularized by the media
A rare condition affecting less than 1% of the general population, DID involves two or more distinct personality states, along with changes in behavior and memory gaps.
The condition has been popularized in books and the media. Movies such as “Split,” “Psycho,” and “Fight Club” all feature characters with DID.
“These bring awareness about the condition, but also often sensationalize or stigmatize it and reinforce stereotypes,” said Mr. Munoz.
In recent years, social media has become an integral part of everyday life. An estimated 4.2 billion people actively frequent sites such as YouTube, TikTok, Twitter, and Meta.
Although social media allows for instant communication and the opportunity for self-expression, there are mounting concerns about the spread of misinformation and its potential impact on mental health and privacy, said Mr. Munoz.
To evaluate the quality and accuracy of information about DID on social media, investigators analyzed 60 YouTube and 97 TikTok videos on the condition.
To evaluate the reliability and the intent and reliability of videos, researchers used the modified DISCERN instrument and the Global Quality Scale, a five-point rating system.
Using these tools, the researchers determined whether the selected videos were useful, misleading, or neither. Mr. Munoz said videos were classified as useful if they contained accurate information about the condition and its pathogenesis, treatment, and management.
Researchers determined that for YouTube videos, 51.7% were useful, 6.6% were misleading, and 34.7% were neither. About 43.3% of these videos involved interviews, 21.7% were educational, 15% involved personal stories, 8.3% were films/TV programs, 5% were comedy skits, and 3.3% were another content type.
The highest quality YouTube videos were from educational organizations and health care professionals. The least accurate videos came from independent users and film/TV sources.
As for TikTok videos on DID, only 5.2% were useful, 10.3% were misleading, and 41.7% were neither.
The main sources for TikTok videos were independent organizations, whereas podcasts and film/TV were the least common sources.
The findings, said Mr. Munoz, underscore the need for medical professionals to develop high-quality content about DID and post it on TikTok to counter misinformation on social media.
Call to action
In a comment, Howard Y. Liu, MD, a child and adolescent psychiatrist and chair of the department of psychiatry, University of Nebraska, Omaha, described the study as “compelling.”
When it comes to public health messages, it’s important to know what social media people are using. Today’s parents are on Twitter and Facebook, whereas their children are more likely to be checking out YouTube and TikTok, said Dr. Liu, chair of the APA’s Council on Communications.
“TikTok is critical because that’s where all the youth eyeballs are,” he said.
The medical profession needs to engage with the platform to reach this next-generation audience and help stop the spread of misinformation about DID, said Dr. Liu. He noted that the APA is looking into undertaking such an initiative.
The study investigators report no relevant disclosures. Dr. Liu reports no relevant disclosures.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – , new research shows.
These findings, say investigators, underscore the need for mental health professionals to help counter the spread of false information by creating accurate content and posting it on the popular social media platform.
“Health care professionals need to make engaging content to post on social media platforms like YouTube and especially TikTok, to reach wider audiences and combat misinformation about DID,” study investigator Isreal Bladimir Munoz, a fourth-year medical student at University of Texas, Galveston, said in an interview.
The findings were presented at the annual meeting of the American Psychiatric Association.
Popularized by the media
A rare condition affecting less than 1% of the general population, DID involves two or more distinct personality states, along with changes in behavior and memory gaps.
The condition has been popularized in books and the media. Movies such as “Split,” “Psycho,” and “Fight Club” all feature characters with DID.
“These bring awareness about the condition, but also often sensationalize or stigmatize it and reinforce stereotypes,” said Mr. Munoz.
In recent years, social media has become an integral part of everyday life. An estimated 4.2 billion people actively frequent sites such as YouTube, TikTok, Twitter, and Meta.
Although social media allows for instant communication and the opportunity for self-expression, there are mounting concerns about the spread of misinformation and its potential impact on mental health and privacy, said Mr. Munoz.
To evaluate the quality and accuracy of information about DID on social media, investigators analyzed 60 YouTube and 97 TikTok videos on the condition.
