LOS ANGELES – Stroke survivors are at a significantly increased risk of developing health problems that can impact their daily life even if they have experienced only a single stroke and are still living in the community, according to an analysis of the Health and Retirement Study.
Stroke survivors are significantly more likely to fall and to have memory and motor impairment, urinary incontinence, and some sleep disturbance after having a stroke, compared with age-matched controls, Afshin Divani, Ph.D., reported at the International Stroke Conference.
"Physicians, caregivers, and rehabilitation providers need to pay particular attention to these comorbid conditions," particularly in light of the aging population and increased number of stroke survivors, said Dr. Divani, director of stroke research at the University of Minnesota Medical Center in Fairview.
The Health and Retirement Study, launched in 1992, is a national representative sample of community-living adults aged 50 years and older. It examines economic circumstances, health, and marital and family status using a questionnaire delivered every other year. Beginning in 1998, the survey was expanded to include questions directed at specific subgroups, including stroke survivors. Questions about stroke are administered only to participants who are at least 65 years old.
Dr. Divani and his colleagues used the database to conduct a longitudinal study of health problems in stroke survivors. "We collected information on 631 stroke subjects who were noninstitutionalized. We excluded anyone who was institutionalized in the next interview wave, as well as those who had experienced multiple strokes."
The team collected demographic information, as well as data on living arrangements, physician-diagnosed disorders (diabetes, cancer, lung disease, psychiatric disorders, and neurologic/sensory disorders); general health; and health problems (pain, incontinence, sleep, falls, and fall-related injury).
They compared data from stroke survivors with data from an age- and sex-matched control cohort of 631 survey participants.
The subjects’ mean age was 75 years; 53% were female. Self-reported general health was significantly lower in stroke survivors, with 22% reporting poor health, compared with 7% of controls. Similarly, 34% of survivors reported fair health, compared with 21% of controls. But only 2% of stroke survivors reported excellent health, compared with 9% of controls. Health was rated as very good by 12% of stroke survivors and 28% of controls.
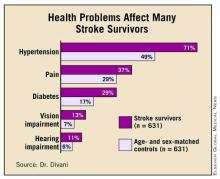
Diabetes, pain, hypertension, and vision and hearing impairment were all significantly more common among stroke survivors. (See box.) Significantly more survivors (15% vs. 6%) also needed a proxy respondent to complete the interview. "This suggests that stroke survivors were unable to answer questions, hold the phone, or participate in a face-to-face interview," Dr. Divani said.
For the longitudinal study, the investigators tried to pinpoint when the health problem occurred – a difficult task, because only the stroke questions involved a time stamp. "We looked at subsequent interview waves and went back to see if the respondents already had those problems before the stroke, and if they did, we excluded them from the study," Dr. Divani said.
In the longitudinal analysis, motor impairment was significantly more common among stroke survivors (33% vs. 24%), as was urinary incontinence (19% vs. 11%).
Among the four dimensions of sleep quality that the investigators assessed (trouble falling asleep, waking up at night, waking early, and not feeling rested), only one – not feeling rested – was significantly more common among survivors (33% vs. 22%). Falling and fall-related injuries were also significantly more common.
There also was a significant association between stroke and memory deficit, occurring in 9% of survivors and 3% of nonstroke subjects.
The investigators then conducted a multivariate analysis to determine which problems were significantly more likely to develop after a stroke. The strongest risk was for memory deficit (odds ratio, 2.4). Survivors also had 64% greater odds of having urinary incontinence and 45% greater odds of having motor impairment than did controls. In the area of sleep quality, survivors had 59% greater odds of not feeling rested, although there were no significant risks associated with the other aspects of sleep.
All aspects of falls and fall-related injuries became nonsignificant in the multivariate analysis, Dr. Divani noted. "This may be because fear of falling makes them more careful, and having a motor deficit prevents them from doing a complex task like climbing stairs," so if a fall occurs, it’s more likely to be while walking on a flat surface, and not from an elevated location. "A stair fall has a much higher risk of injury than someone falling while walking."
Although the data paint a good initial picture of poststroke health issues, Dr. Divani cautioned that it probably underestimates the true impact. "I need to emphasize that we selected noninstitutionalized subjects who had only one stroke," he said. "We selected the most healthy stroke survivors, which means we are probably underestimating the true problems among stroke patients."