User login
Half of all breast cancer survivors conceived naturally within 3 months of trying
SAN ANTONIO – Half of premenopausal breast cancer patients who had completed chemotherapy conceived by intercourse alone within 3 months of beginning to attempt conception, a study showed.
This single-center study provides some guidance for women and the physicians caring for them that an attempt at natural conception is worthwhile if ovarian function has returned after chemotherapy, said Nikita Sinha.
Speaking at the annual meeting of the American Society for Reproductive Medicine, Ms. Sinha, a medical student at the University of California, San Francisco, said that this is a worthwhile strategy, “even for patients with limited ovarian reserve, prior to using cryopreserved tissue.” Cytotoxicity of chemotherapy was not associated with decreased chances for conception, she said.
Ms. Sinha and her colleagues designed a prospective cohort study to follow women aged 18-44 years who had been diagnosed with breast cancer and had received a fertility preservation consult. A total of 297 women who had completed cancer treatment were contacted and asked to complete a survey that asked questions about their oncologic and reproductive history. Of these, 200 (67%) completed the survey, but 43 more patients were excluded because they had not received chemotherapy.
Of the remaining 157 women, 40 (25%) attempted to conceive. Return of ovarian function occurred in 36 of the 40 women (90%). Of these 36 women, 4 also began their attempts to conceive with assisted reproductive technology (ART) because of age, previous history of infertility, or a preimplantation genetic diagnosis of the BRCA mutation. Thus, a total of eight patients (20%) first attempted to conceive with ART.
Three-fourths of women in both groups had eggs or embryos cryopreserved before their chemotherapy. In the ART group, a total of five women (62.5%) became pregnant: One first attempted intrauterine insemination and became pregnant; two first attempted pregnancy by egg donation, and one became pregnant; and three of five women who attempted embryo transfer from cryopreserved eggs or embryos became pregnant.
Of the 32 women who first attempted to conceive by intercourse, 18 became pregnant after 3 months, and 16 women had a live birth, for a 50% live birth rate for this group. Of the remaining 14 women who did not become pregnant by intercourse, 8 went on to attempt conception by ART.
Of these eight women, intrauterine insemination was attempted by three, with two resulting pregnancies. The single patient who used letrozole became pregnant. Of the four patients who attempted frozen embryo transfer, two became pregnant, for a total of five pregnancies (62.5%).
Comparing the 18 women who became pregnant with the 14 women who did not, Ms. Sinha and her colleagues found no significant differences in age, parity, hormone receptor status, pre- or postchemotherapy antral follicle count, type of chemotherapy, or time since chemotherapy. Receiving leuprolide acetate during therapy was not a significant factor.
Of the patients who became pregnant, 2 of 28 (7%) have had a recurrence of their breast cancer; both of these patients are estrogen receptor positive, said Ms. Sinha. One of the 12 patients who didn’t become pregnant also has had a recurrence; she is estrogen receptor negative.
In this study, the winnowing process of patient selection resulted in a limited sample size, with the potential for selection bias, said Ms. Sinha. Data collection is ongoing for breast cancer patients who receive fertility preservation consultations at her facility, she said.
The women trying to conceive were, on average, 37 years old at their initial attempt at conception, and had completed chemotherapy about 4 years ago. Most patients received cytotoxic chemotherapy, and 25 (63%) had estrogen receptor–positive cancer.
Previous work had shown that up to 80% of women of reproductive age will have some ovarian function resume after treatment with gonadotoxic chemotherapy agents, said Ms. Sinha.
However, the fertility risk for cancer survivors is twofold, said Ms. Sinha. “While acute ovarian failure is a well-known risk, there remains an increased risk of early menopause despite resumption of menses, especially in younger aged women” who are cancer survivors, she said.
Ms. Sinha reported that her work was supported by the University of California, San Francisco Clinical and Translational Science Institute.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN ANTONIO – Half of premenopausal breast cancer patients who had completed chemotherapy conceived by intercourse alone within 3 months of beginning to attempt conception, a study showed.
This single-center study provides some guidance for women and the physicians caring for them that an attempt at natural conception is worthwhile if ovarian function has returned after chemotherapy, said Nikita Sinha.
Speaking at the annual meeting of the American Society for Reproductive Medicine, Ms. Sinha, a medical student at the University of California, San Francisco, said that this is a worthwhile strategy, “even for patients with limited ovarian reserve, prior to using cryopreserved tissue.” Cytotoxicity of chemotherapy was not associated with decreased chances for conception, she said.
Ms. Sinha and her colleagues designed a prospective cohort study to follow women aged 18-44 years who had been diagnosed with breast cancer and had received a fertility preservation consult. A total of 297 women who had completed cancer treatment were contacted and asked to complete a survey that asked questions about their oncologic and reproductive history. Of these, 200 (67%) completed the survey, but 43 more patients were excluded because they had not received chemotherapy.
Of the remaining 157 women, 40 (25%) attempted to conceive. Return of ovarian function occurred in 36 of the 40 women (90%). Of these 36 women, 4 also began their attempts to conceive with assisted reproductive technology (ART) because of age, previous history of infertility, or a preimplantation genetic diagnosis of the BRCA mutation. Thus, a total of eight patients (20%) first attempted to conceive with ART.
Three-fourths of women in both groups had eggs or embryos cryopreserved before their chemotherapy. In the ART group, a total of five women (62.5%) became pregnant: One first attempted intrauterine insemination and became pregnant; two first attempted pregnancy by egg donation, and one became pregnant; and three of five women who attempted embryo transfer from cryopreserved eggs or embryos became pregnant.
Of the 32 women who first attempted to conceive by intercourse, 18 became pregnant after 3 months, and 16 women had a live birth, for a 50% live birth rate for this group. Of the remaining 14 women who did not become pregnant by intercourse, 8 went on to attempt conception by ART.
Of these eight women, intrauterine insemination was attempted by three, with two resulting pregnancies. The single patient who used letrozole became pregnant. Of the four patients who attempted frozen embryo transfer, two became pregnant, for a total of five pregnancies (62.5%).
Comparing the 18 women who became pregnant with the 14 women who did not, Ms. Sinha and her colleagues found no significant differences in age, parity, hormone receptor status, pre- or postchemotherapy antral follicle count, type of chemotherapy, or time since chemotherapy. Receiving leuprolide acetate during therapy was not a significant factor.
Of the patients who became pregnant, 2 of 28 (7%) have had a recurrence of their breast cancer; both of these patients are estrogen receptor positive, said Ms. Sinha. One of the 12 patients who didn’t become pregnant also has had a recurrence; she is estrogen receptor negative.
In this study, the winnowing process of patient selection resulted in a limited sample size, with the potential for selection bias, said Ms. Sinha. Data collection is ongoing for breast cancer patients who receive fertility preservation consultations at her facility, she said.
The women trying to conceive were, on average, 37 years old at their initial attempt at conception, and had completed chemotherapy about 4 years ago. Most patients received cytotoxic chemotherapy, and 25 (63%) had estrogen receptor–positive cancer.
Previous work had shown that up to 80% of women of reproductive age will have some ovarian function resume after treatment with gonadotoxic chemotherapy agents, said Ms. Sinha.
However, the fertility risk for cancer survivors is twofold, said Ms. Sinha. “While acute ovarian failure is a well-known risk, there remains an increased risk of early menopause despite resumption of menses, especially in younger aged women” who are cancer survivors, she said.
Ms. Sinha reported that her work was supported by the University of California, San Francisco Clinical and Translational Science Institute.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN ANTONIO – Half of premenopausal breast cancer patients who had completed chemotherapy conceived by intercourse alone within 3 months of beginning to attempt conception, a study showed.
This single-center study provides some guidance for women and the physicians caring for them that an attempt at natural conception is worthwhile if ovarian function has returned after chemotherapy, said Nikita Sinha.
Speaking at the annual meeting of the American Society for Reproductive Medicine, Ms. Sinha, a medical student at the University of California, San Francisco, said that this is a worthwhile strategy, “even for patients with limited ovarian reserve, prior to using cryopreserved tissue.” Cytotoxicity of chemotherapy was not associated with decreased chances for conception, she said.
Ms. Sinha and her colleagues designed a prospective cohort study to follow women aged 18-44 years who had been diagnosed with breast cancer and had received a fertility preservation consult. A total of 297 women who had completed cancer treatment were contacted and asked to complete a survey that asked questions about their oncologic and reproductive history. Of these, 200 (67%) completed the survey, but 43 more patients were excluded because they had not received chemotherapy.