To evaluate the reliability and the intent and reliability of videos, researchers used the modified DISCERN instrument and the Global Quality Scale, a five-point rating system.
Using these tools, the researchers determined whether the selected videos were useful, misleading, or neither. Mr. Munoz said videos were classified as useful if they contained accurate information about the condition and its pathogenesis, treatment, and management.
Researchers determined that for YouTube videos, 51.7% were useful, 6.6% were misleading, and 34.7% were neither. About 43.3% of these videos involved interviews, 21.7% were educational, 15% involved personal stories, 8.3% were films/TV programs, 5% were comedy skits, and 3.3% were another content type.
The highest quality YouTube videos were from educational organizations and health care professionals. The least accurate videos came from independent users and film/TV sources.
As for TikTok videos on DID, only 5.2% were useful, 10.3% were misleading, and 41.7% were neither.
The main sources for TikTok videos were independent organizations, whereas podcasts and film/TV were the least common sources.
The findings, said Mr. Munoz, underscore the need for medical professionals to develop high-quality content about DID and post it on TikTok to counter misinformation on social media.
Call to action
In a comment, Howard Y. Liu, MD, a child and adolescent psychiatrist and chair of the department of psychiatry, University of Nebraska, Omaha, described the study as “compelling.”
When it comes to public health messages, it’s important to know what social media people are using. Today’s parents are on Twitter and Facebook, whereas their children are more likely to be checking out YouTube and TikTok, said Dr. Liu, chair of the APA’s Council on Communications.
“TikTok is critical because that’s where all the youth eyeballs are,” he said.
The medical profession needs to engage with the platform to reach this next-generation audience and help stop the spread of misinformation about DID, said Dr. Liu. He noted that the APA is looking into undertaking such an initiative.
The study investigators report no relevant disclosures. Dr. Liu reports no relevant disclosures.
A version of this article first appeared on Medscape.com.
AT APA 2023
The family firearm often used in youth suicide
SAN FRANCISCO – , according to results of a novel “psychological autopsy study” of loved ones of youth who died by gun-related suicide.
Yet, families don’t always recognize the danger firearms pose to a young person with suicide risk factors, even when there is a young person in the house with a mental health condition, the data show.
Perhaps most importantly, many parents indicated that they would have removed firearms from the home if it had been suggested by their health care professionals.
The study was presented at the American Psychiatric Association annual meeting.
The message is very clear: Clinicians need to ask about guns and gun safety with patients and families, said study investigator Paul Nestadt, MD, of Johns Hopkins Bloomberg School of Public Health in Baltimore.
“It’s never illegal to ask about gun access and it’s medically relevant. Just do it,” he said during a briefing with reporters.
Grim statistics
Suicide rates have been climbing in the United States for the majority of the past 20 years. Suicide is the second most common cause of death among youth.
Dr. Nestadt noted that overall about 8% of suicide attempts result in death, but when an attempt involves a firearm the percentage jumps astronomically to 90%.
Research has shown that for every 10% increase in household firearms in a given community there is a 27% increase in youth suicide deaths.
“In the world of public health and mental health, we think about having access to firearms as an important risk factor for completed suicide. But in the United States, guns have become an important part of how many Americans see themselves,” Dr. Nestadt told reporters.
Research has shown that half of gun owners say owning a gun is central to their identity and three quarters say it’s essential to their freedom, he noted.
To explore these attitudes further, Dr. Nestadt and colleagues did 11 “psychological autopsy interviews” with the loved ones of nine young people aged 17-21 who died by gun-related suicide. They interviewed six mothers, three fathers, one sibling, and one close friend.
Most of the families had some level of “familial engagement” with firearms, Dr. Nestadt reported.
In more than two-thirds of the families, the youth used a family-owned firearm to commit suicide.
Notably, more than three-quarters of the youth had received mental health care before taking their lives, with many receiving care in the weeks prior to their suicide; 44% had made a prior suicide attempt.
