News
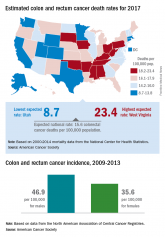
Colorectal cancer mortality highest in W.Va., lowest in Utah
More than 50,000 colorectal cancer deaths are expected in the United States for 2017, according to the American Cancer Society.
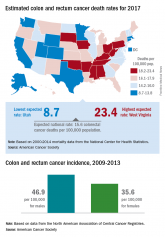
Colorectal cancer has been a “good news” story over the past 10-15 years. In the United States we have seen 30% reduction in both incidence and mortality over 10 years. This may be due to many factors, including increased rates of screening. The increased use of aspirin for cardiovascular protection, NSAIDs for joint and muscle pain, use of hormone replacement therapy, and reductions in smoking all likely contribute to the trend in CRC reduction.
Despite this good news, there is further evidence of rising incidence of CRC in individuals less than 54 years over the past 30 years. Rates of both colon and rectal cancer are increasing for 20 to 54-year-olds. This age group represent a small absolute risk of CRC, accounting for less than 10% of CRC, but the trend is disturbing and begs explanation. Obesity, diabetes, and metabolic syndrome are increasing in younger individuals, and these are potential risk factors for CRC.New or changing environmental exposures may place younger people at risk. The introduction of industrialized food in our diet over the past 4 decades could have both direct and indirect effects. It is possible that some food chemicals could be carcinogenic, but it is also quite possible that alteration of the microbiome by diet and environmental factors could lead to development of neoplasia in predisposed individuals. The use of antibiotics in our food chain may alter the microbiome.
There is considerable state-to-state variation in rates of CRC incidence and mortality. This is not new, but remains largely unexplained. The highest risk appears to be in the so-called “Rust Belt” and deep South, raising questions about environmental exposures that might predispose to CRC. Lower rates in states like Texas, Colorado, and California may be influenced by the population mix. There is evidence that Hispanics may have lower age-adjusted risk of CRC than blacks and Caucasians, so higher proportions of low-risk groups could impact the statewide risk of CRC. The differences between high-risk (West Virginia’s death rate of 23.4/100,000) and low-risk (Utah’s death rate 8.7/100,000) are too large to be explained by demographic differences alone, and strongly suggests an environmental culprit.
David Lieberman, MD, is professor of medicine; chief of the division of gastroenterology and hepatology, Oregon Health and Science University, Portland; and Vice President-elect of AGA.
FROM THE JOURNAL OF THE NATIONAL CANCER INSTITUTE
The proportion of rectal cancer cases diagnosed in people younger than 55 years doubled over the past 2 decades, according to a report published online Feb. 28 in the Journal of the National Cancer Institute.
In contrast, the proportion diagnosed in people older than 55 years has decreased over the last 4 decades, said Rebecca L. Siegel, MPH, strategic director of surveillance information services of surveillance and health services research at the American Cancer Society and her associates.
The study population comprised 490,305 patients.
The incidence of rectal cancer increased by 3.2% per year during the study period among patients aged 20-29 years and in those aged 30-39 years. It didn’t begin rising until the 1990s in adults aged 40-49 years and 50-54 years, and then it rose by a smaller amount – 2.3% per year. In contrast, the incidence of rectal cancer generally declined throughout the 40-year study period among adults aged 55 and older.
Because of these opposing trends, there was a net increase in rectal cancer of 4% per year for people in their twenties together with a net decrease of 2% per year for those aged 75 years and older.
The decreasing rate of rectal cancer in older adults “may partly reflect detection and removal of precancerous lesions during clinical inspection of the rectum, which was common practice well before formal colorectal cancer screening. Inherent differences within the colorectum in the way environmental factors initiate and or promote carcinogenesis, as well as the influence of unknown risk factors, may also have contributed,” Ms. Siegel and her associates said.
The temporal pattern was somewhat different for colon cancer. The risk of colon cancer declined “for successive generations during the first half of the twentieth century but has escalated back to the level of those born circa 1890 for current birth cohorts.”
The rising incidence of both colon and rectal cancers among younger adults is “sobering,” given that such trends “often provide a bellwether of the future disease burden,” they noted.
“The strong birth cohort effects we observed signal relatively recent changes in exposures that influence risk,” including excess body weight, high intake of processed meat, low intake of dietary fiber, and low levels of physical activity. “New strategies to curb the obesity epidemic and shift Americans toward healthier eating and more active lifestyles” are needed, the researchers said.
In addition, both clinicians and the public must be educated about the rising probability of the disease in people younger than 55 years. Timely follow-up of symptoms, regardless of patient age, must be emphasized. Younger adults are nearly 60% more likely than are older adults to be diagnosed with advanced colorectal cancer, largely because they delay seeking medical care. The disease simply isn’t “on the radar” of young adults or their providers, the investigators added.
More than 50,000 colorectal cancer deaths are expected in the United States for 2017, according to the American Cancer Society.