Of the remaining 157 women, 40 (25%) attempted to conceive. Return of ovarian function occurred in 36 of the 40 women (90%). Of these 36 women, 4 also began their attempts to conceive with assisted reproductive technology (ART) because of age, previous history of infertility, or a preimplantation genetic diagnosis of the BRCA mutation. Thus, a total of eight patients (20%) first attempted to conceive with ART.
Three-fourths of women in both groups had eggs or embryos cryopreserved before their chemotherapy. In the ART group, a total of five women (62.5%) became pregnant: One first attempted intrauterine insemination and became pregnant; two first attempted pregnancy by egg donation, and one became pregnant; and three of five women who attempted embryo transfer from cryopreserved eggs or embryos became pregnant.
Of the 32 women who first attempted to conceive by intercourse, 18 became pregnant after 3 months, and 16 women had a live birth, for a 50% live birth rate for this group. Of the remaining 14 women who did not become pregnant by intercourse, 8 went on to attempt conception by ART.
Of these eight women, intrauterine insemination was attempted by three, with two resulting pregnancies. The single patient who used letrozole became pregnant. Of the four patients who attempted frozen embryo transfer, two became pregnant, for a total of five pregnancies (62.5%).
Comparing the 18 women who became pregnant with the 14 women who did not, Ms. Sinha and her colleagues found no significant differences in age, parity, hormone receptor status, pre- or postchemotherapy antral follicle count, type of chemotherapy, or time since chemotherapy. Receiving leuprolide acetate during therapy was not a significant factor.
Of the patients who became pregnant, 2 of 28 (7%) have had a recurrence of their breast cancer; both of these patients are estrogen receptor positive, said Ms. Sinha. One of the 12 patients who didn’t become pregnant also has had a recurrence; she is estrogen receptor negative.
In this study, the winnowing process of patient selection resulted in a limited sample size, with the potential for selection bias, said Ms. Sinha. Data collection is ongoing for breast cancer patients who receive fertility preservation consultations at her facility, she said.
The women trying to conceive were, on average, 37 years old at their initial attempt at conception, and had completed chemotherapy about 4 years ago. Most patients received cytotoxic chemotherapy, and 25 (63%) had estrogen receptor–positive cancer.
Previous work had shown that up to 80% of women of reproductive age will have some ovarian function resume after treatment with gonadotoxic chemotherapy agents, said Ms. Sinha.
However, the fertility risk for cancer survivors is twofold, said Ms. Sinha. “While acute ovarian failure is a well-known risk, there remains an increased risk of early menopause despite resumption of menses, especially in younger aged women” who are cancer survivors, she said.
Ms. Sinha reported that her work was supported by the University of California, San Francisco Clinical and Translational Science Institute.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT ASRM 2017
Key clinical point:
Major finding: Of 36 women whose ovarian function resumed after chemotherapy, 18 (50%) conceived within 3 months of attempting conception.
Data source: A single-center prospective cohort study of women diagnosed with breast cancer who received fertility preservation consultation.
Disclosures: The study was funded by the University of California, San Francisco Clinical and Translational Science Institute.
Ectopic pregnancies predicted by easy-to-use risk stratification model
SAN ANTONIO – An easy-to-use risk stratification tool accurately predicted which pregnancies of unknown location were ectopic pregnancies by using a model validated by retrospective chart review.
Reeva Makhijani, MD, and her colleagues built the tool using a composite of risk factors to create a “generalized additive model,” or GAM, in combination with beta HCG levels. They presented the results during a poster session at the annual meeting of the American Society for Reproductive Medicine.
The model showed that a prior history of ectopic pregnancy (EP) (P = .0045), a history of pelvic surgery (P = .397), and a presentation of vaginal bleeding (P = .0003) all significantly increased the risk of EP.
Another statistical measure, the area under the receiver operating curve (AUC), helps estimate the likelihood of EP according to beta-HCG levels. When the initial beta-HCG was considered together with the ratio of the initial beta HCG to the presenting beta-HCG, the AUC was 0.889. For the initial beta-HCG level alone, the AUC was 0.793, while for the ratio alone, the AUC was 0.88. Higher AUC figures indicate more predictive power.
Dr. Makhijani, an ob.gyn. resident physician at Brown University, Providence, R.I., and her colleagues have built a prototype of a computer application that calculates risk of EP when the significant risk factors and lab values are entered.
After reviewing the electronic medical records of 800 patients who had pregnancies of unknown location (PUL), in the final analysis Dr. Makhijani and her coauthors included 398 patients whose medical histories allowed assessment of risk factors and whose record included at least two beta-HCG values taken 36-72 hours apart. The investigators also excluded patients with molar pregnancies, ruptured EPs, or who had undergone surgery before a second beta-HCG was obtained.
Of the 398 patients, 40 (10%) were eventually found to have EP, while 168 (42%) had an intrauterine pregnancy, and 190 (48%) were diagnosed with spontaneous abortion.
The patients were about 27 years old on average, and just over half (n = 224) were parous. Vaginal bleeding was a presenting sign in 233 patients, and 284 had abdominal pain. Of those with EP, 34 of 40 had vaginal bleeding, and 25 of 40 had abdominal pain.
In addition to the three factors found to have significant association with EP, the investigators initially considered a number of other patient characteristics, including age, parity, and presentation with abdominal pain. Additional risk factors examined included history of infertility, pelvic inflammatory disease, sexually transmitted disease, intrauterine device placement, and diethylstilbestrol (DES) exposure. None of these were significantly associated with risk of EP.
“Our model can be translated into an easy-to-use risk stratification tool that can accurately predict the risk of EP,” said Dr. Makhijani and her coauthors. “This tool could potentially be used by clinicians and ob.gyn. residencies nationally as [pregnancies of unknown location] are a very common management scenario.”
Dr. Makhijani reported having no disclosures and no outside sources of funding.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN ANTONIO – An easy-to-use risk stratification tool accurately predicted which pregnancies of unknown location were ectopic pregnancies by using a model validated by retrospective chart review.
Reeva Makhijani, MD, and her colleagues built the tool using a composite of risk factors to create a “generalized additive model,” or GAM, in combination with beta HCG levels. They presented the results during a poster session at the annual meeting of the American Society for Reproductive Medicine.
The model showed that a prior history of ectopic pregnancy (EP) (P = .0045), a history of pelvic surgery (P = .397), and a presentation of vaginal bleeding (P = .0003) all significantly increased the risk of EP.
Another statistical measure, the area under the receiver operating curve (AUC), helps estimate the likelihood of EP according to beta-HCG levels. When the initial beta-HCG was considered together with the ratio of the initial beta HCG to the presenting beta-HCG, the AUC was 0.889. For the initial beta-HCG level alone, the AUC was 0.793, while for the ratio alone, the AUC was 0.88. Higher AUC figures indicate more predictive power.
Dr. Makhijani, an ob.gyn. resident physician at Brown University, Providence, R.I., and her colleagues have built a prototype of a computer application that calculates risk of EP when the significant risk factors and lab values are entered.
After reviewing the electronic medical records of 800 patients who had pregnancies of unknown location (PUL), in the final analysis Dr. Makhijani and her coauthors included 398 patients whose medical histories allowed assessment of risk factors and whose record included at least two beta-HCG values taken 36-72 hours apart. The investigators also excluded patients with molar pregnancies, ruptured EPs, or who had undergone surgery before a second beta-HCG was obtained.
Of the 398 patients, 40 (10%) were eventually found to have EP, while 168 (42%) had an intrauterine pregnancy, and 190 (48%) were diagnosed with spontaneous abortion.
The patients were about 27 years old on average, and just over half (n = 224) were parous. Vaginal bleeding was a presenting sign in 233 patients, and 284 had abdominal pain. Of those with EP, 34 of 40 had vaginal bleeding, and 25 of 40 had abdominal pain.
In addition to the three factors found to have significant association with EP, the investigators initially considered a number of other patient characteristics, including age, parity, and presentation with abdominal pain. Additional risk factors examined included history of infertility, pelvic inflammatory disease, sexually transmitted disease, intrauterine device placement, and diethylstilbestrol (DES) exposure. None of these were significantly associated with risk of EP.