In many cases, parents shared that they had not considered their family-owned firearms to be sources of danger and indicated that had their clinicians expressed concern about the gun in the home, they may have acted to reduce the risk by removing it.
Several also shared that they would have considered using Maryland’s Extreme Risk Protective Order Law if it had existed at the time and they had been made aware of it.
Extreme risk protection order (ERPO) laws, or “red flag laws,” prohibit individuals at risk for harming themselves or others from purchasing or owning a firearm.
Dr. Nestadt said youth suicide interventions “must acknowledge culturally embedded roots of identity formation while rescripting firearms from expressions of family cohesion to instruments that may undermine that cohesion.”
‘Courageous study’
Dr. Nestadt noted that while this study was challenging on many fronts, it took no convincing to get these grieving families to participate.
“They wanted to talk to us, especially because they were hopeful that our work could help prevent future suicides, but also they wanted to talk about their loved ones,” he said.
“When you lose someone to cancer, people give you hugs and flowers. When you lose someone to suicide, people don’t discuss it. Suicide has a stigma to it.”
Briefing moderator Howard Liu, MD, MBA, chair of the department of psychiatry, University of Nebraska Medical Center, Omaha, praised the study team for a “courageous study that really required a tremendous amount of vulnerability from the research team and clearly from the survivors as well.”
This is an “important and timely public health discussion,” said Dr. Liu, chair of the APA Council on Communications.
“We’re all facing this challenge of how do we reduce suicide across all ages, from youth to adults as well. This is a really vital discussion and such an important clue about access and trying to reduce access in a moment of impulsivity,” he added.
The study had no commercial funding. Dr. Nestadt and Dr. Liu report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – , according to results of a novel “psychological autopsy study” of loved ones of youth who died by gun-related suicide.
Yet, families don’t always recognize the danger firearms pose to a young person with suicide risk factors, even when there is a young person in the house with a mental health condition, the data show.
Perhaps most importantly, many parents indicated that they would have removed firearms from the home if it had been suggested by their health care professionals.
The study was presented at the American Psychiatric Association annual meeting.
The message is very clear: Clinicians need to ask about guns and gun safety with patients and families, said study investigator Paul Nestadt, MD, of Johns Hopkins Bloomberg School of Public Health in Baltimore.
“It’s never illegal to ask about gun access and it’s medically relevant. Just do it,” he said during a briefing with reporters.
Grim statistics
Suicide rates have been climbing in the United States for the majority of the past 20 years. Suicide is the second most common cause of death among youth.
Dr. Nestadt noted that overall about 8% of suicide attempts result in death, but when an attempt involves a firearm the percentage jumps astronomically to 90%.
Research has shown that for every 10% increase in household firearms in a given community there is a 27% increase in youth suicide deaths.
“In the world of public health and mental health, we think about having access to firearms as an important risk factor for completed suicide. But in the United States, guns have become an important part of how many Americans see themselves,” Dr. Nestadt told reporters.
Research has shown that half of gun owners say owning a gun is central to their identity and three quarters say it’s essential to their freedom, he noted.
To explore these attitudes further, Dr. Nestadt and colleagues did 11 “psychological autopsy interviews” with the loved ones of nine young people aged 17-21 who died by gun-related suicide. They interviewed six mothers, three fathers, one sibling, and one close friend.
Most of the families had some level of “familial engagement” with firearms, Dr. Nestadt reported.
In more than two-thirds of the families, the youth used a family-owned firearm to commit suicide.
Notably, more than three-quarters of the youth had received mental health care before taking their lives, with many receiving care in the weeks prior to their suicide; 44% had made a prior suicide attempt.
In many cases, parents shared that they had not considered their family-owned firearms to be sources of danger and indicated that had their clinicians expressed concern about the gun in the home, they may have acted to reduce the risk by removing it.
Several also shared that they would have considered using Maryland’s Extreme Risk Protective Order Law if it had existed at the time and they had been made aware of it.
