Recertification highlights a generational gap
Dr. Rosen, who was not a voting board member when the UCNS decided to switch to continuous certification, suggested that the transition could have been handled more effectively.
“I think Dr. Rapoport speaks to the frustration of how they made the transition, and that it could have been done in a way that recognizes people that held the certificate in a better way,” Dr. Rosen said.
He said that the departure of Dr. Rapoport and other neurologists from the UCNS points to another trend in the certification space. “I do think it brings up a deeper issue: What’s the value of certification? Dr. Rapoport and other people have brought up the question: What actually does this certificate bring you, if it’s not recognized by the federal government, and actually is not recognized by a lot of state governments, as well, as an official certification?”
He said the answer could depend on age.
“There seems to be a difference between younger people entering into the field and people that are more established in the field already,” Dr. Rosen said. “Younger people entering the field, they see certification as a distinction, something that separates them from the experiences and maybe every other neurologist.”
Ms. Collins independently pointed out the same generational gap. She noted that when the ABMS changed their maintenance model from lifelong to periodic in 2000, approximately 60% of their physicians had to change with the times, while the remainder did not.
“They grandfathered the other 40% – the older, probably more Caucasian male physicians,” she said. “It’s just the field. It’s evolved, it’s become more diverse. They created a divide in the physician community about what is the best means to maintain your board.”
In response to these comments, and despite his negative experiences with the UCNS, Dr. Rapoport emphasized that he still places high value on subspecialty certification.
“I care a lot about certification and that is why I decided to study for and take the only exam offered at the time,” he said, “I do not need it to continue my practice in headache medicine. No one asks me if I am certified in headache medicine. My patients are referred to me because of my reputation. But I have always sought the highest level of certification I could get. What UCNS has done is to cheapen the value of their certification.”
Dr. Rosen and Ms. Collins highlighted the other side of the same conclusion: For younger physicians, board certifications are more of a career consideration than they are for older physicians, as they could mean the difference between landing or losing a job.
“The American Board of Medical Specialties and [their] 24 member boards have really woven board certification into a requirement for employment for hospital privileges and for reimbursement,” Ms. Collins said.
And so, the practical value of board certification may depend most on the tenure of the person holding paper.
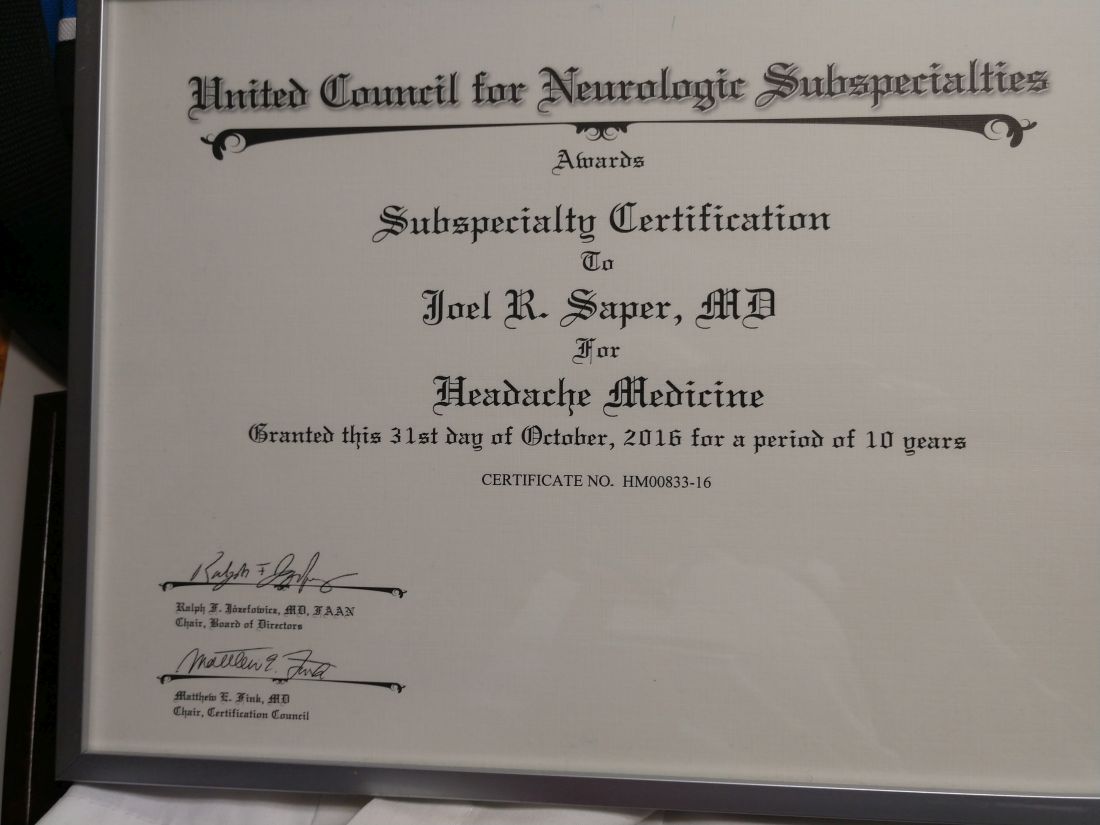
“I have not gone back to get any further certification [from the UCNS],” Dr. Saper said.
Even if his name has been removed from the UCNS register, he pointed out that his printed certificate still shows it’s valid until October 31st, 2026: “If anybody asks: ‘Are you certified?’ I say: ‘Here’s my certificate.’ ”