“Our model can be translated into an easy-to-use risk stratification tool that can accurately predict the risk of EP,” said Dr. Makhijani and her coauthors. “This tool could potentially be used by clinicians and ob.gyn. residencies nationally as [pregnancies of unknown location] are a very common management scenario.”
Dr. Makhijani reported having no disclosures and no outside sources of funding.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN ANTONIO – An easy-to-use risk stratification tool accurately predicted which pregnancies of unknown location were ectopic pregnancies by using a model validated by retrospective chart review.
Reeva Makhijani, MD, and her colleagues built the tool using a composite of risk factors to create a “generalized additive model,” or GAM, in combination with beta HCG levels. They presented the results during a poster session at the annual meeting of the American Society for Reproductive Medicine.
The model showed that a prior history of ectopic pregnancy (EP) (P = .0045), a history of pelvic surgery (P = .397), and a presentation of vaginal bleeding (P = .0003) all significantly increased the risk of EP.
Another statistical measure, the area under the receiver operating curve (AUC), helps estimate the likelihood of EP according to beta-HCG levels. When the initial beta-HCG was considered together with the ratio of the initial beta HCG to the presenting beta-HCG, the AUC was 0.889. For the initial beta-HCG level alone, the AUC was 0.793, while for the ratio alone, the AUC was 0.88. Higher AUC figures indicate more predictive power.
Dr. Makhijani, an ob.gyn. resident physician at Brown University, Providence, R.I., and her colleagues have built a prototype of a computer application that calculates risk of EP when the significant risk factors and lab values are entered.
After reviewing the electronic medical records of 800 patients who had pregnancies of unknown location (PUL), in the final analysis Dr. Makhijani and her coauthors included 398 patients whose medical histories allowed assessment of risk factors and whose record included at least two beta-HCG values taken 36-72 hours apart. The investigators also excluded patients with molar pregnancies, ruptured EPs, or who had undergone surgery before a second beta-HCG was obtained.
Of the 398 patients, 40 (10%) were eventually found to have EP, while 168 (42%) had an intrauterine pregnancy, and 190 (48%) were diagnosed with spontaneous abortion.
The patients were about 27 years old on average, and just over half (n = 224) were parous. Vaginal bleeding was a presenting sign in 233 patients, and 284 had abdominal pain. Of those with EP, 34 of 40 had vaginal bleeding, and 25 of 40 had abdominal pain.
In addition to the three factors found to have significant association with EP, the investigators initially considered a number of other patient characteristics, including age, parity, and presentation with abdominal pain. Additional risk factors examined included history of infertility, pelvic inflammatory disease, sexually transmitted disease, intrauterine device placement, and diethylstilbestrol (DES) exposure. None of these were significantly associated with risk of EP.
“Our model can be translated into an easy-to-use risk stratification tool that can accurately predict the risk of EP,” said Dr. Makhijani and her coauthors. “This tool could potentially be used by clinicians and ob.gyn. residencies nationally as [pregnancies of unknown location] are a very common management scenario.”
Dr. Makhijani reported having no disclosures and no outside sources of funding.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT ASRM 2017
Key clinical point:
Major finding: Incorporating initial and serial beta-HCGs yielded an AUC of 0.889 for predicting ectopic pregnancy.
Data source: A retrospective chart review of 398 patients with pregnancy of unknown location.
Disclosures: The presenter reported having no relevant disclosures and no outside sources of funding.
Universal paternal Rh screening is cost effective in IVF
SAN ANTONIO – Implementing universal paternal Rh screening would be a cost-effective safety strategy among patients receiving in vitro fertilization, according to a model that used up-to-date data and accounted for ethnic variations in the prevalence of the Rh (D) antibody.
Using a universal Rh screening strategy for semen donors to Rh (D) negative women undergoing in vitro fertilization would result in a cost savings of $11.01 per patient, or $1,120,000 per 100,000 Rh negative IVF pregnancies, according to Pietro Bortoletto, MD, and his coauthors. Their findings were presented during a poster session at the annual meeting of the American Society for Reproductive Medicine.
If paternal Rh factor status is unknown, vaginal bleeding during pregnancy prompts maternal administration of anti-D immune globulin if the mother is Rh (D) negative to prevent hemolytic disease of the fetus and newborn. However, wrote Dr. Bortoletto and his colleagues, “in the IVF population, where paternity status is presumed to be certain, the Rh (D) status of the male partner can be used to triage Rh (D) negative women to more appropriate administration of anti-D globulin.”
To see whether a universal paternal Rh screening strategy would be cost effective, Dr. Bortoletto, a resident physician in obstetrics and gynecology at Harvard Medical School and Brigham and Women’s Hospital, both in Boston, and his collaborators constructed a decision tree to estimate cost savings. The model compared a universal paternal-screening strategy for Rh (D) negative women undergoing IVF with the current standard of practice, which does not involve routine Rh (D) screening for the sperm donor.
In constructing the model, the investigators drew on published data showing that first trimester bleeding is more common in women who undergo IVF: It occurs in one-third of these women, compared with about 20% of the general pregnant population.
They also established probability estimates of pregnancy loss before 20 weeks, with and without first trimester bleeding (0.34 and 0.18, respectively); third trimester bleeding, with and without first trimester bleeding (0.05 and 0.02); and trauma in pregnancy (0.08). They estimated the overall probability of the pregnancy producing an Rh positive neonate at 0.62.
An additional factor that Dr. Bortoletto and his collaborators took into account was the variable prevalence of Rh factor by ethnicity; in the United States, it’s most common in white men and least common in Asian men, with intermediate prevalence in African American and Hispanic men.
When paternal ethnicity was included in the analysis, savings were greatest with white sperm donors, at $1,889,000 per 100,000 Rh negative IVF pregnancies. The lower prevalence of Rh factor in Asian men meant that the strategy was not cost effective in this population since it would cost a net $2,323,000 per 100,000 Rh negative IVF pregnancies.
“A targeted screening approach, by paternal ethnicity, may be a targeted strategy for cost reduction,” wrote Dr. Bortoletto and his colleagues.
Figures for cost estimates were drawn from data from the Centers for Medicare & Medicaid (CMS) using 2017 dollars. The cost for tests to determine blood type and Rh status ranged from $6 to $11, so the investigators set the cost estimate of $8.20. The cost for an antibody screen was estimated at $5.25 (range, $4-$7).
The cost for a 300 mcg dose of anti-D immune globulin was estimated at $93.93 (range, $79-$109), and administration costs were $27.04 (range, $25-$28). Kleihauer-Betke testing to determine the amount of fetal blood in maternal circulation was pinned at $10.61 (range, $8-$14).
Even when the lowest end of the cost range of anti-D immune globulin was used, a universal screening model would still realize a cost savings of $820,000 per 100,000 Rh negative IVF pregnancies. When Rh screening cost was set at $11 – at the high end of the range – “the strategy still remained favorable at $981,000,” wrote Dr. Bortoletto and his colleagues.
“Universal paternal Rh screening provides a cost saving intervention by preventing nonindicated and costly administration of anti-D immune globulin in the IVF population presenting with bleeding or trauma in pregnancy,” they wrote.
Dr. Bortoletto reported no outside sources of funding and no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN ANTONIO – Implementing universal paternal Rh screening would be a cost-effective safety strategy among patients receiving in vitro fertilization, according to a model that used up-to-date data and accounted for ethnic variations in the prevalence of the Rh (D) antibody.
Using a universal Rh screening strategy for semen donors to Rh (D) negative women undergoing in vitro fertilization would result in a cost savings of $11.01 per patient, or $1,120,000 per 100,000 Rh negative IVF pregnancies, according to Pietro Bortoletto, MD, and his coauthors. Their findings were presented during a poster session at the annual meeting of the American Society for Reproductive Medicine.
If paternal Rh factor status is unknown, vaginal bleeding during pregnancy prompts maternal administration of anti-D immune globulin if the mother is Rh (D) negative to prevent hemolytic disease of the fetus and newborn. However, wrote Dr. Bortoletto and his colleagues, “in the IVF population, where paternity status is presumed to be certain, the Rh (D) status of the male partner can be used to triage Rh (D) negative women to more appropriate administration of anti-D globulin.”
To see whether a universal paternal Rh screening strategy would be cost effective, Dr. Bortoletto, a resident physician in obstetrics and gynecology at Harvard Medical School and Brigham and Women’s Hospital, both in Boston, and his collaborators constructed a decision tree to estimate cost savings. The model compared a universal paternal-screening strategy for Rh (D) negative women undergoing IVF with the current standard of practice, which does not involve routine Rh (D) screening for the sperm donor.
