Maintaining continence
Urinary continence. To maintain continence, there must be either an intrinsic urethral pressure greater than the pressure in the bladder or occlusion of the urethra when intra-abdominal pressure increases.
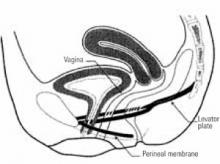
When the anatomy of the pelvis is intact, the proximal urethra and bladder base are held above the perineal membrane (FIGURE 5). Some experts believe that an intra-abdominal urethral position at or above the perineal membrane, within the socalled continence zone, maintains female continence. This is because increases in intra-abdominal pressure are equally transmitted to the urethra and bladder, when the proximal urethra remains in the continence zone; the intrinsically higher urethral pressure maintains closure without leakage of urine.20
The hammock theory of urinary incontinence, meanwhile, proposes that the midurethra is held closed by suburethral support. Increases in intra-abdominal pressure push the urethra down onto these supporting tissues and functionally obstruct the urethra to maintain continence.21 As long as there is adequate support below the urethra, this theory holds, continence is maintained. Both mechanisms—intra-abdominal urethral positioning and suburethral support—may contribute to urinary continence.
Continence also is maintained neurologically, by learned cortical mechanisms and conditioned reflexes that inhibit bladder emptying under social controls, and by neurologic coordination of local reflexes that allow the urethra to relax and the bladder to contract when we voluntarily void. Similar mechanisms govern defecation, requiring the same cortical and locally reflexive learned behaviors.22,23
Rectal continence. The sphincter mechanism of the anal canal consists of 2 separate anatomic structures: the internal and external sphincters.
The internal sphincter is involuntary smooth muscle in the rectal wall. It provides continuous involuntary tone. The external sphincter is composed of a triple-loop system. The top loop is the puborectalis portion of the levator ani muscle. It encircles the rectal neck, suspends the anal canal forward toward the symphysis pubis at a near right angle, and maintains continence by closing the rectal inlet. The intermediate loop of the external sphincter pulls in the opposite direction. It originates at the coccyx as a tendon, encircles the middle segment of the anal canal, and inserts back on the coccyx. The base loop is the smallest and lies beneath the anal mucosa, encircling the anus. It is most commonly referred to as the anal sphincter.
The levator plate is attached to the posterior rectum by the hiatal ligament, an extension of the endopelvic fascia. The hiatal ligament, by contraction or relaxation of the levator plate, provides the mechanism by which the rectal inlet is opened and closed. During defecation, the puborectalis contracts and the levator plate relaxes to open the rectal neck.23
FIGURE 5 Perineal membrane and urethra
When the anatomy of the pelvis is intact, the proximal urethra and bladder base are held above the perineal membrane. This intra-abdominal position (at or above the perineal membrane) keeps the urethra within the continence zone.
Reprinted with permission from American College of Obstetricians and Gynecologists. Precis: Gynecology, Second Edition. Washington, DC, ©ACOG, 2001.
Conclusion
Over the past 25 years, new ways of looking at the anatomy and physiology of pelvic-support defects have evolved, demonstrating the need for changes in diagnostic and therapeutic techniques. Specific physical-examination and technical tests allow clinicians to identify abnormalities of both form and function of the pelvic organs. Once identified, pelvic-support defects can be studied more closely, and treatment methods can be developed. Now that there is a subspecialty in pelvic reconstructive surgery, greater emphasis should be placed on female pelvic anatomy and physiology.1-5,11-14,20,24-26
Dr. Julian reports no affiliation or financial arrangement with any of the companies that manufacture drugs or devices in any of the product classes mentioned in this article.