A compromise
Under pressure from Dr. Saper and others, UCNS compromised by endorsing 10-year diplomates until the 5-year mark.
Alan Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles, and the editor-in-chief of Neurology Reviews, was among those who spoke up, only to see the duration of his certification cut in half.
“UCNS obviously realized that they had been wrong,” Dr. Rapoport said, referring to the compromise they made.
At the 5-year mark, physicians who didn’t adopt the new system were deleted from the UCNS online database, eliminating “the only way the public would know whether or not we were certified. This was after UCNS told us we would stay on the list with a note next to our name suggesting our certification was incomplete. They did not care that this might have hurt our reputations,” Dr. Rapoport said.
“To this day, no refunds, partial or full, have been given for the $1,800 we paid for the privilege of sitting for the exam, or for our time studying, or for the expenses accrued from canceling a day in the office and traveling to a testing center,” Dr. Rapoport said. “I did not want the money back; I wanted the certification promised to me. Since they have removed my name from this list, they do owe me the $1,800. They say they do not return their fees if you fail. How about if you pass and they remove you from their list?”
Yet he went on to make clear that the real issue is the principle of the matter. “This is not about money,” Dr. Rapoport said. “This is about what is fair and right.”
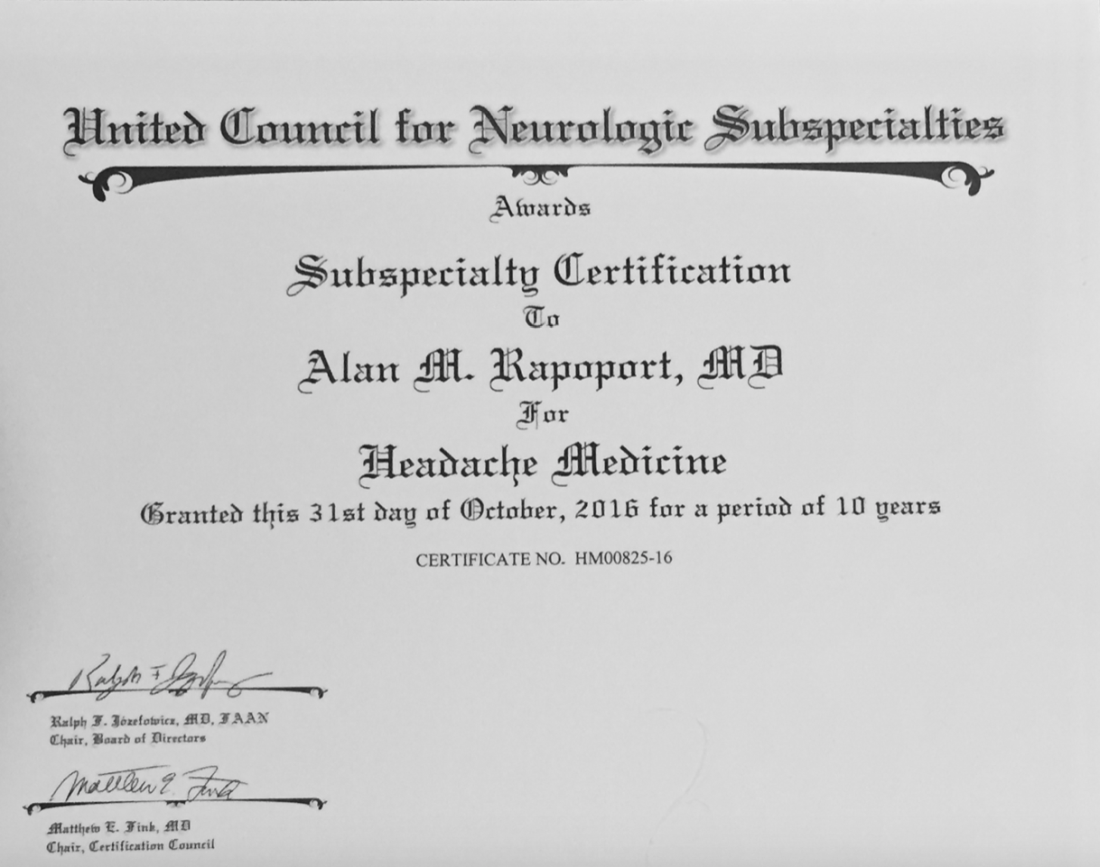
“The UCNS issued me a certificate for 10 years of certification in headache medicine; it is unethical and unlawful to break that contract and grant me only 5 years. Worse, they removed my name as though I do not exist. Along with Dr. Saper, I was one of the doctors that spent time and effort to advance headache medicine from October 1979, when I became a headache specialist, to today. I supported the principles of UCNS and took the first exam. I became the President of the International Headache Society and traveled the world promoting headache medicine; and this is how I am treated. Who can respect this type of certification, or this organization?”
Dr. Saper agreed: “It’s not about the money. It’s about the commitment. It’s very fraudulent.”