Extreme risk protection order (ERPO) laws, or “red flag laws,” prohibit individuals at risk for harming themselves or others from purchasing or owning a firearm.
Dr. Nestadt said youth suicide interventions “must acknowledge culturally embedded roots of identity formation while rescripting firearms from expressions of family cohesion to instruments that may undermine that cohesion.”
‘Courageous study’
Dr. Nestadt noted that while this study was challenging on many fronts, it took no convincing to get these grieving families to participate.
“They wanted to talk to us, especially because they were hopeful that our work could help prevent future suicides, but also they wanted to talk about their loved ones,” he said.
“When you lose someone to cancer, people give you hugs and flowers. When you lose someone to suicide, people don’t discuss it. Suicide has a stigma to it.”
Briefing moderator Howard Liu, MD, MBA, chair of the department of psychiatry, University of Nebraska Medical Center, Omaha, praised the study team for a “courageous study that really required a tremendous amount of vulnerability from the research team and clearly from the survivors as well.”
This is an “important and timely public health discussion,” said Dr. Liu, chair of the APA Council on Communications.
“We’re all facing this challenge of how do we reduce suicide across all ages, from youth to adults as well. This is a really vital discussion and such an important clue about access and trying to reduce access in a moment of impulsivity,” he added.
The study had no commercial funding. Dr. Nestadt and Dr. Liu report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – , according to results of a novel “psychological autopsy study” of loved ones of youth who died by gun-related suicide.
Yet, families don’t always recognize the danger firearms pose to a young person with suicide risk factors, even when there is a young person in the house with a mental health condition, the data show.
Perhaps most importantly, many parents indicated that they would have removed firearms from the home if it had been suggested by their health care professionals.
The study was presented at the American Psychiatric Association annual meeting.
The message is very clear: Clinicians need to ask about guns and gun safety with patients and families, said study investigator Paul Nestadt, MD, of Johns Hopkins Bloomberg School of Public Health in Baltimore.
“It’s never illegal to ask about gun access and it’s medically relevant. Just do it,” he said during a briefing with reporters.
Grim statistics
Suicide rates have been climbing in the United States for the majority of the past 20 years. Suicide is the second most common cause of death among youth.
Dr. Nestadt noted that overall about 8% of suicide attempts result in death, but when an attempt involves a firearm the percentage jumps astronomically to 90%.
Research has shown that for every 10% increase in household firearms in a given community there is a 27% increase in youth suicide deaths.
“In the world of public health and mental health, we think about having access to firearms as an important risk factor for completed suicide. But in the United States, guns have become an important part of how many Americans see themselves,” Dr. Nestadt told reporters.
Research has shown that half of gun owners say owning a gun is central to their identity and three quarters say it’s essential to their freedom, he noted.
To explore these attitudes further, Dr. Nestadt and colleagues did 11 “psychological autopsy interviews” with the loved ones of nine young people aged 17-21 who died by gun-related suicide. They interviewed six mothers, three fathers, one sibling, and one close friend.
Most of the families had some level of “familial engagement” with firearms, Dr. Nestadt reported.
In more than two-thirds of the families, the youth used a family-owned firearm to commit suicide.
Notably, more than three-quarters of the youth had received mental health care before taking their lives, with many receiving care in the weeks prior to their suicide; 44% had made a prior suicide attempt.
In many cases, parents shared that they had not considered their family-owned firearms to be sources of danger and indicated that had their clinicians expressed concern about the gun in the home, they may have acted to reduce the risk by removing it.
Several also shared that they would have considered using Maryland’s Extreme Risk Protective Order Law if it had existed at the time and they had been made aware of it.
Extreme risk protection order (ERPO) laws, or “red flag laws,” prohibit individuals at risk for harming themselves or others from purchasing or owning a firearm.
Dr. Nestadt said youth suicide interventions “must acknowledge culturally embedded roots of identity formation while rescripting firearms from expressions of family cohesion to instruments that may undermine that cohesion.”
