Clinical Review
Zika virus: Counseling considerations for this emerging perinatal threat
Zika virus infection, although typically mild and often asymptomatic, can have serious consequences in pregnancy. As the pandemic rapidly spreads...
Anushka Chelliah, MD, and Patrick Duff, MD


The authors report no financial relationships relevant to this article.

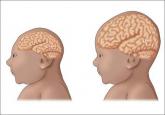
To make the determination that Zika virus (ZV) causes microcephaly, Rasmussen and colleagues1 very recently evaluated Shepard’s 7 criteria,2 published in 1994, for establishing a cause between a microorganism and a specific clinical condition. These 7 criteria are:
References
Zika virus infection, although typically mild and often asymptomatic, can have serious consequences in pregnancy. As the pandemic rapidly spreads...

Physicians have requested information about which insect repellents to recommend to help pregnant women avoid Zika and other mosquito-born...

Recent studies offer new data on treatments for surgical-site infections after cesarean delivery, postpartum endometritis, and chlamydia infection...

Which infections affect women more adversely during pregnancy, and how can risk of exposure to these infections be diminished?
