CLICK HERE to access 6 articles about treating postpartum hemorrhage published in OBG Management in 2011 and 2012.
CASE You are performing a cesarean delivery for a 30-year-old G1P0 woman who presented in labor with a breech fetus at term. Earlier in the pregnancy an external version was unsuccessful in achieving a cephalic presentation. The breech delivery of the newborn is uncomplicated but, immediately following delivery of the placenta, you note excessive uterine bleeding and diagnose a postpartum hemorrhage (PPH) due to uterine atony. Manual massage of the uterus and administration of oxytocin, misoprostol, carboprost tromethamine (Hemabate), and methergine do not result in resolution of the hemorrhage. Your assistant suggests a uterine compression suture to treat the PPH.
What uterine compression suture would you choose?
The management of PPH can be conveniently described using one algorithm for cases that follow a vaginal delivery, and another algorithm for PPH that occurs during cesarean delivery (see “Managing PPH following vaginal and cesarean delivery”). If PPH does not respond to initial treatment steps, more invasive and resource-intensive steps should be performed quickly. Time is critical; delay in initiating escalating steps in the treatment algorithm should be minimized.
PPH at cesarean: Remember your suture options!
In the algorithm for the treatment of PPH occurring at the time of cesarean delivery, the uterine compression suture is an important option.
In 1997, Christopher B-Lynch reported1 on the first widely utilized uterine compression suture. Alternative compression sutures have been reported by Hayman,2 Pereira,3 and others. Every obstetrician should be proficient with the placement of at least one uterine compression suture for the treatment of PPH caused by uterine atony.
Consider the hysterotomy
When it’s open. When PPH caused by uterine atony occurs at cesarean delivery and the hysterotomy incision is open, the B-Lynch suture (FIGURE 1) is a common selection by obstetricians.
When it’s closed. When the hysterotomy is already closed when PPH is noted, the Hayman or Pereira suture(s) are often selected by obstetricians (FIGURES 2 AND 3). Both of these compression sutures also could be applied when the hysterotomy is open.
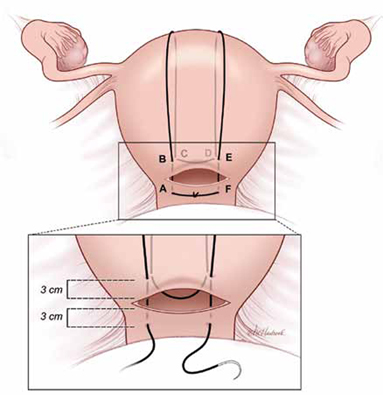
FIGURE 1 B-Lynch suture
The B-Lynch suture as seen from the anterior uterine wall.
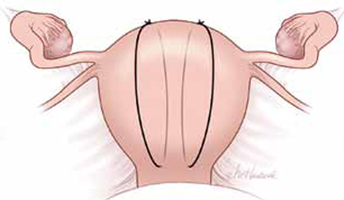
FIGURE 2 Hayman suture
The Hayman suture passes directly from the anterior uterine wall through the posterior uterine wall. Two to four longitudinal sutures can be placed. Two longitudinal sutures are pictured in this figure. A transverse cervicoisthmic suture also can be placed, if needed, to control bleeding from the lower uterine segment.
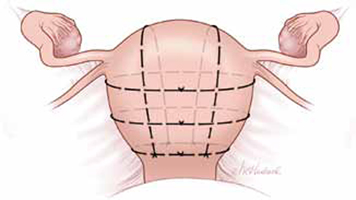
FIGURE 3 Pereira sutures
The Pereira sutures combine longitudinal and transverse sutures placed as a series of bites into the submucosal myometrium. The sutures do not enter the uterine cavity. The longitudinal sutures begin and end at the level of the transverse suture closest to the cervix. Avoid damage to blood vessels and the ureters when placing the transverse sutures. Two longitudinal sutures and three transverse sutures are pictured in this figure.
Combination treatment
Consider combining a uterine compression suture with either:
- placement of an intrauterine balloon, the so-called uterine sandwich,4 or
- uterine devascularization sutures (O’Leary ligation of branches of uterine artery and ligation of the uterine-ovarian arteries).
It’s important to note that the combination of a uterine compression suture with devascularization sutures may be associated with a higher rate of uterine ischemia and myometrial necrosis than the combination of compression sutures with an intrauterine balloon.5
Placing the B-Lynch suture
The B-Lynch suture (FIGURE 1) is placed with the following steps:
1) Take bites on either side of the right edge of the hysterotomy incision (A and B). These bites are placed approximately 3 cm from the edge of the hysterotomy incision.
2) Loop the suture around the fundus and reenter the uterus through the posterior uterine wall at point C, which is directly below point B.
3) Pull the suture tightly, but do not tear into the myometrium.
4) Exit the posterior wall of the uterus through point D.
5) Loop the suture over the uterine fundus.
6) Anchor the suture in the lower uterine segment by taking bites on either side of the left edge of the uterine hysterotomy incision (E and F).
7) Pull the two ends of the suture tight while an assistant simultaneously squeezes the uterus to aid compression.
8) Place a surgical knot while the assistant continues to compress the uterus.
9) Close the lower uterine segment in the usual manner. B-Lynch1 advised that if there is excessive bleeding from a specific area of the uterus (possible placenta accreta) that a figure-of-8 stitch should be placed through that area of the uterus prior to placing the compression suture.


