LAS VEGAS – Morcellation during laparoscopic hysterectomy or myomectomy for presumed large fibroids provides slightly better 5-year overall survival and higher quality of life scores than abdominal hysterectomy, according to a new study.
The strength of this soon-to-be-published decision analysis lies in its balance and comprehensive nature. It utilized the best-available published literature to estimate the mortality risk stemming from tissue dissemination of occult leiomyosarcoma through power morcellation – an issue of hot controversy – but it also incorporated the increased risks of procedure-related morbidity and mortality associated with the alternative to morcellation in patients with large fibroids: that is, abdominal hysterectomy, Dr. Matthew Siedhoff explained at the annual Minimally Invasive Surgery Week.
The decision analysis was undertaken in the wake of the Food and Drug Administration’s April 2014 safety warning citing a 1 in 350 risk of occult malignancy in women undergoing hysterectomies or myomectomies for removal of presumed fibroids and that laparoscopic surgeries involving power morcellation performed in women with unsuspected uterine sarcomas may spread cancerous tissue, potentially shortening survival. The attendant publicity has caused considerable alarm and confusion among patients and the general public. The FDA is currently deliberating possible actions ranging from a black box warning to outright banning of power morcellation.
Meanwhile, several prominent medical centers, including Brigham and Women’s Hospital, Massachusetts General Hospital, both in Boston, and the Cleveland Clinic, have banned the use of power morcellation – precipitously, in Dr. Siedhoff’s view.
Also since the FDA safety statement, Johnson & Johnson has taken its power morcellator off the market and several large insurance companies have announced plans to halt reimbursement when power morcellation is used in gynecologic surgery. However, exactly how that would happen is unclear because there is no billing code associated with power morcellation, and it would be arduous for insurers to actually read through all operative reports.
“This decision analysis is a tool for surgeons and patients to help make informed decisions. It balances the FDA analysis, which pretty much just emphasizes morcellation risk to the exclusion of all the known benefits of laparoscopy. The analysis argues that reducing the risk associated with morcellation – perhaps through the use of specimen containment or preoperative leiomyosarcoma diagnosis – is a better approach than abandoning minimally invasive gynecologic surgery for fibroids. That would be throwing the baby out with the bathwater,” declared Dr. Siedhoff, an ob.gyn. and director of the division of advanced laparoscopy and pelvic pain at the University of North Carolina, Chapel Hill.
A decision analysis entails probability modeling of outcomes based upon consensus event rates obtained from studies in the published literature.
“It’s helpful to do a decision analysis when you can’t do a randomized controlled trial, which you certainly can’t for this issue,” he observed at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
The decision analysis was carried out by Dr. Siedhoff and coinvestigators at the University of North Carolina at Chapel Hill, with department of obstetrics and gynecology chair Dr. Daniel Clarke-Peterson as senior author. The researchers assumed two hypothetical cohorts of 100,000 women undergoing hysterectomy for fibroids large enough that surgical options were limited to laparoscopic hysterectomy with morcellation or abdominal hysterectomy. The primary outcomes were 5-year overall mortality and quality of life as measured in quality-adjusted life-years (QALYs).
The analysis assumed that among the 100,000 women in each group there would be 120 FIGO Stage I or II occult leiomyosarcomas, with an associated 59% 5-year mortality from cancer. It was further assumed that intraperitoneal dissemination of tumor via morcellation would in effect boost those cancers to FIGO Stage III, with 72% mortality at 5 years. This would result in 86 deaths from leiomyosarcoma over 5 years in the morcellation group, compared with 71 in women who underwent abdominal hysterectomy. However, this was counterbalanced by more hysterectomy-related deaths in the abdominal hysterectomy group: 32, compared with 12 in women undergoing morcellation. The final 5-year tally: 98 deaths overall in the morcellation group and 103 in the abdominal hysterectomy group.
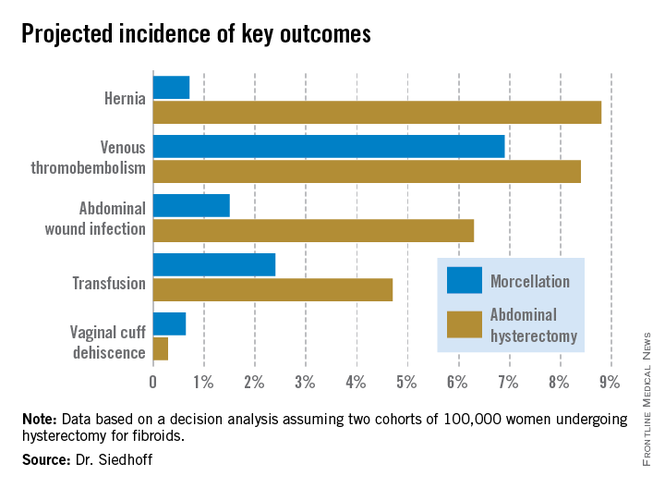
QALYs are calculated by estimating how much a given adverse event – for example, venous thromboembolism, along with its attendant treatment and potential further complications – would diminish a theoretical year of otherwise perfect health. The total QALYs in the group of 100,000 women undergoing morcellation was estimated at 499,171, compared with 490,711 over 5 years in the abdominal hysterectomy group. That’s because with the exception of vaginal cuff dehiscence, all of the other complications assessed in the decision analysis, including wound infections, transfusions, hernias, and venous thromboembolisms, were more frequent in the abdominal hysterectomy group. The forthcoming final publication will include the citations on which all of the event probabilities were based.