In constructing the model, the investigators drew on published data showing that first trimester bleeding is more common in women who undergo IVF: It occurs in one-third of these women, compared with about 20% of the general pregnant population.
They also established probability estimates of pregnancy loss before 20 weeks, with and without first trimester bleeding (0.34 and 0.18, respectively); third trimester bleeding, with and without first trimester bleeding (0.05 and 0.02); and trauma in pregnancy (0.08). They estimated the overall probability of the pregnancy producing an Rh positive neonate at 0.62.
An additional factor that Dr. Bortoletto and his collaborators took into account was the variable prevalence of Rh factor by ethnicity; in the United States, it’s most common in white men and least common in Asian men, with intermediate prevalence in African American and Hispanic men.
When paternal ethnicity was included in the analysis, savings were greatest with white sperm donors, at $1,889,000 per 100,000 Rh negative IVF pregnancies. The lower prevalence of Rh factor in Asian men meant that the strategy was not cost effective in this population since it would cost a net $2,323,000 per 100,000 Rh negative IVF pregnancies.
“A targeted screening approach, by paternal ethnicity, may be a targeted strategy for cost reduction,” wrote Dr. Bortoletto and his colleagues.
Figures for cost estimates were drawn from data from the Centers for Medicare & Medicaid (CMS) using 2017 dollars. The cost for tests to determine blood type and Rh status ranged from $6 to $11, so the investigators set the cost estimate of $8.20. The cost for an antibody screen was estimated at $5.25 (range, $4-$7).
The cost for a 300 mcg dose of anti-D immune globulin was estimated at $93.93 (range, $79-$109), and administration costs were $27.04 (range, $25-$28). Kleihauer-Betke testing to determine the amount of fetal blood in maternal circulation was pinned at $10.61 (range, $8-$14).
Even when the lowest end of the cost range of anti-D immune globulin was used, a universal screening model would still realize a cost savings of $820,000 per 100,000 Rh negative IVF pregnancies. When Rh screening cost was set at $11 – at the high end of the range – “the strategy still remained favorable at $981,000,” wrote Dr. Bortoletto and his colleagues.
“Universal paternal Rh screening provides a cost saving intervention by preventing nonindicated and costly administration of anti-D immune globulin in the IVF population presenting with bleeding or trauma in pregnancy,” they wrote.
Dr. Bortoletto reported no outside sources of funding and no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN ANTONIO – Implementing universal paternal Rh screening would be a cost-effective safety strategy among patients receiving in vitro fertilization, according to a model that used up-to-date data and accounted for ethnic variations in the prevalence of the Rh (D) antibody.
Using a universal Rh screening strategy for semen donors to Rh (D) negative women undergoing in vitro fertilization would result in a cost savings of $11.01 per patient, or $1,120,000 per 100,000 Rh negative IVF pregnancies, according to Pietro Bortoletto, MD, and his coauthors. Their findings were presented during a poster session at the annual meeting of the American Society for Reproductive Medicine.
If paternal Rh factor status is unknown, vaginal bleeding during pregnancy prompts maternal administration of anti-D immune globulin if the mother is Rh (D) negative to prevent hemolytic disease of the fetus and newborn. However, wrote Dr. Bortoletto and his colleagues, “in the IVF population, where paternity status is presumed to be certain, the Rh (D) status of the male partner can be used to triage Rh (D) negative women to more appropriate administration of anti-D globulin.”
To see whether a universal paternal Rh screening strategy would be cost effective, Dr. Bortoletto, a resident physician in obstetrics and gynecology at Harvard Medical School and Brigham and Women’s Hospital, both in Boston, and his collaborators constructed a decision tree to estimate cost savings. The model compared a universal paternal-screening strategy for Rh (D) negative women undergoing IVF with the current standard of practice, which does not involve routine Rh (D) screening for the sperm donor.
In constructing the model, the investigators drew on published data showing that first trimester bleeding is more common in women who undergo IVF: It occurs in one-third of these women, compared with about 20% of the general pregnant population.
They also established probability estimates of pregnancy loss before 20 weeks, with and without first trimester bleeding (0.34 and 0.18, respectively); third trimester bleeding, with and without first trimester bleeding (0.05 and 0.02); and trauma in pregnancy (0.08). They estimated the overall probability of the pregnancy producing an Rh positive neonate at 0.62.
An additional factor that Dr. Bortoletto and his collaborators took into account was the variable prevalence of Rh factor by ethnicity; in the United States, it’s most common in white men and least common in Asian men, with intermediate prevalence in African American and Hispanic men.
When paternal ethnicity was included in the analysis, savings were greatest with white sperm donors, at $1,889,000 per 100,000 Rh negative IVF pregnancies. The lower prevalence of Rh factor in Asian men meant that the strategy was not cost effective in this population since it would cost a net $2,323,000 per 100,000 Rh negative IVF pregnancies.
“A targeted screening approach, by paternal ethnicity, may be a targeted strategy for cost reduction,” wrote Dr. Bortoletto and his colleagues.
Figures for cost estimates were drawn from data from the Centers for Medicare & Medicaid (CMS) using 2017 dollars. The cost for tests to determine blood type and Rh status ranged from $6 to $11, so the investigators set the cost estimate of $8.20. The cost for an antibody screen was estimated at $5.25 (range, $4-$7).
The cost for a 300 mcg dose of anti-D immune globulin was estimated at $93.93 (range, $79-$109), and administration costs were $27.04 (range, $25-$28). Kleihauer-Betke testing to determine the amount of fetal blood in maternal circulation was pinned at $10.61 (range, $8-$14).
Even when the lowest end of the cost range of anti-D immune globulin was used, a universal screening model would still realize a cost savings of $820,000 per 100,000 Rh negative IVF pregnancies. When Rh screening cost was set at $11 – at the high end of the range – “the strategy still remained favorable at $981,000,” wrote Dr. Bortoletto and his colleagues.
“Universal paternal Rh screening provides a cost saving intervention by preventing nonindicated and costly administration of anti-D immune globulin in the IVF population presenting with bleeding or trauma in pregnancy,” they wrote.
Dr. Bortoletto reported no outside sources of funding and no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
At ASRM 2017
Key clinical point:
Major finding: Universal screening would save $1,120,000 per 100,000 Rh negative IVF pregnancies.
Data source: Decision tree incorporating Rh (D) prevalence, bleeding risk, and cost data.
Disclosures: Dr. Bortoletto reported having no relevant disclosures and no outside funding.
Young female hematologic cancer survivors have increased infertility risk
SAN ANTONIO – Young women who were survivors of hematologic cancer were more likely to have a diagnosis of infertility than cancer-free women, according to a large population-based study.
Using Ontario, Canada, universal health care databases, Maria Velez, MD, and her colleagues compared young female hematologic cancer survivors with age-matched women who were cancer-free, finding that 20.4% of the cancer survivors and 15% of the cancer-free women had an infertility diagnosis (P less than .001).
The matched cohort study used the Ontario Cancer Registry and identified 1,226 women aged 16-34 years who had been recurrence free for at least 5 years after a hematologic malignancy such that it captured cancer diagnoses made between 1992 and 2005. Each of these women was matched with four randomly selected, cancer-free women (n = 4,293) by the investigators, who took each woman’s age, location and socioeconomic status into account.
Then, the Ontario Health Insurance Plan database was queried to see which women in each group had claims billed under a diagnosis of infertility, denoted by ICD-9 code 628. Dr. Velez said that, for the survivor group, the investigators began tallying infertility diagnoses a full year after treatment was completed.
Pooling all types of hematologic cancer and adjusting for socioeconomic status, the overall relative risk for infertility was 1.35 for hematologic cancer survivors (95% confidence interval, 1.19-1.54; P less than .001).*
Dr. Velez and her colleagues also compared relative risk by type of hematologic cancer. The relative risk for infertility was 1.35 for survivors of non-Hodgkin lymphoma (n = 371); 1.30 for Hodgkin lymphoma (n = 731); and 1.71 for leukemia (n = 124). These were all statistically significant elevations in RR.
In the survivor group, the mean age at cancer diagnosis was 25.7 years, and patients were followed for a median 16.2 years. The mean age of infertility diagnosis for cancer survivors – 33 years – was not significantly different from that of the cancer-free group (32.8 years).
