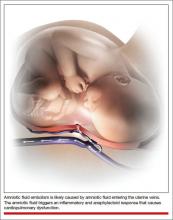
Amniotic fluid embolism (AFE) occurs in about 1 in 20,000 to 1 in 40,000 deliveries.1,2 Although the condition is rare, the case fatality rate is high, and AFE is a common cause of maternal death in developed countries. AFE cannot be predicted or prevented. Moreover, the condition is difficult to precisely define and is often a diagnosis of exclusion.
AFE should be considered in the differential diagnosis of a pregnant woman with sudden onset of shortness of breath, hypotension, or cardiac arrhythmia or arrest, followed by coagulopathy and hemorrhage. Premonitory symptoms, including restlessness, confusion, disorientation, agitation, chills, nausea, numbness, and tingling, are commonly reported just before the cardiorespiratory collapse. AFE is less likely if the initial obstetric event is hemorrhage in the absence of cardiorespiratory compromise or a preceding coagulopathy.3
Typically, the onset is just before birth, during birth, or within the first few hours after delivery. In the United Kingdom, which has a robust centralized registry for reporting AFE, about 56% of cases occur before birth and 44% after birth.4
Related article: Is the incidence of amniotic fluid embolism rising? John T. Repke, MD (Examining the Evidence, August 2010)
The resources available to obstetric units vary greatly. Each unit needs to assess its resources and develop an AFE treatment protocol that builds on the unique strengths of the unit. Treatment of AFE requires the coordinated actions of anesthesiologists, obstetricians, nurses, the blood bank, pharmacy, and cardiovascular specialists. Coordinated activity among the members of such a large multidisciplinary team requires a written protocol that is practiced on a regular basis.
Six important components of a multidisciplinary response to AFE treatment protocol are:
- high-quality cardiopulmonary resuscitation (CPR)
- a protocol for massive transfusion
- treatment of diffuse bleeding and coagulopathy
- treatment of uterine and pelvic bleeding
- extracorporeal lung and heart support
- post-AFE intensive care.
1. Initiate high-quality CPR
Hypotension and hypoxemia due to cardiac and pulmonary dysfunction are prominent features of AFE. Dysrythmias such as pulseless electrical activity, bradycardia, ventricular fibrillation, and asystole are common. Rapid institution of high-quality CPR is critical to the survival of women with AFE.
Interventions often used in CPR of patients with AFE include initiation of high-quality chest compressions, early defibrillation if indicated, immediate administration of 100% oxygen by mask ventilation followed by early intubation, and rapid establishment of peripheral, arterial, and central venous access. Volume assessment, fluid replacement, and administration of vasopressors and inotropes are also important.
CPR of pregnant women requires special interventions, including maximal left lateral displacement of the uterus to reduce compression of the descending aorta and vena cava. Lateral displacement of the uterus can be accomplished by left lateral tilt or by manual uterine displacement. To optimize the effectiveness of chest compressions, many experts recommend placing the woman in a supine position and using manual uterine displacement rather than a left lateral tilt.5 For chest compressions, the hands should be placed just above the center of the sternum to adjust for the elevation of the diaphragm caused by the gravid uterus.
The gravid uterus can compromise the effectiveness of CPR. Fetal viability and neurologic outcome are best if delivery occurs within 5 minutes of the onset of cardiopulmonary arrest. If the gestational age of the fetus is consistent with extrauterine viability and initial CPR has not restored cardiac function, it is best to initiate fetal delivery within 4 minutes of the onset of cardiopulmonary arrest with the intent to deliver the fetus within 5 minutes.6,7 If the fetus is beyond 20 weeks’ gestational age, delivery early in the course of CPR improves the effectiveness of maternal resuscitation and may increase the probability of maternal survival.
In one study of the response of anesthesiologists, obstetricians, and nurses to a simulated cardiac arrest caused by an AFE, the participants did not routinely use defibrillation when indicated, did not place a firm support under the back for chest compressions, and did not switch the provider of chest compressions every 2 minutes.8 This study indicates that additional training and routinely scheduled multidisciplinary simulation of the response to cardiopulmonary arrest could improve the quality of our CPR.
2. Use a massive transfusion protocol
Severe coagulopathy and diffuse bleeding are commonly encountered in AFE. Target goals for the replacement of blood products include:
- hemoglobin concentration ≥8 g/dL
- fibrinogen ≥150 to 200 mg/dL
- platelets ≥50,000/μL
- prothrombin time international normalized ratio (INR) ≤1.5.
Most massive transfusion protocols provide for the rapid delivery of 4 to 8 units of red blood cells and a similar number of units of fresh frozen plasma to the patient’s bedside. In the management of AFE, 20 to 30 units of red blood cells and a similar quantity of fresh frozen plasma may need to be transfused. Cryoprecipitate takes 20 to 30 minutes to thaw, so preparations to transfuse cryoprecipitate should be initiated as soon as the massive transfusion protocol is triggered. A case of AFE can completely empty the blood bank of all available blood products and necessitate the use of alternative agents.