‘Courageous study’
Dr. Nestadt noted that while this study was challenging on many fronts, it took no convincing to get these grieving families to participate.
“They wanted to talk to us, especially because they were hopeful that our work could help prevent future suicides, but also they wanted to talk about their loved ones,” he said.
“When you lose someone to cancer, people give you hugs and flowers. When you lose someone to suicide, people don’t discuss it. Suicide has a stigma to it.”
Briefing moderator Howard Liu, MD, MBA, chair of the department of psychiatry, University of Nebraska Medical Center, Omaha, praised the study team for a “courageous study that really required a tremendous amount of vulnerability from the research team and clearly from the survivors as well.”
This is an “important and timely public health discussion,” said Dr. Liu, chair of the APA Council on Communications.
“We’re all facing this challenge of how do we reduce suicide across all ages, from youth to adults as well. This is a really vital discussion and such an important clue about access and trying to reduce access in a moment of impulsivity,” he added.
The study had no commercial funding. Dr. Nestadt and Dr. Liu report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT APA 2023
Black patients most likely to be restrained in EDs, Latino patients least likely
SAN FRANCISCO – .
In contrast, Hispanic/Latino patients were less likely to be restrained than both Black and White patients, researchers reported in a poster presented at the annual meeting of the American Psychiatric Association. The study authors also found that clinicians rarely turned to restraints, using them in just 2,712 of 882,390 ED visits (0.3%) over a 7-year period.
The study doesn’t examine why the disparities exist. But lead author Erika Chang-Sing, a medical student at Yale University, New Haven, Conn., said in an interview that it’s clear that racial bias is the cause of the differences in restraint rates among White, Black, and Hispanics/Latino patients. “We think that there are multiple contributing factors to the higher rates of restraint for Black patients brought to the hospital by police, and all of them are rooted in systemic racism,” she said, adding that “the lower odds of restraint in the Hispanic or Latino group are also rooted in systemic racism and inequity.”
According to Ms. Chang-Sing, researchers launched the study to gain insight into the use of the restraints in the Southeast and to see what’s happening in light of the recent publicizing of killings of Black people by police. Being taken to the hospital by police “might contribute both to the individual patient’s behavior and the health care provider’s assessment of risk in determining whether or not to apply restraints,” she said.
Other research has linked ethnicity to higher rates of restraint use. For example, a 2021 study of 32,054 cases of patients under mandatory psychiatric hold in 11 Massachusetts emergency rooms found that Black (adjusted odds ratio, 1.22) and Hispanic (aOR, 1.45) patients were more likely to be restrained than White patients.
For the new study, researchers retrospectively tracked 885,102 emergency room visits at three North Carolina emergency departments from 2015 to 2022, including 9,130 who were brought in by police and 2,712 who were physically restrained because of the perceived risk of violence. “Providers use restraints, or straps, to secure the patient’s wrists and ankles to the bed,” Ms. Chang-Sing said.
Among all patients, 52.5% were Black, but 66% of those who were restrained were Black. The numbers for White patients were 35.7% and 23.9%, respectively, and 5.7% and 3.2% for Hispanics/Latino patients. Black patients were less likely than White patients to get a psychiatric primary emergency department diagnosis (aOR, 0.67), but those in that category were more likely than their White counterparts to be restrained (aOR, 1.36).
The higher risk of restraint use in Black patients overall disappeared when researchers adjusted their statistics to account for the effects of sex, age, and type of insurance (aOR, 0.86). Ms. Chang-Sing said the study team is reanalyzing the data since they think insurance may not be a confounder.
Why might Hispanic/Latino ethnicity be protective against restraint use? “This may be due to language barriers, fear of law enforcement, and avoidance of the hospital in the first place,” Ms. Chang-Sing said.
