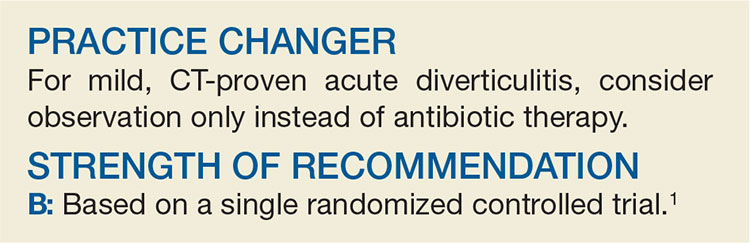
A 58-year-old man presents to your office with a 2-day history of moderate (6/10) left lower quadrant pain, mild fever (none currently), 2 episodes of vomiting, no diarrhea, and no relief with OTC medications. You suspect diverticulitis and obtain an abdominal CT scan, which shows mild, uncomplicated (Hinchey stage 1a) diverticulitis. How would you treat this patient?
Diverticulitis is common; each year, about 200,000 people in the United States are admitted to the hospital because of it.2,3 Health care providers typically treat diverticular disease with antibiotics and bowel rest.2,3 While severe forms of diverticulitis often require parenteral antibiotics and/or surgery, practitioners are increasingly managing the condition with oral antibiotics.4
One previous randomized controlled trial (RCT; N = 623) found that antibiotic treatment for acute uncomplicated diverticulitis did not speed recovery or prevent complications (perforation or abscess formation) or recurrence at 12 months.5 The study’s strengths included limiting enrollment to people with CT-proven diverticulitis, using a good randomization and concealment process, and employing intention-to-treat analysis. The study was limited by the lack of a standardized antibiotic regimen across centers, previous diverticulitis diagnoses in 40% of patients, nonuniform follow-up processes to confirm anatomic resolution, and the lack of assessment to confirm resolution.5
STUDY SUMMARY
Watchful waiting just as effective as antibiotics
This newer study was a single-blind RCT that compared treatment with antibiotics to observation among 528 adults in the Netherlands. Patients were enrolled if they had CT-proven, primary, left-sided, uncomplicated acute diverticulitis (Hinchey stage 1a and 1b).1 (The Hinchey classification is based on radiologic findings, with 0 for clinical diverticulitis only, 1a for confined pericolic inflammation or phlegmon, and 1b for pericolic or mesocolic abscess.6) Exclusion criteria included suspicion of colonic cancer by CT or ultrasound (US), previous CT/US-proven diverticulitis, sepsis, pregnancy, or antibiotic use in the previous 4 weeks.1
Observational vs antibiotic treatment. Enrolled patients were randomly assigned to receive amoxicillin-clavulanate (1,200 mg by IV qid for at least 48 hours, followed by 625 mg po tid, for 10 total days; n = 266) or to be observed (n = 262). Randomization was performed by computer, with a random varying block size and stratification by Hinchey classification and center; allocation was concealed. The investigators were masked to the allocation until all analyses were completed.1
The primary outcome was the time to functional recovery (resumption of pre-illness work activities) during a 6-month follow-up period. Secondary outcomes included hospital readmission rate; complicated, ongoing, and recurrent diverticulitis; sigmoid resection; other nonsurgical intervention; antibiotic adverse effects; and all-cause mortality.
Results. Median recovery time for observational treatment was not inferior to antibiotic treatment (14 d vs 12 d; hazard ratio for functional recovery, 0.91). Observation was not inferior to antibiotics for any of the secondary endpoints at 6 and 12 months of follow-up: complicated diverticulitis (3.8% vs 2.6%, respectively), recurrent diverticulitis (3.4% vs 3%), readmission (17.6% vs 12%), or adverse events (48.5% vs 54.5%). Initial hospitalization length of stay was shorter in the observation group (2 vs 3 d). The researchers conducted a 24-month telephone follow-up, but no differences from the 12-month follow-up were noted.1
Continue to: WHAT'S NEW