ECG Challenge

Man Shovels Path to Angina
While shoveling gravel several days ago, a 62-year-old man developed exertional angina. Though he stopped to rest, the pain persisted and radiated...
Lyle W. Larson, PhD, PA-C, is clinical faculty in the Department of Medicine, Division of Cardiology, Cardiac Electrophysiology, at the University of Washington, Seattle.
While playing in a company racquetball tournament, a 47-year-old man suddenly collapses. He is unresponsive, without a pulse, and his coworkers immediately initiate CPR. A single shock from an on-site AED successfully resuscitates him from ventricular fibrillation. Paramedics arrive within 12 minutes, by which time the patient is conscious and responsive to commands.
During transportation to the emergency department, however, he develops ventricular tachycardia and loses consciousness; a single shock cardioverts him to normal sinus rhythm. An ECG is ordered and the cardiac catheterization team mobilized.
While waiting, you contact the patient’s wife by telephone. She tells you that her husband has been complaining of chest discomfort for the past week and woke up two nights ago with what he described as “indigestion.” She says she suggested he see a clinician, and he agreed to do so—but not until after the tournament.
His medical history is remarkable only for chronic gastroesophageal reflux disease (GERD), for which he takes chewable antacids on a daily basis. He has no prior cardiac or pulmonary history. There is no surgical history apart from a tonsillectomy in childhood.
The patient is the Chief Operating Officer at a local manufacturing facility. He is married and has three children. His parents and grandparents are alive and in good health, aside from some arthritis in the older generation.
The review of systems, obtained from his wife, is noncontributory. She says he is in excellent health—he jogs, rides mountain bikes, and enjoys racquetball. Her husband attributed his recent chest discomfort to GERD; when she asked if it could be cardiac related, he adamantly denied the possibility, as he was in “excellent health” with “good genes.”
Vital signs include a blood pressure of 118/56 mm Hg; pulse, 80 beats/min; respiratory rate, 18 breaths/min-1; and O2 saturation, 100% on 2 L oxygen. He is afebrile.
Physical exam reveals a thin, otherwise healthy male who appears anxious and apprehensive. He denies ongoing chest pain but states that his chest wall is sore beneath the defibrillator pads. A focal exam reveals normal lung sounds and a regular rate and rhythm with no murmurs, gallops, or rubs. The abdomen is soft and nontender. All peripheral pulses are strong and equal bilaterally, and there are no focal neurologic signs.
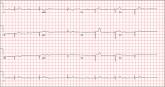
The ECG taken at admission shows a ventricular rate of 80 beats/min; PR interval, 162 ms; QRS duration, 106 ms; QT/QTc interval, 370/426 ms; P axis, 51°; R axis, –20°; and T axis, 70°. What is your interpretation of the ECG?
The correct interpretation includes normal sinus rhythm with a new anterior myocardial infarction (MI) and inferolateral injury.
Criteria for an anterior MI include Q waves in leads V 2 to V 6 and hyperacute ST-T wave changes. V 1 is usually spared.
Inferolateral injury is evidenced by the presence of Q waves and absence of R waves in leads III and aVF.
The patient’s cardiac catheterization revealed left anterior descending and circumflex artery disease.

While shoveling gravel several days ago, a 62-year-old man developed exertional angina. Though he stopped to rest, the pain persisted and radiated...

One week ago, a 67-year-old African-American woman with a history of diabetes, hypertension, and smoking developed a nonproductive cough and chest...
An 82-year-old man is referred from a nearby Alzheimer care facility following an episode of postural hypotension. While trying to get out of bed...