Dr. Velez and her colleagues also examined whether parity at the time of diagnosis was a factor. Cancer survivors who were nulliparous had a pooled relative risk of 1.35 for infertility, compared with the cancer-free women (P less than .001)*. A significantly elevated relative risk was seen for each individual cancer, except for leukemia. Dr. Velez said that this was likely a statistical artifact of the relatively small number of women who had this diagnosis.
The relative risk of an infertility diagnosis for women who were parous at the time of diagnosis was 1.21, a nonsignificant difference (95% CI, 0.80-1.83; P = .37). No individual diagnosis in this group carried a significantly elevated relative risk for infertility.
It’s difficult to know why parity might make a difference in risk of an infertility diagnosis, Dr. Velez said. There might be “nonbiologic” reasons, such as a difference in motivation to seek care for infertility or in desire for pregnancy, she said.
Strengths of the study included the large sample size and the population-based cohort design. The study was the first to use the ICD-9 code of infertility in cancer research, Dr. Velez said. Also, the relatively recent study period meant that patients received more modern cancer treatment regimens, making the data more relevant than some older Scandinavian studies that reached back into the 1960s, said Dr. Velez of the department of obstetrics and gynecology, in the division of reproductive endocrinology and infertility at Queen’s University, Kingston, Ont.
The study did not track the treatment regimen patients received, so it does not shed light on which chemotherapy regimens might be less gonadotoxic over time. The results are a call to include “the effect of cancer treatment on ovarian reserve as a secondary outcome” in clinical trials for cancer therapies, Dr. Velez said.
The study was conducted through the Institute for Clinical Evaluative Sciences and funded by the Faculty of Health Sciences at Queen's University. Dr. Velez reported that she has no financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
*Correction 11/14/17: An earlier version of this article misstated the P values.
SAN ANTONIO – Young women who were survivors of hematologic cancer were more likely to have a diagnosis of infertility than cancer-free women, according to a large population-based study.
Using Ontario, Canada, universal health care databases, Maria Velez, MD, and her colleagues compared young female hematologic cancer survivors with age-matched women who were cancer-free, finding that 20.4% of the cancer survivors and 15% of the cancer-free women had an infertility diagnosis (P less than .001).
The matched cohort study used the Ontario Cancer Registry and identified 1,226 women aged 16-34 years who had been recurrence free for at least 5 years after a hematologic malignancy such that it captured cancer diagnoses made between 1992 and 2005. Each of these women was matched with four randomly selected, cancer-free women (n = 4,293) by the investigators, who took each woman’s age, location and socioeconomic status into account.
Then, the Ontario Health Insurance Plan database was queried to see which women in each group had claims billed under a diagnosis of infertility, denoted by ICD-9 code 628. Dr. Velez said that, for the survivor group, the investigators began tallying infertility diagnoses a full year after treatment was completed.
Pooling all types of hematologic cancer and adjusting for socioeconomic status, the overall relative risk for infertility was 1.35 for hematologic cancer survivors (95% confidence interval, 1.19-1.54; P less than .001).*
Dr. Velez and her colleagues also compared relative risk by type of hematologic cancer. The relative risk for infertility was 1.35 for survivors of non-Hodgkin lymphoma (n = 371); 1.30 for Hodgkin lymphoma (n = 731); and 1.71 for leukemia (n = 124). These were all statistically significant elevations in RR.
In the survivor group, the mean age at cancer diagnosis was 25.7 years, and patients were followed for a median 16.2 years. The mean age of infertility diagnosis for cancer survivors – 33 years – was not significantly different from that of the cancer-free group (32.8 years).
Dr. Velez and her colleagues also examined whether parity at the time of diagnosis was a factor. Cancer survivors who were nulliparous had a pooled relative risk of 1.35 for infertility, compared with the cancer-free women (P less than .001)*. A significantly elevated relative risk was seen for each individual cancer, except for leukemia. Dr. Velez said that this was likely a statistical artifact of the relatively small number of women who had this diagnosis.
The relative risk of an infertility diagnosis for women who were parous at the time of diagnosis was 1.21, a nonsignificant difference (95% CI, 0.80-1.83; P = .37). No individual diagnosis in this group carried a significantly elevated relative risk for infertility.
It’s difficult to know why parity might make a difference in risk of an infertility diagnosis, Dr. Velez said. There might be “nonbiologic” reasons, such as a difference in motivation to seek care for infertility or in desire for pregnancy, she said.
Strengths of the study included the large sample size and the population-based cohort design. The study was the first to use the ICD-9 code of infertility in cancer research, Dr. Velez said. Also, the relatively recent study period meant that patients received more modern cancer treatment regimens, making the data more relevant than some older Scandinavian studies that reached back into the 1960s, said Dr. Velez of the department of obstetrics and gynecology, in the division of reproductive endocrinology and infertility at Queen’s University, Kingston, Ont.
The study did not track the treatment regimen patients received, so it does not shed light on which chemotherapy regimens might be less gonadotoxic over time. The results are a call to include “the effect of cancer treatment on ovarian reserve as a secondary outcome” in clinical trials for cancer therapies, Dr. Velez said.
The study was conducted through the Institute for Clinical Evaluative Sciences and funded by the Faculty of Health Sciences at Queen's University. Dr. Velez reported that she has no financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
*Correction 11/14/17: An earlier version of this article misstated the P values.
SAN ANTONIO – Young women who were survivors of hematologic cancer were more likely to have a diagnosis of infertility than cancer-free women, according to a large population-based study.
Using Ontario, Canada, universal health care databases, Maria Velez, MD, and her colleagues compared young female hematologic cancer survivors with age-matched women who were cancer-free, finding that 20.4% of the cancer survivors and 15% of the cancer-free women had an infertility diagnosis (P less than .001).
The matched cohort study used the Ontario Cancer Registry and identified 1,226 women aged 16-34 years who had been recurrence free for at least 5 years after a hematologic malignancy such that it captured cancer diagnoses made between 1992 and 2005. Each of these women was matched with four randomly selected, cancer-free women (n = 4,293) by the investigators, who took each woman’s age, location and socioeconomic status into account.
Then, the Ontario Health Insurance Plan database was queried to see which women in each group had claims billed under a diagnosis of infertility, denoted by ICD-9 code 628. Dr. Velez said that, for the survivor group, the investigators began tallying infertility diagnoses a full year after treatment was completed.
Pooling all types of hematologic cancer and adjusting for socioeconomic status, the overall relative risk for infertility was 1.35 for hematologic cancer survivors (95% confidence interval, 1.19-1.54; P less than .001).*
Dr. Velez and her colleagues also compared relative risk by type of hematologic cancer. The relative risk for infertility was 1.35 for survivors of non-Hodgkin lymphoma (n = 371); 1.30 for Hodgkin lymphoma (n = 731); and 1.71 for leukemia (n = 124). These were all statistically significant elevations in RR.
In the survivor group, the mean age at cancer diagnosis was 25.7 years, and patients were followed for a median 16.2 years. The mean age of infertility diagnosis for cancer survivors – 33 years – was not significantly different from that of the cancer-free group (32.8 years).
Dr. Velez and her colleagues also examined whether parity at the time of diagnosis was a factor. Cancer survivors who were nulliparous had a pooled relative risk of 1.35 for infertility, compared with the cancer-free women (P less than .001)*. A significantly elevated relative risk was seen for each individual cancer, except for leukemia. Dr. Velez said that this was likely a statistical artifact of the relatively small number of women who had this diagnosis.
The relative risk of an infertility diagnosis for women who were parous at the time of diagnosis was 1.21, a nonsignificant difference (95% CI, 0.80-1.83; P = .37). No individual diagnosis in this group carried a significantly elevated relative risk for infertility.
It’s difficult to know why parity might make a difference in risk of an infertility diagnosis, Dr. Velez said. There might be “nonbiologic” reasons, such as a difference in motivation to seek care for infertility or in desire for pregnancy, she said.
Strengths of the study included the large sample size and the population-based cohort design. The study was the first to use the ICD-9 code of infertility in cancer research, Dr. Velez said. Also, the relatively recent study period meant that patients received more modern cancer treatment regimens, making the data more relevant than some older Scandinavian studies that reached back into the 1960s, said Dr. Velez of the department of obstetrics and gynecology, in the division of reproductive endocrinology and infertility at Queen’s University, Kingston, Ont.
