DALLAS – Low-dose ketamine as an adjunct to intravenous morphine for moderate to severe pain in the emergency department provides superior relief, compared with morphine alone, according to a randomized, double-blind clinical trial.
Ketamine at subanesthetic doses was an effective analgesic with an opioid-sparing effect. However, this utility must be balanced against an increase in potentially problematic side effects, including dizziness, dysphoria, and sinus tachycardia in some cases, at the higher of the two doses tested, Dr. Francesca L. Beaudoin said at the annual meeting of the Society for Academic Emergency Medicine.
The study was conducted at a single, large, urban, academic ED, where 60 adults presented with pain of less than 7 days’ duration and an average baseline pain score of 9 out of a possible 10 on a numeric rating scale. Study participants were placed on standard of care IV morphine at 0.1 mg/kg and randomized to one of three treatment arms featuring adjunctive placebo, IV ketamine at 0.1 mg/kg, or ketamine at 0.3 mg/kg. Patients’ pain status was assessed at 30, 60, and 120 minutes after administration of their study medication. They received rescue analgesia as needed in order to achieve a 50% reduction in pain, explained Dr. Beaudoin, an emergency medicine physician at Rhode Island Hospital and Brown University, Providence, R.I.
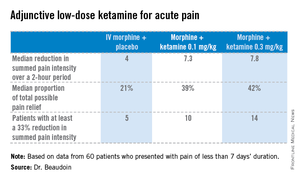
The primary endpoint was pain intensity reduction, as calculated by adding together the differences in pain scores from baseline to each of the three assessment points. Results on this endpoint and related secondary outcome measures were significantly better in the two ketamine groups than in the morphine-only control arm. A clinically meaningful reduction in acute pain scores was achieved in 25% of those treated with 0.1 mg/kg of IV morphine plus placebo, 50% given morphine plus 0.1 mg/kg of IV ketamine, and 70% given morphine plus IV ketamine at 0.3 mg/kg.
Although there were consistent trends favoring greater efficacy for the higher vs. the lower dose of ketamine, these differences didn’t achieve statistical significance, probably because of the small study size, she said.
There was a trend for ketamine at 0.3 mg/kg to provide more durable pain relief. Both ketamine groups had a median 4-point decrease in numeric pain rating scores at 30 and 60 minutes. At 120 minutes, however, the group given lower-dose ketamine had backslid to a median 2.5-point reduction, compared with baseline; the higher-dose group still averaged a 4-point improvement in pain scores. In contrast, patients in the control group had a median 2-point decrease in pain intensity at all three time points.
No clinically important differences in sedation scores were noted between the three treatment groups. Nor were there any differences in time to discharge from the ED, nor in hospital admission rates.
Nine patients in the morphine-alone arm received rescue analgesia, as did four in each of the two adjunctive ketamine groups.
The adverse event profile was noteworthy, she said, and "it’s probably going to be important when we use this study information moving forward." Nine of the 20 patients in the higher-dose ketamine group had dizziness, and five of them had dizziness that lasted up to an hour. Three in the higher-dose ketamine group and two in the lower-dose group had dysphoria, which they regarded as unpleasant. "Two patients in the higher-dose ketamine group actually called the experience ‘scary’ and said they wouldn’t want to do it again," according to Dr. Beaudoin.
Also, three patients on higher-dose ketamine developed sinus tachycardia, with a heart rate of 150 bpm in one case. These events were transient, didn’t require intervention, and resolved spontaneously within 30 minutes. Nevertheless, this must be a consideration in introducing adjunctive low-dose ketamine more broadly into clinical practice, particularly in patients who may have cardiac disease.
The surgical literature provides evidence that low-dose ketamine improves postoperative pain and confers an opioid-sparing effect. The reason the practice hasn’t been adopted into clinical practice in EDs is probably because of the lack of randomized, controlled clinical trials addressing this question – until now, she noted.
"In terms of future directions, I think what’s really interesting is to try to identify what subgroups this is useful for and who it is safe in. That’s where I think this should move," Dr. Beaudoin said.
She reported having no relevant financial conflicts. The study was funded by the University Emergency Medicine Foundation.