Therapeutic hypothermia (TH) for moderate and severe neonatal encephalopathy has been shown to reduce the risk of newborn death, major neurodevelopmental disability, developmental delay, and cerebral palsy.1 It is estimated that 8 newborns with moderate or severe neonatal encephalopathy need to be treated with TH to prevent 1 case of cerebral palsy.1 The key elements of TH include:
- initiate hypothermia within 6 hoursof birth
- cool the newborn to a core temperature of 33.5˚ C to 34.5˚ C (92.3˚ F to 94.1˚ F) for 72 hours
- obtain brain ultrasonography to assess for intracranial hemorrhage
- obtain sequential MRI studies to assess brain structure and function
- initiate EEG monitoring for seizure activity.
During hypothermia the newborn is sedated, and oral feedings are reduced. During TH, important physiological goals are to maintain normal oxygenation, blood pressure, fluid balance, and glucose levels.1,2
TH: The basics
Most of the major published randomized clinical trials used the following inclusion criteria to initiate TH2:
- gestational age at birth of ≥ 35 weeks
- neonate is within 6 hours of birth
- an Apgar score ≤ 5 at 10 minutes of life or prolonged resuscitation at birth or umbilical artery cord pH < 7.1 or neonatal blood gas within 60 minutes of life < 7.1
- moderate to severe encephalopathy or the presence of seizures
- absence of recognizable congenital abnormalities at birth.
However, in some institutions, expert neonatologists have developed more liberal criteria for the initiation of TH, to be considered on a case-by-case basis. These more inclusive criteria, which will result in more newborns being treated with TH, include3:
- gestational age at birth of ≥ 34 weeks
- neonate is within 12 hours of birth
- a sentinel event at birth or Apgar score ≤ 5 at 10 minutes of life or prolonged resuscitation or umbilical artery cord pH < 7.1 or neonatal blood gas within 60 minutes of life < 7.1 or postnatal cardiopulmonary failure
- moderate to severe encephalopathy or concern for the presence of seizures.
Birth at a gestational age ≤ 34 weeks is a contraindication to TH. Relative contraindications to initiation of TH include: birth weight < 1,750 g, severe congenital anomaly, major genetic disorders, known severe metabolic disorders, major intracranial hemorrhage, severe septicemia, and uncorrectable coagulopathy.3 Adverse outcomes of TH include thrombocytopenia, cardiac arrythmia, and fat necrosis.4
Diagnosing neonatal encephalopathy
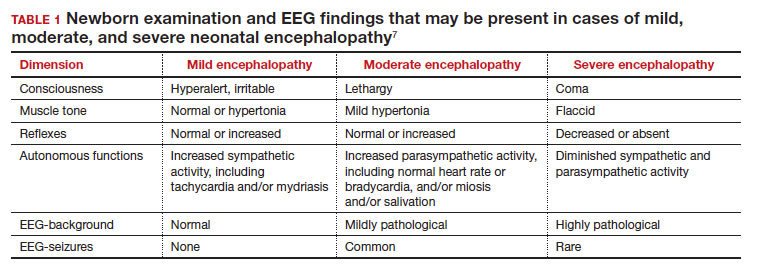
Neonatal encephalopathy is a clinical diagnosis, defined as abnormal neurologic function in the first few days of life in an infant born at ≥ 35 weeks’ gestation. It is divided into 3 categories: mild (Stage 1), moderate (Stage 2), and severe (Stage 3).5,6 Institutions vary in the criteria used to differentiate mild from moderate neonatal encephalopathy, the two most frequent forms of encephalopathy. Newborns with mild encephalopathy are not routinely treated with TH because TH has not been shown to be helpful in this setting. Institutions with liberal criteria for diagnosing moderate encephalopathy will initiate TH in more cases. Involvement of a pediatric neurologist in the diagnosis of moderate encephalopathy may help confirm the diagnosis made by the primary neonatologist and provide an independent, second opinion about whether the newborn should be diagnosed with mild or moderate encephalopathy, a clinically important distinction. Physical examination and EEG findings associated with cases of mild, moderate, and severe encephalopathy are presented in TABLE 1.7
Continue: Obstetric factors that may be associated with neonatal encephalopathy...