Abstract
- Objective: To summarize the current literature, research findings, and interventions for self-care communication in the physician-patient relationship.
- Methods: Literature review.
- Results: Diabetes management requires patients to follow complex self-care recommendations for nutrition, physical activity, blood glucose monitoring, and medication. Adherence to these recommendations improves glycemic control and mitigates the risk of diabetes complications; however, many patients struggle to follow these behaviors in everyday life. In the physician-patient relationship, self-care communication is largely influenced by interpersonal trust. Physicians need to incorporate interpersonal and relational skills to establish a trusting relationship. Physician-level barriers to self-care communication include lack of time, lack of collaboration and teamwork among health care providers, lack of patients’ access to resources, and lack of psychosocial support for diabetes patients. Among patients, psychosocial barriers and health literacy may affect willingness to discuss self-care. Motivational interviewing techniques may be helpful for improving communication around patient self-management and promotion of healthy behaviors.
- Conclusion: Physicians can assist patients with their diabetes self-care by discussing self-care challenges during medical visits.
Diabetes is one of the most significant and growing chronic health problems in the world, affecting approximately 415 million people [1]. Diabetes is marked by the body’s inability to make insulin as well as the body’s inability to effectively use the insulin it produces [2]. Diagnosis of diabetes has increased sharply in recent decades and is expected to increase even more, with the largest increases in middle- and low-income countries [3]. Diabetes is a leading cause of blindness, kidney failure, myocardial infarction, stroke, and amputation [3], and in 2015 it accounted for 5 million deaths worldwide [1]. Further, diabetes’s costs to society represent 12% ($673 billion) of global health expenditures [1]. By 2040, models predict that 642 million people will be diagnosed with diabetes and costs will continue to grow as the population ages [1]. Thus, prevention of diabetes is the ultimate goal; however, more effective management for individuals already diagnosed with diabetes is critical to reduce the risk of complications and the economic burden of the disease.
Diabetes management requires patients to perform complex self-care regimens, including weight reduction, frequent blood glucose monitoring, taking oral and/or insulin medications, engaging in physical activity, adhering to diabetes nutrition guidelines, and attending clinic appointments [4–9]. These self-care behaviors are critically linked to improved glycemic control, however, integrating them into one’s daily life can be challenging [10–12]. Recent National Health and Nutrition Examination Survey (NHANES) data show that approximately half of adults with diabetes are not meeting recommended goals for diabetes care [13]. Physicians can assist patients with their diabetes self-care by scheduling frequent follow-up visits and discussing self-care challenges with their patients [14].
In this review, we discuss the current literature on physician-patient communication and diabetes self-care. First, we discuss the qualities of an effective physician-patient relationship followed by the importance of self-care communication in diabetes care. Next, we discuss barriers and facilitators to self-care communication. Finally, we review interventions for improving physician-patient communication in diabetes self-care.
Qualities of an Effective Physician-Patient Relationship
Successful diabetes care requires teamwork between physicians and patients [15]. Two components of successful teamwork are physician-patient communication and shared decision-making, both of which have been shown to improve patient satisfaction, adherence to treatment plans and health outcomes [16–23]. In shared decision-making, the physician and patient share medical information [24–26]. Specifically, the physician presents different treatment options to the patient and describes the risks and benefits of each option. Then the patient expresses his or her preferences for treatment to ensure that the care provided aligns with the patient’s values and needs [27]. Thus, shared decision-making in the treatment relationship is predicated on effective communication between the physician and patient [19].
Effective physician-patient communication is supported by continuous care [19,28], a secure attachment style [29, 30], shared goals [19], a mutual understanding of respective roles and tasks [15,31–33], and a bond characterized by liking, confidence, and trust [19,28,31]. Trust is paramount in physician-patient communication. Interpersonal trust and social trust are the 2 predominant types [34]. Interpersonal trust refers to the relationship the patient has with the physician, specifically the confidence the patient has in the physician as well as the responsibility, competence, compassion, and regard the physician has for the patient’s welfare [34–36]. For patients and physicians, interpersonal trust is developed over time with repeated interactions [34–36]. On the other hand, social trust refers to the beliefs of honesty, integrity, and reliability in others [36]. Social trust is influenced by social constructs, including the media and institutions of higher education [36].
In the physician-patient relationship, self-care communication is largely influenced by interpersonal trust. A patient’s trust can be acquired through multiple medical appointments with the physician. Further, how the patient is treated during these appointments as well as how much time and attention the physician invests in the patient’s care influences the level of interpersonal trust. A high level of trust in the relationship can lead to in improvements in adherence to self-care, continuity of care, physician-patient communication, and overall quality of the physician-patient relationship [37–39].
