You say you want a revolution
Well, you know
We all want to change the world
—John Lennon
Gynecology was once a revolutionary specialty. Innovative and enterprising, its members were pioneers in operative laparoscopy, and they educated other surgical services on the merits and techniques of endoscopy.
Today the specialty lags behind others in both innovation and adoption of minimally invasive surgical techniques (FIGURE). By 2007, 95% of cholecystectomies were performed laparoscopically, as well as 90% of bariatric procedures and 70% of appendectomies. In contrast, only 20% of hysterectomies were performed using the laparoscopic approach. One reason for this discrepancy may be the extraordinary confidence that patients have in their gynecologist.
Consider the two sides of a coin that were revealed by the findings of an Internet survey of 526 women conducted by Russell Research and commissioned by the Patient Awareness Program of the AAGL. On one hand, investigators found that survey participants shared a steadfast opinion that their gynecologist would describe all available treatment choices, including the least traumatic and safest surgical procedures. Ninety-eight percent expected their physician to describe minimally invasive treatment options even if he or she was not proficient in them at the time—and to mention options that entail the least amount of pain. In addition, 94% of respondents expected their gynecologist to promote options with the lowest impact on lifestyle.1 Yet, on the other hand, although 517 of 528 (98%) respondents who were 18 years or older had experienced stress urinary incontinence, fibroids, or uterine prolapse, fewer than 40% were aware that a number of minimally invasive techniques could greatly reduce the need for hysterectomy. Fewer than 50% of respondents who suffered from menorrhagia were aware of endometrial ablation as a treatment, and only 21% realized that it could be performed in an office. Only 45% of women who had leiomyomata had heard of myomectomy. And one of every three women who had stress urinary incontinence was unaware of sling procedures. Fewer than 20% knew that sterilization could be performed in an office.1 Although these women expected to be thoroughly informed by their physician, their lack of awareness suggests the opposite.
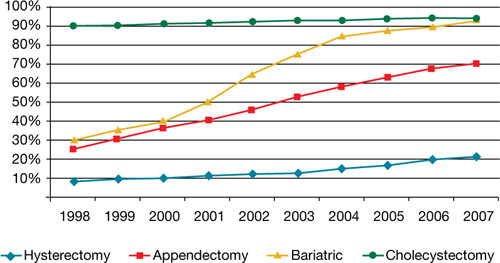
Use of minimally invasive options for 4 common surgeries
Resident physicians need more hands-on experience
A barrier to adoption of minimally invasive surgical approaches is the limited access many residents have to training and experience. This barrier could become especially problematic as third-party payers gain awareness of the advantages of minimally invasive surgery and shift reimbursement accordingly. In association with the American Society of Reproductive Medicine (ASRM), AAGL is actively engaged in enhancing surgical education through its Fellowship in Minimally Invasive Gynecology and is designing programs to supplement resident education. It is also establishing centers of excellence through its professional interest partner, the Council on Gynecologic Endoscopy (CGE).
Although the solution to our problem seems simple—increase the number of gynecologists who perform minimally invasive gynecologic surgery—that is easier said than done. According to data from the Accreditation Council for Graduate Medical Education ( ACGME), one of every three graduating residents has limited experience in minimally invasive procedures, and 30% of residents perform an average of only 12 laparoscopic operations a year as the primary surgeon. The average is even lower for hysteroscopic procedures!2

In an article published earlier this year in the Journal of Minimally Invasive Gynecology, Jon I. Einarsson, MD, MPH, and colleagues explore attitudes toward hysterectomy among gynecologists in the United States.3 Although nearly three quarters of hysterectomies are performed using an open abdominal approach, only 8% of respondents said they would choose the abdominal approach for themselves or their spouse. Among respondents who reported the highest surgical volumes, the percentage likely to choose a laparoscopic approach was significantly higher. The main barriers to laparoscopic hysterectomy? Limited opportunity for training during residency, technical difficulty, personal surgical experience, and operating time.3
We need an advanced curriculum
We have made tremendous progress in postgraduate education, thanks to the efforts of AAGL and ASRM. Nevertheless, we lack a specific, unified curriculum to train and ultimately credential gynecology residents and fellows in minimally invasive surgery.
Once again, our specialty lags behind general surgery. As of July 2009, all residents performing general surgery are required to complete and pass a course, “Fundamentals of laparoscopic surgery” (FLS). This joint undertaking of the American College of Surgeons and the Society of American Gastrointestinal and Endoscopic Surgeons has established minimum standards for basic cognitive and technical skills required for laparoscopic surgery.
Using the FLS course as a model, AAGL is designing a structured core curriculum to educate not only residents and fellows, but practicing gynecologists as well. Like the FLS course, the AAGL curriculum will emphasize both didactic teaching and lab skills, but it will be even more extensive because it will include hysteroscopy.