Emergency physician Wendy Macias-Konstantopoulos, MD, MPH, MBA, of Harvard Medical School and Massachusetts General Hospital, both in Boston, coauthored the 2021 study on police restraints. In an interview, she said the new findings add to previous research by providing data about the role played by the police who bring patients to the ED. She added that there is no evidence that certain populations simply need more restraints.
What can be done to reduce disparities in restraint use? Mental health teams can make a difference by responding to mental health emergencies, Ms. Chang-Sing said. “These providers can be instrumental in communicating to patients that the intention is to care for them, not to punish them.”
Another strategy is to increase the number of clinics and crisis response centers, she said. Hospital-based crisis response teams can also be helpful, she said. “Because these teams are focused only on behavioral emergencies, they can be more thoughtful in avoiding the use of restraints.”
No study funding was reported. The study authors and Dr. Macias-Konstantopoulos have no disclosures.
SAN FRANCISCO – .
In contrast, Hispanic/Latino patients were less likely to be restrained than both Black and White patients, researchers reported in a poster presented at the annual meeting of the American Psychiatric Association. The study authors also found that clinicians rarely turned to restraints, using them in just 2,712 of 882,390 ED visits (0.3%) over a 7-year period.
The study doesn’t examine why the disparities exist. But lead author Erika Chang-Sing, a medical student at Yale University, New Haven, Conn., said in an interview that it’s clear that racial bias is the cause of the differences in restraint rates among White, Black, and Hispanics/Latino patients. “We think that there are multiple contributing factors to the higher rates of restraint for Black patients brought to the hospital by police, and all of them are rooted in systemic racism,” she said, adding that “the lower odds of restraint in the Hispanic or Latino group are also rooted in systemic racism and inequity.”
According to Ms. Chang-Sing, researchers launched the study to gain insight into the use of the restraints in the Southeast and to see what’s happening in light of the recent publicizing of killings of Black people by police. Being taken to the hospital by police “might contribute both to the individual patient’s behavior and the health care provider’s assessment of risk in determining whether or not to apply restraints,” she said.
Other research has linked ethnicity to higher rates of restraint use. For example, a 2021 study of 32,054 cases of patients under mandatory psychiatric hold in 11 Massachusetts emergency rooms found that Black (adjusted odds ratio, 1.22) and Hispanic (aOR, 1.45) patients were more likely to be restrained than White patients.
For the new study, researchers retrospectively tracked 885,102 emergency room visits at three North Carolina emergency departments from 2015 to 2022, including 9,130 who were brought in by police and 2,712 who were physically restrained because of the perceived risk of violence. “Providers use restraints, or straps, to secure the patient’s wrists and ankles to the bed,” Ms. Chang-Sing said.
Among all patients, 52.5% were Black, but 66% of those who were restrained were Black. The numbers for White patients were 35.7% and 23.9%, respectively, and 5.7% and 3.2% for Hispanics/Latino patients. Black patients were less likely than White patients to get a psychiatric primary emergency department diagnosis (aOR, 0.67), but those in that category were more likely than their White counterparts to be restrained (aOR, 1.36).
The higher risk of restraint use in Black patients overall disappeared when researchers adjusted their statistics to account for the effects of sex, age, and type of insurance (aOR, 0.86). Ms. Chang-Sing said the study team is reanalyzing the data since they think insurance may not be a confounder.
Why might Hispanic/Latino ethnicity be protective against restraint use? “This may be due to language barriers, fear of law enforcement, and avoidance of the hospital in the first place,” Ms. Chang-Sing said.
Emergency physician Wendy Macias-Konstantopoulos, MD, MPH, MBA, of Harvard Medical School and Massachusetts General Hospital, both in Boston, coauthored the 2021 study on police restraints. In an interview, she said the new findings add to previous research by providing data about the role played by the police who bring patients to the ED. She added that there is no evidence that certain populations simply need more restraints.
What can be done to reduce disparities in restraint use? Mental health teams can make a difference by responding to mental health emergencies, Ms. Chang-Sing said. “These providers can be instrumental in communicating to patients that the intention is to care for them, not to punish them.”
