ECG Challenge

Euphoric Man, Offbeat Rhythm
During a preoperative assessment, a 70-year-old man mentions that he has been experiencing irregular heart "thumping" for the past few months. See...
Lyle W. Larson, PhD, PA-C, is clinical faculty in the Department of Medicine, Division of Cardiology, Cardiac Electrophysiology, at the University of Washington, Seattle.
An active 74-year-old woman becomes nauseated and diaphoretic while cleaning up her church’s Sunday evening potluck. She shrugs it off, attributing it to something she ate, but while preparing to go home, she abruptly becomes short of breath and complains she can’t catch her breath. Two coworkers describe her appearance as pale with “complete loss of color” and insist on driving her to the local emergency department (ED).
When she arrives 10 minutes later, her shortness of breath is resolving. She denies chest pain, vomiting, and diarrhea. Despite receiving oxygen via nasal cannula, she still appears pale. An ECG and laboratory tests are ordered.
The patient’s medical history is remarkable for type 2 diabetes, hypothyroidism, obesity, and hypertension. Her surgical history is remarkable for a cholecystectomy and a hysterectomy 40 years ago, following the delivery of her third child.
The patient is a retired elementary school principal. She drinks alcohol socially and has never smoked. She lost her husband to colon cancer several years ago and now lives by herself in her home. She has three adult children who are all alive and well. Her mother died of heart failure, and her father was killed in an automobile accident.
Her current medication list includes metformin, levothyroxine, and hydrochlorothiazide. She states she has tried other medications for her diabetes and hypertension but prefers her current regimen. She is allergic to radiographic contrast media, with a documented near-anaphylactic reaction in the past.
Physical exam reveals a pleasant, cooperative, but apprehensive woman who appears her stated age. She wears corrective lenses and bilateral hearing aids. Her neck veins are not distended, and there is no evidence of thyromegaly. Respirations are rapid and shallow, with few crackles in both bases bilaterally but no rhonchi or rales. Her cardiac exam reveals a regular rate and rhythm with a soft, grade II, mid-systolic murmur at the left upper sternal border without radiation. There are no extra heart sounds or rubs. The abdomen is soft and nontender with well-healed surgical scars. The peripheral pulses are full and equal in both upper and lower extremities. The neurologic exam is grossly intact.
The review of systems shows that she has gained 14 pounds over the past four months, has been less physically active, and feels like she is “slowing down.” She also says her hearing and eyesight aren’t what they used to be, and she has chronic constipation. The remainder of her review of systems is unremarkable.
The patient’s weight is 218 lb and her height, 64 in. Vital signs include a blood pressure of 148/
110 mm Hg; pulse, 80 beats/min and regular; O2 saturation, 98% on 4 L O2 via nasal prongs; and respiratory rate, 20 breaths/min-1.
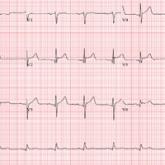
An ECG is obtained, and blood specimens for labwork—including a complete chemistry profile, complete blood count, thyroid function studies, and troponin levels—are collected. The ECG shows a ventricular rate of 80 beats/min; PR interval, 162 ms; QRS duration, 106 ms; QT/QTc intervals, 370/426 ms; P axis, 51°; R axis, –20°; and T axis, 70°. What is your interpretation of this ECG?
The correct interpretation includes normal sinus rhythm, acute ST elevation anterior myocardial infarction (STEMI), and inferolateral injury. Sinus rhythm is signified by a P wave for every QRS complex and a QRS complex for every P wave at a rate between 60 and 100 beats/min.
A STEMI is defined as new ST elevations at the J point in at least two contiguous leads—in women, 1.5 mm in leads V2 and V3 and 1 mm in all other leads; in men, 2 mm (those 40 and older) or 2.5 mm (those younger than 40) in leads V2 and V3 and 1 mm in all other leads. The anterior location is evidenced by the significant Q waves in leads I, V2, V3, and V4. T-wave inversions in these leads are absent due to the STEMI.
Inferolateral injury is identified by the Q waves in leads I, aVL, V5, and V6. Pseudo Q waves are seen in leads II, III, and aVF.
Troponin levels were significant for an acute myocardial infarction (MI). Cardiac cauterization confirmed an occlusion of the proximal left anterior descending coronary artery, and significant stenosis of the first obtuse marginal branch of the circumflex coronary artery. The patient’s lack of chest pain represents a common presentation of an MI in women, particularly those with a history of diabetes.

During a preoperative assessment, a 70-year-old man mentions that he has been experiencing irregular heart "thumping" for the past few months. See...
A company racquetball tournament takes a turn for the worse when this 47-year-old man suddenly collapses. Despite complaining of chest discomfort...

While shoveling gravel several days ago, a 62-year-old man developed exertional angina. Though he stopped to rest, the pain persisted and radiated...