In the diabetes physician-patient relationship, minimal research has explored how trust in one’s physician impacts self-care communication. In a study by Beverly and colleagues, diabetes patients emphasized the importance of a trusting physician-patient relationship for diabetes care [27]. Another study by Ritholz and colleagues found that physicians and patients both stress the importance of developing trust to facilitate self-care communication [40]. Specifically, trust as well as acceptance from the physician contributes to open and honest self-care communication in the physician-patient diabetes relationship[40]. Additional research is needed to determine whether a high level of physician-patient trust is associated with increased self-care behaviors and improved diabetes outcomes over time.
Importance of Diabetes Self-Care Communication
Diabetes self-care communication in the physician-patient relationship increases patient satisfaction, improves adherence to treatment regimens, and leads to better clinical outcomes [22,41–43]. For physicians, effective self-care communication requires the performance of specific communication tasks and behaviors, including collecting a medical history, explaining a diagnosis and prognosis, and providing clear and concise therapeutic instructions [44]. In addition, physicians must incorporate interpersonal and relational skills to establish a trusting relationship [44,45]. Both physicians and patients agree that a trusting treatment relationship is a requirement for open and honest self-care communication [45]. For patients, effective communication necessitates the disclosure of self-care successes and failures [46]. Diabetes patients face challenging self-care regimens, and these challenges can interfere with glycemic control and increase the risk for diabetes complications [47,48]. For this reason, patients must feel comfortable discussing their self-are challenges so that their physician can individualize treatment prescriptions and recommendations, thereby increasing the likelihood of treatment success.
Barriers to Self-Care Communication
Physician-patient self-care communication is essential to improving patient adherence [29,49] yet numerous barriers exist that undermine effective physician-patient self-care communication. From the physician perspective, the most commonly cited barrier to self-care communication is time [50]. A recent study of family medicine practices found that the time physicians spent discussing self-care with their patients varied from 1 to 17 minutes, suggesting that time is a major barrier to self-care communication [51]. Other barriers include lack of collaboration and teamwork among health care providers, lack of patients’ access to resources, and lack of psychosocial support for patients with diabetes [50]. Relatedly, Beverly and colleagues [52] found that physicians often feel inadequately trained to address diabetes patients’ psychosocial issues and this perceived lack of expertise may contribute to physicians feeling overwhelmed and frustrated within the physician-patient relationship, which may hinder open self-care communication.
For patients, barriers tend to differ from those perceived by physicians. A qualitative study using semi-structured interviews with patients and clinicians, and direct observation of clinical encounters at an inner-city family practice training site, revealed different perceptions of the term “control” between physicians and patients. In practice, physicians used the term “control” to focus on the management of blood glucose levels rather than trying to understand the patients’ understanding of diabetes and subsequent treatment goals. Differing viewpoints contributed to frustration and hindered effective communication [53]. In another qualitative study with physicians and patients, both noted that patients were reluctant to discuss self-care for fear being judged or shamed about food intake and weight [45]. This finding was supported in a quantitative follow-up study assessing patient reluctance to discuss self-care. Thirty percent of surveyed patients reported reluctance to discussing self-care with their physicians for fear of being judged, not wanting to disappoint their doctors, guilt, and shame [14]. Interestingly, patients reporting elevated depressive symptoms were more likely to be reluctant to discuss their self-care [14]. Cognitive behavioral changes (eg, cognitive distortions, avoidance behavior, attention deficits) associated with major depression and depressive symptoms may impair patients’ ability to recall self-care information. Also, patients reporting more depressive symptoms may be more socially withdrawn during a medical appointment, and thus less willing to communicate with their physician about self-care.
Other studies found that psychosocial factors such as diabetes distress [54,55] and pessimistic attitudes [56–59], cultural differences [60–66], lack of family and social support [60,67–70], lack of readiness to change behavior [71], introversion and social isolation [72,73], hypo-glycemia fear [74,75] and ineffectual coping styles [76,77] interfere with self-care and glycemic control. Further, low health literacy is associated with difficulty adhering to self-care, particular medication regimens, and negative health outcomes [78].
In summary psychosocial barriers and health literacy may affect a patients’ willingness to discuss self-care during a medical visit. Therefore, routine assessment of psychosocial factors and health literacy may be necessary to address a patient’s barriers to self-care as well as to promote open and honest self-care communication. Interventions and evidenced-based approaches that address psychosocial factors, health literacy, and physician-patient self-care communication are needed.