After the UCNS decision, Dr. Rapoport and Dr. Saper sought legal counsel, but ultimately decided not to sue the UCNS because of the lengthy process it would entail and the cost, estimated to be over $100,000.
“Our lawyers said: ‘It’s going to be years to get through it. You’ll probably win in the end, because it was fraudulent behavior,’ ” Dr. Saper said.
A different viewpoint
Ms. Riggott offered a different viewpoint: Nobody was guaranteed 10 years of certification.
“People do not pay for certification [from the UCNS],” Ms. Riggott said. “They pay to sit for an exam. It’s an exam administration fee. That can be construed as: ‘They paid for 10 years.’ They did not. They paid to sit for an exam. There are people who pay for an exam, and they don’t pass it, and they’re not certified. They don’t get a refund. That’s just the way high-stakes certification exams go.”
Dr. Saper and Dr. Rapoport see it differently. “The inherent reason any of us sit for an exam is to get certified.” Dr. Rapoport added. “Ms. Riggott is not being honest. There was an implied contract that if we passed, we would be granted a 10-year certification because that was what we did previously and that is what they told us would happen. Why would they have sent me this nice certificate for 10 more years of certification if she were telling the truth?”
Profits over promises
Dr. Rapoport estimates that many other neurologists had their certificates cut short and were dropped from this official list, some of them eminent members of the field, including David Watson, MD, professor and chair of neurology at West Virginia University Rockefeller Neuroscience Institute, Morgantown, and Robert Cowan, MD, professor of neurology and chief of the division of headache medicine at Stanford (Calif.) University.
“It is troubling when the organizations charged with maintaining the integrity of our specialization do not act with integrity,” Dr. Watson said. “The UCNS chose profits over promises and has refused to meaningfully engage with those of us whom they have wronged. What was once a point of pride for me (being in the second class of certified headache medicine diplomates) has become a meaningless piece of paper. This makes me sad.”
Dr. Cowan said the UCNS actions angered him while affirming his lifelong skepticism of clubs. “I was very sorry, but not surprised, to see the UCNS change the rules when the opportunity to make more money presented itself, and not surprised they did not honor their contracts. UCNS is just another scam like Best Doctors in the US and similar hypes. Neither are worth another dime of my money nor the time spent discussing them. One thing more: I have no quarrel with efforts to encourage keeping up with the field, although no one I know needs codification or direction as to which articles should be read. My outrage comes when responsible behavior is used as an excuse to line the pockets of dishonest, immoral individuals. I’m done.”
According to Ms. Riggott, the UCNS continuous certification process continues to evolve based on feedback from diplomates. She noted that “change is hard,” although the challenges of the transition appear to be paying off. “Initial retention for continuing certification is much higher than we would have expected from a high-stakes recertification exam,” she said. “So we are very, very happy about that.”
Proprietary tests drive revenue
According to Katie Collins, executive director of the National Board of Physicians and Surgeons, proprietary tests are a key revenue driver for medical boards, casting doubt on their educational motives.
“This isn’t really about maintaining their education, it’s really about having control over what they learn,” Ms. Collins said. “And unfortunately, physicians no longer have control over what they learn.”
NBPAS was formed largely in response to physicians dissatisfied with this situation. For $189 every 2 years, plus $25 for a paper certificate, NBPAS recertifies doctors originally credentialed by the American Board of Medical Specialties or the American Osteopathic Association.
Instead of making physicians take proprietary tests, NBPAS requires them to earn 50 hours of Accreditation Council for Continuing Medical Education–accredited CME every 2 years. Physicians can select where they seek this credit, giving them the agency to “pick and choose where they want to learn more,” Ms. Collins said, noting that this allows physicians to address personal knowledge gaps, instead of mastering the prescriptive lessons issued by other boards.
While this benefits physicians, Ms. Collins added, it also reduces the bottom line.
NBPAS is a “true 501(c)(3),” she said. “We have money for rainy days, but certainly not millions. We don’t have anything close to a million in savings.” Most medical boards are making millions on top of their services, she said. “That’s not for me to rein in, but it’s for me to point out.”
Noah Rosen, MD, associate professor of neurology and psychiatry at Northwell Health, Great Neck, N.Y., and former UCNS board member, said the UCNS was not motivated by money when they decided to switch to continuous recertification.
“The UCNS budget is publicly available,” Dr. Rosen said in an interview. “This is not a money-making organization,” he added, noting that the UCNS has “been basically operating on a breakeven budget,” and that certification “is not really a money-making proposition.”
Public IRS filings from 2019 and 2020 suggest a slightly different picture. In 2019, the UCNS reported net income of $72,256. In 2020, the inaugural year of the continuous certification program, net income jumped almost fivefold to $349,108. Over the same period, total assets held by the UCNS rose from $1.97 million to $2.37 million.
For comparison, NBPAS controls approximately $500,000 in total assets. The ABIM? Just shy of $72 million.