The study did not track the treatment regimen patients received, so it does not shed light on which chemotherapy regimens might be less gonadotoxic over time. The results are a call to include “the effect of cancer treatment on ovarian reserve as a secondary outcome” in clinical trials for cancer therapies, Dr. Velez said.
The study was conducted through the Institute for Clinical Evaluative Sciences and funded by the Faculty of Health Sciences at Queen's University. Dr. Velez reported that she has no financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
*Correction 11/14/17: An earlier version of this article misstated the P values.
AT ASRM 2017
Key clinical point:
Major finding: Young women who survived hematologic cancer had a 20.4% risk of infertility, compared with 15% among cancer-free controls (P less than .001). The overall relative risk for infertility among hematologic cancer survivors was 1.35.
Data source: Prospective, age-matched cohort study of 1,226 cancer survivors and 4,293 cancer-free controls.
Disclosures: Dr. Velez reported that she had no disclosures. The Institute for Clinical Evaluative Services in Toronto funded the study.
Are microRNAs the key to an endometriosis biomarker?
SAN ANTONIO – The results of a prospective study showed that, in patients without a surgical endometriosis diagnosis, a serum test of microRNA (miRNA) levels yielded a very high predictive value when endometriosis was later surgically confirmed.
“This is the first prospective study performed within a diverse population that identifies miRNAs can reliably be used to differentiate between endometriosis and other gynecologic pathologies,” Sarah Moustafa, MD, said at the annual meeting of the American Society for Reproductive Medicine.
Dr. Moustafa and her collaborators found that the area under the receiver operating characteristic curve (AUC) for the combination of miRNAs 125, 451, and 3613 was 0.917. The AUC of another combination was even higher: the miRNAs let-7b, 150, 342, and 451 yielded an AUC of 0.977 for endometriosis. These figures support that the miRNA combinations give “an excellent diagnostic potential for endometriosis,” Dr. Moustafa said.
The study enrolled 86 women of reproductive age who were scheduled to have a laparotomy or laparoscopy for benign gynecologic reasons. Pregnant patients and those with malignancy were excluded. Patients had blood drawn before their surgeries to have blinded miRNA analysis via quantitative reverse transcriptase polymerase chain reaction.
Dr. Moustafa and her colleagues looked at the diagnostic value of individual miRNAs and also examined combinations of promising miRNAs by seeing which levels were elevated or depressed in patients who were later found to have surgically diagnosed endometriosis. The study built on previous retrospective work that had identified some candidate miRNAs.
In this prospective study, women with endometriosis had significantly lower serum levels of miRNAs 3613 and let-7b and significantly higher serum levels of miRNAs 150, 125b, 451, and 342. The investigators also analyzed the data to see if there were miRNA level differences between women who were on hormones and those who were not, and also to see if cycle timing affected results; neither of these factors affected miRNA levels, Dr. Moustafa reported.
When the enrolled patients had surgery, 36 were found to have endometriosis and 50 had a variety of other diagnoses, with uterine fibroids (48%) and no abnormal pathology (28%) predominating.
“A noninvasive diagnostic test does not currently exist” but is sorely needed, Dr. Moustafa said.
There’s a long gap from the onset of endometriosis symptoms to diagnosis, with one study showing that symptoms can be present for an average of 6.7-11 years before surgical diagnosis occurs. In one survey of more than 7,000 women, nearly half (46%) saw more than five physicians before they got the correct diagnosis, said Dr. Moustafa, a resident in the obstetrics, gynecology, and reproductive sciences department at Yale University, New Haven, Conn.
In a discussion following the presentation, attendee Steve Young, MD, PhD, professor of reproductive endocrinology and fertility at the University of North Carolina, Chapel Hill, said it would be useful to have a biomarker that could be a surrogate for disease burden. “You could look at miRNAs after surgery. Do you see changes back toward normal?” Dr. Young said.
Dr. Moustafa responded that the research team is in the process of collecting postoperative data to see whether levels change when the disease burden is diminished by surgery.
Next steps, she said, include looking for miRNAs in saliva to explore whether an even less invasive test might be possible. Also, there are suggestions that miRNA 125 might be a marker for more severe disease, so the team is investigating this association as well.
Whether the combination miRNA screen is ready for prime time is still an open question, she said. “Any time a new screening test is developed we have to have caution.” Current thinking, she said, points toward the utility of miRNA screening for patients with unexplained fertility, for example.
“At this point, the pendulum is so far on the side of underdiagnosis that we think patients would benefit from a screening test,” Dr. Moustafa added.
The study was supported by OvaScience. Dr. Moustafa reported having no relevant financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN ANTONIO – The results of a prospective study showed that, in patients without a surgical endometriosis diagnosis, a serum test of microRNA (miRNA) levels yielded a very high predictive value when endometriosis was later surgically confirmed.
“This is the first prospective study performed within a diverse population that identifies miRNAs can reliably be used to differentiate between endometriosis and other gynecologic pathologies,” Sarah Moustafa, MD, said at the annual meeting of the American Society for Reproductive Medicine.
Dr. Moustafa and her collaborators found that the area under the receiver operating characteristic curve (AUC) for the combination of miRNAs 125, 451, and 3613 was 0.917. The AUC of another combination was even higher: the miRNAs let-7b, 150, 342, and 451 yielded an AUC of 0.977 for endometriosis. These figures support that the miRNA combinations give “an excellent diagnostic potential for endometriosis,” Dr. Moustafa said.
The study enrolled 86 women of reproductive age who were scheduled to have a laparotomy or laparoscopy for benign gynecologic reasons. Pregnant patients and those with malignancy were excluded. Patients had blood drawn before their surgeries to have blinded miRNA analysis via quantitative reverse transcriptase polymerase chain reaction.
Dr. Moustafa and her colleagues looked at the diagnostic value of individual miRNAs and also examined combinations of promising miRNAs by seeing which levels were elevated or depressed in patients who were later found to have surgically diagnosed endometriosis. The study built on previous retrospective work that had identified some candidate miRNAs.
In this prospective study, women with endometriosis had significantly lower serum levels of miRNAs 3613 and let-7b and significantly higher serum levels of miRNAs 150, 125b, 451, and 342. The investigators also analyzed the data to see if there were miRNA level differences between women who were on hormones and those who were not, and also to see if cycle timing affected results; neither of these factors affected miRNA levels, Dr. Moustafa reported.
When the enrolled patients had surgery, 36 were found to have endometriosis and 50 had a variety of other diagnoses, with uterine fibroids (48%) and no abnormal pathology (28%) predominating.
“A noninvasive diagnostic test does not currently exist” but is sorely needed, Dr. Moustafa said.
There’s a long gap from the onset of endometriosis symptoms to diagnosis, with one study showing that symptoms can be present for an average of 6.7-11 years before surgical diagnosis occurs. In one survey of more than 7,000 women, nearly half (46%) saw more than five physicians before they got the correct diagnosis, said Dr. Moustafa, a resident in the obstetrics, gynecology, and reproductive sciences department at Yale University, New Haven, Conn.
In a discussion following the presentation, attendee Steve Young, MD, PhD, professor of reproductive endocrinology and fertility at the University of North Carolina, Chapel Hill, said it would be useful to have a biomarker that could be a surrogate for disease burden. “You could look at miRNAs after surgery. Do you see changes back toward normal?” Dr. Young said.
Dr. Moustafa responded that the research team is in the process of collecting postoperative data to see whether levels change when the disease burden is diminished by surgery.
Next steps, she said, include looking for miRNAs in saliva to explore whether an even less invasive test might be possible. Also, there are suggestions that miRNA 125 might be a marker for more severe disease, so the team is investigating this association as well.
Whether the combination miRNA screen is ready for prime time is still an open question, she said. “Any time a new screening test is developed we have to have caution.” Current thinking, she said, points toward the utility of miRNA screening for patients with unexplained fertility, for example.
“At this point, the pendulum is so far on the side of underdiagnosis that we think patients would benefit from a screening test,” Dr. Moustafa added.
The study was supported by OvaScience. Dr. Moustafa reported having no relevant financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN ANTONIO – The results of a prospective study showed that, in patients without a surgical endometriosis diagnosis, a serum test of microRNA (miRNA) levels yielded a very high predictive value when endometriosis was later surgically confirmed.
“This is the first prospective study performed within a diverse population that identifies miRNAs can reliably be used to differentiate between endometriosis and other gynecologic pathologies,” Sarah Moustafa, MD, said at the annual meeting of the American Society for Reproductive Medicine.