Facilitators to Self-Care Communication
Despite numerous barriers to self-care communication, several factors promote self-care communication in the physician-patient relationship. For example, direct and non-accusatory communication from physicians as well as providing patients with hope for living with diabetes both support physician-patient self-care communication [45]. A recent systematic review by Sohal and colleagues [79] found that trust in physicians, the use of culturally appropriate exercise and dietary advice, and increasing family involvement improved physician-patient communication and diabetes self-care [79]. Lastly, a study by Schillinger and colleagues [80] found that physician assessment of patient recall and comprehension of new concepts during medical visits improved diabetes outcomes [80].
Patient-Physician Self-Care Communication Interventions
One of the more successful interventions for improving diabetes self-care and patient-physician communication is motivational interviewing (MI). MI is a non-judgmental communication style designed to explore a patient’s intrinsic motivation to change health behaviors [81]. Inherent to MI is the belief that motivation for change is malleable and that it can be transformed in the context of the patient-physician relationship [81]. MI is a patient-centered method designed to empower a patient’s ability and responsibility to make health-related decisions, with the physician supporting the patient’s autonomy in the process [82]. Recent meta-analyses and systematic reviews [83–87] showed that MI interventions improve self-care behaviors and glycemic control in the short-term; long-term effects of MI on self-care and glycemia remain inconclusive. More high-quality research is needed to evaluate the MI training content of these interventions in order to determine its long-term effectiveness and replicate outcomes in various healthcare settings [87].
Other studies not included in the meta-analyses and reviews found MI interventions improved self-care behaviors [88–90], glycemic control [90,91], and quality of life [91]. A qualitative study exploring diabetes patients’ experiences with MI and self-care behaviors revealed that patients’ appreciate when providers initiate discussions that result in new ways of thinking about self-care and promote a sense of well-being in patients [92]. New research utilizing patient navigators to connect diabetes patients’ to their primary care providers showed MI techniques improved patient self-efficacy and glycemic control [93]. Another study, an internet-based incentives study, found that the application of a brief MI interviewing session improved blood glucose monitoring in adolescents with type 1 diabetes [94]. Thus, creative strategies that employ MI techniques in collaboration with other members of the health care team (ie, patient navigation [93], telehealth [89], health coaching [95], internet-based tools [94]) hold promise for improving self-care and patient-physician communication. Increased collaboration with members of the health care team (eg, certified diabetes educators, nurses, dietitians, pharmacists, exercise physiologists), community health workers [96,97] and peer mentors [98,99] may help reinforce messages, promote shared decision-making, improve diabetes outcomes, increase patient satisfaction, and reduce medical costs [100].
Few other interventions have directly addressed physician-patient diabetes self-care communication. One older study examined the effectiveness of an intervention designed to increase of diabetes patients’ involvement in medical decision-making [16]. Patients randomized to the intervention arm participated in a 20-minute session prior to meeting with their physician, in which researchers reviewed their medical chart and used systematic prompts to encourage patients to negotiate medical decisions with their physician. Patients in the control arm received standard educational materials in a session of equal length. Patients in the intervention arm improved glycemia and elicited twice the amount of medical information from their physician compared to controls [16]. These findings suggest that brief interventions prior to medical appointments can improve patient communication, self-care behavior, and in turn, diabetes outcomes [16].
A recent study evaluated the effectiveness of a training program in communication skills for pediatric diabetes care providers in the UK [101, 102]. In this cluster randomized controlled trial, pediatric providers allocated to the Talking Diabetes intervention participated in web-based material and face-to-face seminars designed to prepare providers for constructive self-care conversations with patients as well as skills for promoting behavior change. The psychoeducational training emphasized shared decision-making and utilized motivational interviewing techniques [101]. Twenty-six centers and 693 young people with type 1 diabetes participated in the study [102]. At 12-month follow-up, the Talking Diabetes intervention did not demonstrate improvements in glycemic control. Further, the intervention had a negative effect on patients’ quality of life but a short-term improvement in coping [102]. Interestingly, parents of patients in the intervention arm reported greater continuity of care, which suggests that parents benefited more from the intervention than their children. Future communication interventions targeting the pediatric population should provide ongoing support to children of physicians exposed to interventions such as Talking Diabetes [102].
