SAN DIEGO – The hottest topic today in the treatment of sexually transmitted diseases caused by Chlamydia trachomatis is the unresolved question of whether azithromycin is still as effective as doxycycline, the other current guideline-recommended, first-line therapy, Dr. Kimberly Workowski said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
“This is important, because doxycycline is administered twice a day for 7 days, and azithromycin is given as a single pill suitable for directly observed therapy,” noted Dr. Workowski, professor of medicine at Emory University in Atlanta and lead author of the 2015 Centers for Disease Control and Prevention STD treatment guidelines.
Several recent retrospective case series have suggested azithromycin is less effective, with the biggest efficacy gap being seen in rectal C. trachomatis infections. These nonrandomized studies were further supported by an Australian meta-analysis of six randomized, controlled trials comparing the two antibiotics for the treatment of genital chlamydia. The investigators found roughly 3% greater efficacy for doxycycline, compared with azithromycin, for urogenital chlamydia, and a 7% advantage for doxycycline in treating symptomatic urethral infection in men.
However, the investigators were quick to add the caveat that “the quality of the evidence varies considerably” (Clin Infect Dis. 2014 Jul 15;59(2):193-205).
There’s a pressing need for better data. Dr. Workowski and her colleagues on the STD guidelines panel are eagerly awaiting the results of a well-structured randomized trial led by Dr. William M. Geisler, professor of medicine at the University of Alabama, Birmingham. The investigators randomized more than 300 chlamydia-infected male and female inmates in youth correctional facilities to guideline-recommended azithromycin at 1 g orally in a single dose or oral doxycycline at 100 mg twice daily for 7 days. The results, which are anticipated soon, should influence clinical practice, Dr. Workowski said.
“There is something going on here that we’re trying to understand. It may have something to do with organism load,” according to Dr. Workowski.
Here’s what else is new in chlamydia:
•Pregnancy: For treatment of chlamydia in pregnancy, amoxicillin at 500 mg orally t.i.d. for 7 days has been demoted from a first-line recommended therapy to alternative-regimen status. Now, the sole recommended first-line treatment in pregnancy is oral azithromycin at 1 g orally in a single dose.
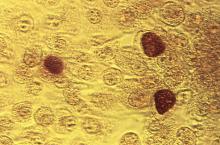
“We did this based on in vitro studies showing Chlamydia trachomatis is not well-killed by amoxicillin. Instead, the drug induces persistent viable noninfectious forms which can sometimes reactivate,” Dr. Workowski explained.
•Delayed-release doxycycline: This FDA-approved drug, known as Doryx, administered as a 200-mg tablet once daily for 7 days, “might be an alternative” to the standard generic doxycycline regimen of 100 mg twice daily for 7 days, according to the current Centers for Disease Control and Prevention guidelines. In a randomized, double-blind trial, the new agent was as effective as twice-daily generic doxycycline in men and women with urogenital C. trachomatis infection, and it had fewer gastrointestinal side effects. Doryx is costlier than the twice-daily alternatives.
• Lymphogranuloma venereum: The current guidelines repeat a point made in previous editions, but one Dr. Workowski believes remains underappreciated and thus worthy of emphasis: Rectal exposure to C. trachomatis serovars L1, L2, and L3 in men who have sex with men or in women who have rectal sex can cause lymphogranuloma venereum, which takes the form of proctocolitis mimicking inflammatory bowel disease.
At the time of the initial visit, before results of diagnostic tests for chlamydia are available, patients suspected of having lymphogranuloma venereum should be started presumptively on the recommended regimen for this STD, which is oral doxycycline at 100 mg b.i.d. for 21 days.
“If you also see painful ulcers or, on anoscopy, mucosal ulcers, you should also treat empirically for herpes simplex until your culture results come back,” she added.
Dr. Workowski reported having no financial conflicts of interest.