Clinical Review

2014 Update on abnormal uterine bleeding
Randomized data shed light on AUB associated with fibroids, adenomyosis, and the use of progestins
Amy Garcia, MD, is Director, Center for Women’s Surgery and Garcia Institute for Hysteroscopic Training, Albuquerque, and Clinical Assistant Professor, Department of Obstetrics and Gynecology, University of New Mexico School of Medicine, Albuquerque. Dr. Garcia serves on the OBG Management Board of Editors.
Dr. Garcia reports that she receives grant or research support from Hologic, Inc. She is a consultant to Bayer, Boston Scientific, Channel Medsystems, Ethicon, Hologic, IOGYN, Karl Storz Endoscopy, Minerva Surgical, and Smith & Nephew. She is a speaker for Ethicon.

The cesarean scar defect: A common etiology of abnormal uterine bleeding
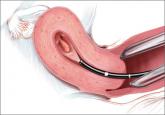
CESAREAN SCAR DEFECT DIAGNOSED WITH HYSTEROSCOPY


Videos courtesy of Amy Garcia, MD
CASE: POSTMENSTRUAL BLEEDING, HISTORY OF CESAREAN DELIVERIES
A 36-year-old woman (G3P3) reports prolonged and postmenstrual bleeding. Her cycles are regular, every 28 to 30 days, and are associated with ovulatory symptoms. She bleeds for 8 to 10 days with each cycle, having heavy bleeding on cycle day 2 requiring use of super tampons every 3 hours. Beginning on day 5 of the cycle, the blood becomes much darker and scant requiring a small pad, which she changes twice daily. Often, she experiences dark bleeding with physical activity—specifically, running—usually several days after her cycle has ended. She is otherwise healthy and uses no medications. She uses condoms for contraception. She has had a prior vaginal delivery followed by two cesarean sections. Physical examination is normal.
What is causing this patient’s abnormal bleeding pattern?
From 1996 to 2009, the total US cesarean delivery rate increased steadily from 20.7% to 32.9% and has remained stable at 32.8% through 2012. 1 With 3,952,841 registered births in 2012, the number of operative procedures performed annually approximates 1.3 million. 2 This means, potentially, that one-third of pregnant American women will undergo cesarean delivery annually, translating into an increasing prevalence of long-term sequelae of this surgery.
An increasingly recognized etiology of AUB
One long-term complication of cesarean delivery, not often discussed, is the presence of a defect within the uterine scar that is directly associated with a type of abnormal uterine bleeding (AUB) referred to as postmenstrual bleeding. Stewart first reported this post–cesarean delivery phenomenon in 1975. 3 It is postulated that the cesarean scar defect (CSD) 4 forms a pocket, which holds the menstrual effluent, allowing bleeding to occur after regular menstrual cycle bleeding has concluded. Often, remnant menstrual blood is extruded slowly over several days, and is generally dark brown, indicating old blood. Physical activity sometimes can initiate expulsion of the old blood even after the regular cycle has ceased ( FIGURE 1 ).
As early as 1995, Morris reported the histopathologic changes within the cesarean scar in a series of 51 hysterectomy specimens with scar present for 2 to 15 years. His findings included distortion and widening of the lower uterine segment (75%), congested endometrium above the scar recess (61%), marked lymphocytic infiltration (65%), capillary dilation (65%), residual suture material with foreign body giant cell reaction (92%), fragmentation and breakdown of the endometrium of the scar (37%), and iatrogenic adenomyosis confined to the scar (28%). Morris concluded that in addition to AUB, these scar abnormalities could give rise to clinical symptoms such as pelvic pain, dyspareunia, and dysmenorrhea. 5 It also has been suggested that otherwise unexplained infertility is associated with anatomic and physiologic changes seen with CSD. 6 A recent review article published by Tower summarized additional clinical outcomes of CSD, such as ectopic pregnancy and increased surgical risks for such gynecologic procedures as uterine evacuation in the nonpregnant or postpartum state, hysterectomy, endometrial ablation, and intrauterine device placement. 4
The CSD generally is described as a triangular or circular sonographically anechoic area in the myometrium of the anterior lower uterine segment or cervix at the site of a previous cesarean section. In nonpregnant patients, the defect is best evaluated with contrast infusion sonography (CIS), such as saline infusion or gel infusion, versus transvaginal ultrasound (TVUS) alone ( FIGURE 2 ).4,7,8 However, the precise dimensions and definition of the scar defect vary among investigators. 4,6,7,8,10

Randomized data shed light on AUB associated with fibroids, adenomyosis, and the use of progestins

How to assess technology and apply new findings to patient care
Understanding of abnormal uterine bleeding has been hampered by inconsistent use of terminology and a lack of classification of its causes, but...