Currently, 3 ongoing studies aim to improve self-care and clinical outcomes via physician-patient communication interventions. A study by Ricci-Cabello and colleagues [103] aims to improve diabetes self-care by enhancing patient-physician communication in an underserved community of adults with uncontrolled type 2 diabetes. In this 3-arm randomized controlled trial, patients allocated to groups A and B received communication skills training and graphic feedback about glycosylated hemoglobin A 1c levels; patients in group C received usual care. Patients in group B also received telephone reinforcement [103]. The second study, by Billimek and colleagues, aims to improve physician-patient communication about medication regimens via diabetes coaching [104]. In this intervention, 190 Mexican-American adult patients with type 2 diabetes were randomly assigned to complete a Coached Care visit with trained community health workers or a Coached Care visit plus the EMPATHy software toolkit, a computer-based activity with strategies and resources to overcome self-care barriers. The primary endpoints are (1) the development of care plan that addresses everyday barriers to medication adherence and (2) completion of a concrete behavioral goal [104]. Finally, the third study, by Grant and colleagues, aims to improve physician-patient communication via a pre-visit prioritization of diabetes concerns. In this controlled, cluster-randomized, multisite trial, primary care physicians were randomized to the Pre-Visit Prioritization for Complex Patients with Diabetes or the control group [105]. The Pre-Visit Prioritization IT-tool is designed to help patients identify one or two concerns prior to a medical visit and then send these priorities to the primary care physician via an electronic health record. The overall goal of the intervention is to improve communication of self-care concerns during a medical visit [105]. Findings from these 3 interventions are forthcoming; findings may provide evidence for validated interventions that improve physician-patient self-care communication in diabetes.
Techniques to Improve Self-Care Communication
Incorporating communication skills in continuing medical education and diabetes education may improve self-care communication in the physician-patient relationship. Educational programs that teach physicians how to provide consistent messages, repeat information, reinforce and offer feedback regarding specific self-care behaviors, and problem-solve self-care challenges may improve patients’ willingness to discuss self-care [14,106]. Most patients will remember only a small portion of the information given to them during medical visit. Studies that compare how much information patients retain versus how much information physicians provide show that patients forget 31% to 71% of information [107]. Therefore, physicians need techniques that promote open self-care communication during a visit. The following techniques can help physicians improve self-care communication [108]:
- Discuss the most important self-care information first; patients tend to remember the information that is presented first.
- Use the phrase “This is very important…” when discussing key points because patients will remember things that are perceived as important.
- Deliver simple, clear, and concrete instructions; patients are more likely to forget complex or confusing instructions. For example, “Check your blood glucose every morning within five minutes of waking up and before you eat breakfast” is more specific and easier to follow than “Check your blood glucose”.
- Ask open-ended questions to allow patients to verbalize feelings or concerns about their diabetes self-care.
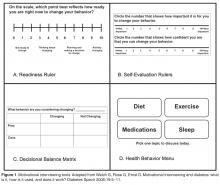
- Employ MI techniques to help patients who are struggling to initiate and adhere to self-care behaviors. MI tools, such as the Readiness Ruler, Self-Evaluation Rulers, Decisional Balance Matrix, and Health Behavior Menu ( Figure), may help patients and physicians discuss self-care behaviors during a medical visit [109].
– Express empathy by reflective listening and asking patients for permission before offering information or advice about diabetes self-care.
– Roll with resistance by engaging the patient in the process of problem solving rather than opposing a patient’s resistance to change behaviors.
– Develop discrepancy by helping the patient recognize that there is an inconsistency between his/her behavior and personal goals.
– Support self-efficacy by empowering the patient to believe that he/she can change behaviors.
6. Demonstrate active listening skills by reflecting and summarizing the patient’s statements. Reflecting and summarizing show the patient that the physician has been listening to concerns and understands what the patient is saying. This is also an opportunity to correct any miscommunications from the visit.
7. Write down instructions or provide handouts to the patient to help reinforce learning and information retention.
8. Ask patients to write a list of questions a few days prior to the medical appointment and bring it with them. Patients are more likely to remember information about issues they have previously considered that directly relate to them.
9. Consider collaborating with community health workers, patient navigators, peer mentors, and other members of the healthcare team to improve communication, diabetes outcomes, and patient satisfaction.
Summary
Physician-patient self-care communication is essential to achieving optimal diabetes outcomes [15,22,33,110] Patients’ ability to inform physicians about their self-care challenges [14], and physicians’ ability to respond to patients’ self-care reports directly and in non-accusatory language, are vital factors in effective diabetes care [45]. Interventions and education that promote open and honest conversations are particularly important given patients’ well-documented struggles achieving self-care and glycemic goals [111] and physicians’ feelings of inadequacy, frustration, and fatigue when they are not making an impact on patients’ outcomes [48,112]. More research is needed to determine the best strategies to improve self-care communication in the physician-patient relationship.
Corresponding author: Elizabeth A. Beverly, PhD, Department of Family Medicine, Ohio University Heritage College of Osteopathic Medicine, Athens, OH 45701, beverle1@ohio.edu.
Financial disclosures: None.
Author contributions: drafting of article, EAB, MFW, ABC, KEP, NNI; critical revision of the article, EAB, MFW, ABC, KEP, NNI.