Dr. Moustafa and her collaborators found that the area under the receiver operating characteristic curve (AUC) for the combination of miRNAs 125, 451, and 3613 was 0.917. The AUC of another combination was even higher: the miRNAs let-7b, 150, 342, and 451 yielded an AUC of 0.977 for endometriosis. These figures support that the miRNA combinations give “an excellent diagnostic potential for endometriosis,” Dr. Moustafa said.
The study enrolled 86 women of reproductive age who were scheduled to have a laparotomy or laparoscopy for benign gynecologic reasons. Pregnant patients and those with malignancy were excluded. Patients had blood drawn before their surgeries to have blinded miRNA analysis via quantitative reverse transcriptase polymerase chain reaction.
Dr. Moustafa and her colleagues looked at the diagnostic value of individual miRNAs and also examined combinations of promising miRNAs by seeing which levels were elevated or depressed in patients who were later found to have surgically diagnosed endometriosis. The study built on previous retrospective work that had identified some candidate miRNAs.
In this prospective study, women with endometriosis had significantly lower serum levels of miRNAs 3613 and let-7b and significantly higher serum levels of miRNAs 150, 125b, 451, and 342. The investigators also analyzed the data to see if there were miRNA level differences between women who were on hormones and those who were not, and also to see if cycle timing affected results; neither of these factors affected miRNA levels, Dr. Moustafa reported.
When the enrolled patients had surgery, 36 were found to have endometriosis and 50 had a variety of other diagnoses, with uterine fibroids (48%) and no abnormal pathology (28%) predominating.
“A noninvasive diagnostic test does not currently exist” but is sorely needed, Dr. Moustafa said.
There’s a long gap from the onset of endometriosis symptoms to diagnosis, with one study showing that symptoms can be present for an average of 6.7-11 years before surgical diagnosis occurs. In one survey of more than 7,000 women, nearly half (46%) saw more than five physicians before they got the correct diagnosis, said Dr. Moustafa, a resident in the obstetrics, gynecology, and reproductive sciences department at Yale University, New Haven, Conn.
In a discussion following the presentation, attendee Steve Young, MD, PhD, professor of reproductive endocrinology and fertility at the University of North Carolina, Chapel Hill, said it would be useful to have a biomarker that could be a surrogate for disease burden. “You could look at miRNAs after surgery. Do you see changes back toward normal?” Dr. Young said.
Dr. Moustafa responded that the research team is in the process of collecting postoperative data to see whether levels change when the disease burden is diminished by surgery.
Next steps, she said, include looking for miRNAs in saliva to explore whether an even less invasive test might be possible. Also, there are suggestions that miRNA 125 might be a marker for more severe disease, so the team is investigating this association as well.
Whether the combination miRNA screen is ready for prime time is still an open question, she said. “Any time a new screening test is developed we have to have caution.” Current thinking, she said, points toward the utility of miRNA screening for patients with unexplained fertility, for example.
“At this point, the pendulum is so far on the side of underdiagnosis that we think patients would benefit from a screening test,” Dr. Moustafa added.
The study was supported by OvaScience. Dr. Moustafa reported having no relevant financial disclosures.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT ASRM 2017
Key clinical point:
Major finding: The areas under the receiver operating curve for the most promising miRNA combinations were 0.917 and 0.977.
Data source: Blinded, prospective study of 86 women slated to have diagnostic pelvic laparoscopy or laparotomy.
Disclosures: Dr. Moustafa reported no relevant disclosures. OvaScience supported the study.
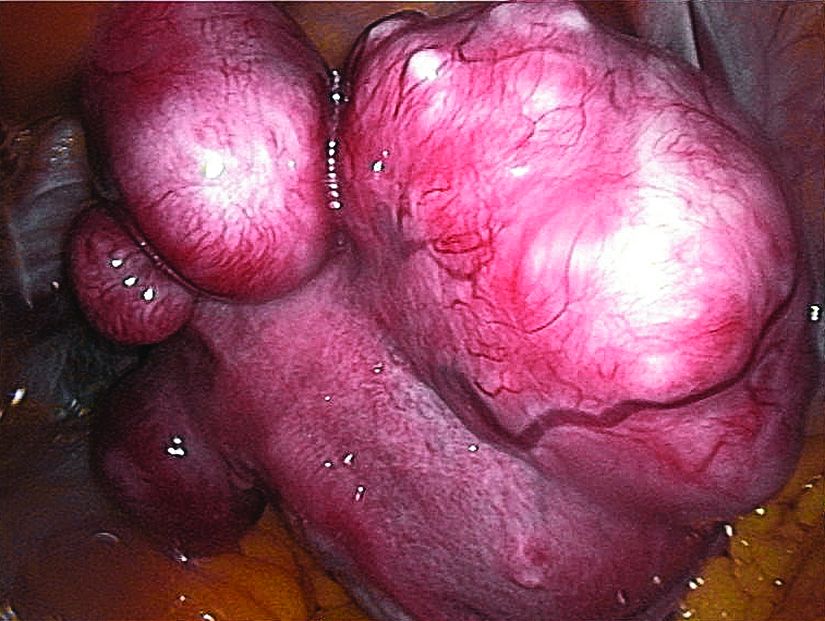
Ulipristal acetate reduced bleeding for women with fibroids
SAN ANTONIO – About half of women with uterine fibroids became amenorrheic when taking the selective progesterone receptor modulator ulipristal acetate (UPA) during a 12-week study cycle, and women taking UPA experienced significant improvement of quality of life, compared with those taking placebo.
Of those women taking 5 mg of UPA, 40.5%-42% became amenorrheic; of those taking 10 mg, 54.8%-57.3% became amenorrheic, James Liu, MD, reported at the annual meeting of the American Society for Reproductive Medicine. These results compared to amenorrhea rates of 0%-8% for women on placebo (P less than .0001 for all values).
The primary aim of VENUS II was to evaluate UPA’s efficacy and safety as intermittent treatment of abnormal uterine bleeding associated with uterine fibroids. Patients received UPA at either 5 mg or 10 mg orally. Secondary efficacy measures included the maintenance effect of UPA at both doses when compared to placebo, by assessing the rate of amenorrhea and the time to amenorrhea. Another secondary measure assessed uterine fibroid–related quality of life.
Safety was assessed by tracking adverse events through both courses of treatment. The study was not powered to compare the two doses against each other, but rather compared each against placebo.
Altogether, 432 patients were randomized to one of the treatment arms, which was begun after an initial screening period of about 10-12 weeks. The first treatment course lasted 12 weeks, after which patients went off treatment for two menstrual cycles. They then began another treatment course for 12 weeks and were followed for an additional 12 weeks after treatment was stopped.
Patients were included if they were premenopausal, aged 18-50 years old, had prolonged bleeding in at least 4 of the last 6 menstrual periods, had menstrual blood loss of at least 80 mL by cycle by the alkaline hematin method, and had at least one discrete leiomyoma without a uterine size greater than 20 weeks. About two-thirds of patients were black, reflecting the higher prevalence of uterine fibroids in this population, said Dr. Liu, professor of medicine and reproductive biology at Case Western Reserve University, Cleveland.
Most patients (60%-80%) had their bleeding controlled on either dose of UPA, compared with fewer than 10% of women taking placebo.
Quality of life data, presented separately at ASRM by Lee Shulman, MD, examined the impact of treatment on patients’ physical and social activities, and also on the severity of symptoms and health-related quality of life.
“The majority of patients on UPA versus a minority of patients on placebo described their menstrual/vaginal bleeding at the end of treatment course 1 as ‘much better’ or ‘very much better,’ ” said Dr. Shulman, chief of clinical genetics in the department of ob.gyn. at Northwestern University in Evanston, Ill.
Of patients taking 5 mg UPA, 75% reported that degree of improvement, as did 87% of those on 10 mg UPA, compared with 17.9% of those taking placebo. .
Adverse events were rare, with hot flashes occurring in about 10% of women taking UPA, compared with less than 2% of those taking placebo. Headaches, fatigue, and nausea were also reported, but rates were not significantly different from rates for those taking placebo. One serious adverse event that was deemed treatment related was a uterine hemorrhage experienced by a woman taking UPA.
“Even in treatment course 1 we already had profound and statistically significant effects in symptoms across the board,” Dr. Shulman said. “How long will they last? We obviously need more data. But the study suggests that the benefits last significantly longer than that associated with leuprolide acetate.”