Another strategy is to increase the number of clinics and crisis response centers, she said. Hospital-based crisis response teams can also be helpful, she said. “Because these teams are focused only on behavioral emergencies, they can be more thoughtful in avoiding the use of restraints.”
No study funding was reported. The study authors and Dr. Macias-Konstantopoulos have no disclosures.
SAN FRANCISCO – .
In contrast, Hispanic/Latino patients were less likely to be restrained than both Black and White patients, researchers reported in a poster presented at the annual meeting of the American Psychiatric Association. The study authors also found that clinicians rarely turned to restraints, using them in just 2,712 of 882,390 ED visits (0.3%) over a 7-year period.
The study doesn’t examine why the disparities exist. But lead author Erika Chang-Sing, a medical student at Yale University, New Haven, Conn., said in an interview that it’s clear that racial bias is the cause of the differences in restraint rates among White, Black, and Hispanics/Latino patients. “We think that there are multiple contributing factors to the higher rates of restraint for Black patients brought to the hospital by police, and all of them are rooted in systemic racism,” she said, adding that “the lower odds of restraint in the Hispanic or Latino group are also rooted in systemic racism and inequity.”
According to Ms. Chang-Sing, researchers launched the study to gain insight into the use of the restraints in the Southeast and to see what’s happening in light of the recent publicizing of killings of Black people by police. Being taken to the hospital by police “might contribute both to the individual patient’s behavior and the health care provider’s assessment of risk in determining whether or not to apply restraints,” she said.
Other research has linked ethnicity to higher rates of restraint use. For example, a 2021 study of 32,054 cases of patients under mandatory psychiatric hold in 11 Massachusetts emergency rooms found that Black (adjusted odds ratio, 1.22) and Hispanic (aOR, 1.45) patients were more likely to be restrained than White patients.
For the new study, researchers retrospectively tracked 885,102 emergency room visits at three North Carolina emergency departments from 2015 to 2022, including 9,130 who were brought in by police and 2,712 who were physically restrained because of the perceived risk of violence. “Providers use restraints, or straps, to secure the patient’s wrists and ankles to the bed,” Ms. Chang-Sing said.
Among all patients, 52.5% were Black, but 66% of those who were restrained were Black. The numbers for White patients were 35.7% and 23.9%, respectively, and 5.7% and 3.2% for Hispanics/Latino patients. Black patients were less likely than White patients to get a psychiatric primary emergency department diagnosis (aOR, 0.67), but those in that category were more likely than their White counterparts to be restrained (aOR, 1.36).
The higher risk of restraint use in Black patients overall disappeared when researchers adjusted their statistics to account for the effects of sex, age, and type of insurance (aOR, 0.86). Ms. Chang-Sing said the study team is reanalyzing the data since they think insurance may not be a confounder.
Why might Hispanic/Latino ethnicity be protective against restraint use? “This may be due to language barriers, fear of law enforcement, and avoidance of the hospital in the first place,” Ms. Chang-Sing said.
Emergency physician Wendy Macias-Konstantopoulos, MD, MPH, MBA, of Harvard Medical School and Massachusetts General Hospital, both in Boston, coauthored the 2021 study on police restraints. In an interview, she said the new findings add to previous research by providing data about the role played by the police who bring patients to the ED. She added that there is no evidence that certain populations simply need more restraints.
What can be done to reduce disparities in restraint use? Mental health teams can make a difference by responding to mental health emergencies, Ms. Chang-Sing said. “These providers can be instrumental in communicating to patients that the intention is to care for them, not to punish them.”
Another strategy is to increase the number of clinics and crisis response centers, she said. Hospital-based crisis response teams can also be helpful, she said. “Because these teams are focused only on behavioral emergencies, they can be more thoughtful in avoiding the use of restraints.”
No study funding was reported. The study authors and Dr. Macias-Konstantopoulos have no disclosures.
AT APA 2023