Ulipristal acetate is already approved by the Food and Drug Administration at a different dosage as emergency contraception. The VENUS II data support its use for women with uterine fibroids, the researchers said. “Our results provide reassurance,” Dr. Liu said. “We can conclude that UPA is effective and safe in the management of uterine fibroids in the U.S. population.”
Dr. Liu reported that he had no relevant disclosures. Dr. Shulman reported relationships with multiple pharmaceutical companies, including Allergan, which funded the VENUS II study.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN ANTONIO – About half of women with uterine fibroids became amenorrheic when taking the selective progesterone receptor modulator ulipristal acetate (UPA) during a 12-week study cycle, and women taking UPA experienced significant improvement of quality of life, compared with those taking placebo.
Of those women taking 5 mg of UPA, 40.5%-42% became amenorrheic; of those taking 10 mg, 54.8%-57.3% became amenorrheic, James Liu, MD, reported at the annual meeting of the American Society for Reproductive Medicine. These results compared to amenorrhea rates of 0%-8% for women on placebo (P less than .0001 for all values).
The primary aim of VENUS II was to evaluate UPA’s efficacy and safety as intermittent treatment of abnormal uterine bleeding associated with uterine fibroids. Patients received UPA at either 5 mg or 10 mg orally. Secondary efficacy measures included the maintenance effect of UPA at both doses when compared to placebo, by assessing the rate of amenorrhea and the time to amenorrhea. Another secondary measure assessed uterine fibroid–related quality of life.
Safety was assessed by tracking adverse events through both courses of treatment. The study was not powered to compare the two doses against each other, but rather compared each against placebo.
Altogether, 432 patients were randomized to one of the treatment arms, which was begun after an initial screening period of about 10-12 weeks. The first treatment course lasted 12 weeks, after which patients went off treatment for two menstrual cycles. They then began another treatment course for 12 weeks and were followed for an additional 12 weeks after treatment was stopped.
Patients were included if they were premenopausal, aged 18-50 years old, had prolonged bleeding in at least 4 of the last 6 menstrual periods, had menstrual blood loss of at least 80 mL by cycle by the alkaline hematin method, and had at least one discrete leiomyoma without a uterine size greater than 20 weeks. About two-thirds of patients were black, reflecting the higher prevalence of uterine fibroids in this population, said Dr. Liu, professor of medicine and reproductive biology at Case Western Reserve University, Cleveland.
Most patients (60%-80%) had their bleeding controlled on either dose of UPA, compared with fewer than 10% of women taking placebo.
Quality of life data, presented separately at ASRM by Lee Shulman, MD, examined the impact of treatment on patients’ physical and social activities, and also on the severity of symptoms and health-related quality of life.
“The majority of patients on UPA versus a minority of patients on placebo described their menstrual/vaginal bleeding at the end of treatment course 1 as ‘much better’ or ‘very much better,’ ” said Dr. Shulman, chief of clinical genetics in the department of ob.gyn. at Northwestern University in Evanston, Ill.
Of patients taking 5 mg UPA, 75% reported that degree of improvement, as did 87% of those on 10 mg UPA, compared with 17.9% of those taking placebo. .
Adverse events were rare, with hot flashes occurring in about 10% of women taking UPA, compared with less than 2% of those taking placebo. Headaches, fatigue, and nausea were also reported, but rates were not significantly different from rates for those taking placebo. One serious adverse event that was deemed treatment related was a uterine hemorrhage experienced by a woman taking UPA.
“Even in treatment course 1 we already had profound and statistically significant effects in symptoms across the board,” Dr. Shulman said. “How long will they last? We obviously need more data. But the study suggests that the benefits last significantly longer than that associated with leuprolide acetate.”
Ulipristal acetate is already approved by the Food and Drug Administration at a different dosage as emergency contraception. The VENUS II data support its use for women with uterine fibroids, the researchers said. “Our results provide reassurance,” Dr. Liu said. “We can conclude that UPA is effective and safe in the management of uterine fibroids in the U.S. population.”
Dr. Liu reported that he had no relevant disclosures. Dr. Shulman reported relationships with multiple pharmaceutical companies, including Allergan, which funded the VENUS II study.
koakes@frontlinemedcom.com
On Twitter @karioakes
SAN ANTONIO – About half of women with uterine fibroids became amenorrheic when taking the selective progesterone receptor modulator ulipristal acetate (UPA) during a 12-week study cycle, and women taking UPA experienced significant improvement of quality of life, compared with those taking placebo.
Of those women taking 5 mg of UPA, 40.5%-42% became amenorrheic; of those taking 10 mg, 54.8%-57.3% became amenorrheic, James Liu, MD, reported at the annual meeting of the American Society for Reproductive Medicine. These results compared to amenorrhea rates of 0%-8% for women on placebo (P less than .0001 for all values).
The primary aim of VENUS II was to evaluate UPA’s efficacy and safety as intermittent treatment of abnormal uterine bleeding associated with uterine fibroids. Patients received UPA at either 5 mg or 10 mg orally. Secondary efficacy measures included the maintenance effect of UPA at both doses when compared to placebo, by assessing the rate of amenorrhea and the time to amenorrhea. Another secondary measure assessed uterine fibroid–related quality of life.
Safety was assessed by tracking adverse events through both courses of treatment. The study was not powered to compare the two doses against each other, but rather compared each against placebo.
Altogether, 432 patients were randomized to one of the treatment arms, which was begun after an initial screening period of about 10-12 weeks. The first treatment course lasted 12 weeks, after which patients went off treatment for two menstrual cycles. They then began another treatment course for 12 weeks and were followed for an additional 12 weeks after treatment was stopped.
Patients were included if they were premenopausal, aged 18-50 years old, had prolonged bleeding in at least 4 of the last 6 menstrual periods, had menstrual blood loss of at least 80 mL by cycle by the alkaline hematin method, and had at least one discrete leiomyoma without a uterine size greater than 20 weeks. About two-thirds of patients were black, reflecting the higher prevalence of uterine fibroids in this population, said Dr. Liu, professor of medicine and reproductive biology at Case Western Reserve University, Cleveland.
Most patients (60%-80%) had their bleeding controlled on either dose of UPA, compared with fewer than 10% of women taking placebo.
Quality of life data, presented separately at ASRM by Lee Shulman, MD, examined the impact of treatment on patients’ physical and social activities, and also on the severity of symptoms and health-related quality of life.
“The majority of patients on UPA versus a minority of patients on placebo described their menstrual/vaginal bleeding at the end of treatment course 1 as ‘much better’ or ‘very much better,’ ” said Dr. Shulman, chief of clinical genetics in the department of ob.gyn. at Northwestern University in Evanston, Ill.
Of patients taking 5 mg UPA, 75% reported that degree of improvement, as did 87% of those on 10 mg UPA, compared with 17.9% of those taking placebo. .
Adverse events were rare, with hot flashes occurring in about 10% of women taking UPA, compared with less than 2% of those taking placebo. Headaches, fatigue, and nausea were also reported, but rates were not significantly different from rates for those taking placebo. One serious adverse event that was deemed treatment related was a uterine hemorrhage experienced by a woman taking UPA.
“Even in treatment course 1 we already had profound and statistically significant effects in symptoms across the board,” Dr. Shulman said. “How long will they last? We obviously need more data. But the study suggests that the benefits last significantly longer than that associated with leuprolide acetate.”
Ulipristal acetate is already approved by the Food and Drug Administration at a different dosage as emergency contraception. The VENUS II data support its use for women with uterine fibroids, the researchers said. “Our results provide reassurance,” Dr. Liu said. “We can conclude that UPA is effective and safe in the management of uterine fibroids in the U.S. population.”
Dr. Liu reported that he had no relevant disclosures. Dr. Shulman reported relationships with multiple pharmaceutical companies, including Allergan, which funded the VENUS II study.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT ASRM 2017
Key clinical point:
Major finding: Between 40.5% and 57.3% of women taking ulipristal acetate (UPA) achieved amenorrhea, compared with 0%-8% of women on placebo (P less than .0001).
Data source: Venus II, a phase 3 prospective, randomized, double-blind, double-dummy, placebo-controlled study that was partially parallel and partially crossover, with 432 patients.
Disclosures: Dr. Liu reported no relevant disclosures; Dr. Shulman reported financial relationships with multiple pharmaceutical companies, including Allergan, which funded the trial.